
Influence of Sandblasting on Surface Roughness and Shear Bond Strength of Silicone Soft Liner Applied to 3D Printed Acrylic Denture Bases Material
Mohammed Taqi Sohail Wadi* and Bayan Saleem KhalafPublished Date : October 10, 2025
DOI : https://doi.org/10.12982/NLSC.2026.009
Journal Issues : Number 1, January-March 2026
Abstract Removable dental prostheses remain a reliable treatment for edentulous patients. Conventional fabrication requires multiple steps, whereas computer-aided design and manufacturing (CAD-CAM), particularly 3D printing, offers faster and more cost-effective alternatives.
This in vitro study aimed to evaluate the effect of sandblasting on surface roughness and shear bond strength of silicone soft liner bonded to 3D-printed and heat-cured acrylic denture base materials.
Eighty specimens were divided into four groups: heat-cured control, 3D-printed control, heat-cured sandblasted, and 3D-printed sandblasted. Surface roughness was measured using a profilometer, while shear bond strength was tested with a universal testing machine. Data were analyzed with one-way ANOVA and Games-Howell post hoc test.
Sandblasting significantly increased both surface roughness and shear bond strength compared to untreated groups. The 3D-printed specimens showed higher roughness values after sandblasting than heat-cured ones.
Sandblasting improves surface roughness and bonding performance of both heat-cured and 3D-printed denture base resins, supporting its use as an effective surface treatment in prosthodontics.
Keywords: Acrylic roughness test, Shear bond strength, Heat cure acrylic denture soft liner, Sandblasting, 3D printing.
Graphical Abstract:
Citation: Sohail Wadi, M.T. and Khalaf, B.S. 2026. Influence of sandblasting on surface roughness and shear bond strength of silicone soft liner applied to 3D printed acrylic denture bases material. Natural and Life Sciences Communications. 25(1): e2026009.
INTRODUCTION
Removable dental prostheses (RPDs) are the preferred option for patients missing teeth who are unable to get implant therapy due to anatomical, psychological, or economic constraints (Abduo, 2013). Conventional full-mouth dentures for older patients Missing teeth are a complex and time-consuming process requiring multiple clinical and laboratory appointments (Saponaro et al., 2016). The advent of contemporary technology 3D printers is being used in additive manufacturing for many reasons, such as production, health care, research, and education. In prosthetic dentistry, additive manufacturing's ability to manipulate material using CAD data affects prosthesis quality, mechanical properties, cost, and production time. Also, due to the capacity for data storage, the process of remanufacturing dentures can be facilitated (Fareed Al-Sammraaie and A Fatalla, 2023; Ali and Taha, 2024).
3D printing technology, especially the additive technique, has grown preferred in dental applications due to its superior printing resolution, rapid production rate, and cost economy if compared to traditional heat-cured resins (Tzeng et al., 2021). It is cost-effective as it avoids the use of rotary tools, decreases the loss of raw materials, and enables the simultaneous production of several goods (Gad et al., 2022).
The most common use Technologies for additive manufacturing include stereolithography apparatuses (SLA) that use laser light for incremental polymerization and digital light processing (DLP), which uses a projector for polymerization (Lee, 2016; Alharbi et al., 2017).
Removable prostheses may give rise to less adaptability with alveolar ridge over time one should consider relining, rebasing, or refabricating to solve these issues. Relining is the most widely used of these three techniques and is frequently considered the best choice for moderate to minor ridge resorption (Tallgren, 1972; Hatamleh et al., 2010).
Resilient denture lining materials are applied to improve retention, evenly dissipate load, and minimize concentrated stress by producing a cushioning effect below the denture base material, thereby inhibiting more resorption (Alabady and Khalaf, 2023). Denture liners are categorized into two types: hard and resilient. Resilient liners are also divided into short- and long-term liners. Short-term liners are made for a 30-day duration, while long-term denture liners preserve their resiliency for more than 30 days and may be worn for up to 1 year (Abdul-Baqi et al., 2022; Adwar et al., 2024; Talib and Taha, 2024).
Denture-resilient liner materials have drawbacks, including color instability, loss of resiliency, inadequate hardness, surface defects, porosity, water absorption, microbial accumulation, and the most serious issues is debonding with denture base material (Hamedirad et al., 2021). Providing a strong and lasting binding between denture liners and acrylic resins is necessary to avoid separation at the denture borders for optimal denture function (Alkinani, 2014; Abdul-Baqi et al., 2022).
A shear load is a force that forces a material to slide in a plane parallel to the direction of the force (Panda et al., 2021). Shear stress weakens the binding between the denture base and resilient liner, causing bond failure. This failure allows oral fluids to enter the interface, causing the reline material to detach from the denture base (Rajaganesh et al., 2016; Taha et al., 2024).
The purpose of this study is to compare a 3D-printed denture base to a standard PMMA resin that has been surface treated with sandblasting in terms of surface roughness and soft-liner shear bond strength.
Hypothesis: The null hypothesis indicated that 3D and PMMA acrylic denture bases had the same surface roughness and shear bond strength.
MATERIALS AND METHODS
Materials
A total of 80 specimens were prepared and divided to 40 specimens for the roughness and shear bond tests for both materials. The specimens groups:
1. 1st control group (HCC): comprised of heat cured acrylic specimens that were not subjected to any surface treatment.
2. 2nd control group (3DC): comprised of 3D printed acrylic specimens that were not subjected to any surface treatment.
3. 1st test group (HCS): heat-cured acrylic specimens that were treated with a100µm particle size sand blast.
4. 2nd test group (3DS): 3D printed acrylic specimens that were treated with a 100µm particle size sand blast.
This study was conducted as an in vitro experiment to evaluate controlled conditions of bonding and surface characteristics.
Sample size calculation
An a priori power analysis was performed in GPower (version 3.1) for a one-way ANOVA (fixed effects, omnibus) with 4 independent groups (HCC, 3DC, HCS, 3DS). Assuming a large effect size of f = 0.50 (≈ partial η2 ≈ 0.20), α = 0.05, and power (1–β) = 0.80, the required total sample size was 40 (i.e., n = 10 per group). GPower output: critical F ≈ 2.84 (df1 = 3, df2 = 36), noncentrality parameter λ = 10.00, actual power ≈ 0.803.
The same allocation was applied per outcome (surface roughness and shear bond strength), yielding 40 specimens per test and 80 specimens in total.
The PD (procryla) heat-cured acrylic material was used to fabricate the heat-cured specimens According to manufacturing instructions. The three-dimensional acrylic specimens were created by using a Creality Halot one plus 4k LCD MSLA 3D printer (Creality, China) with a Detax denture base resin (Detax, Germany). The specimens were constructed with a layer thickness of fifty microns, and the exposure duration was taken for four seconds.
Following the manufacturer's instructions, after removing the specimens from the build plate, they were immersed in a 99% isopropyl alcohol (IPA) solution for 10 minutes. After that, the specimens were dried using 1.5 psi compressed air to eliminate contaminated IPA. The last step was to put the specimens in a UV light polymerization device for 15 minutes while submerged in glycerin.
The preparation of the specimens was finished by sandpaper with a grit size of 600 while being subjected to a flow of water. The manual procedure was performed for 50 seconds, for a distance of 10 cm in a linear direction on a flat surface, the motion and number of abrading strokes were unified across all specimens to prevent surface irregularities (Zeid Abood, 2016). The abraded specimens were subsequently subjected to a cleaning process involving the use of an ultrasonic cleaning device filled with distilled water and subjected to vibration for a duration of 20 minutes (Mustafa and Hamad, 2015).
The acrylic specimens of roughness and shear bond strength shown in figure 1. The shear bond specimen was composed of two acrylic blocks positioned in a stacked configuration, resulting in a space with measurements of 25 mm in length, 25 mm in width, and 3 mm in depth. The acrylic blocks were invested using silicone putty impression material (Zeid Abood, 2016). The specimens in a silicone mold were completely immersed in a custom-made flask measuring 8 by 16 by 12 cm and filled with newly mixed dental stone.
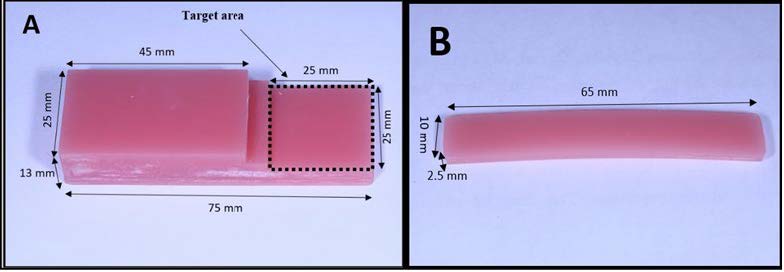
Figure 1. Acrylic specimens: A- shear, B- roughness.
After the specimens removed from flasks, the heat-cured and 3D-printed acrylic specimens were subjected to the impact of aluminum oxide sand blast particles. The particles of sandblast, measuring 100 µm in size, were directed towards the surface of the specimens using a pressure of 2.8 bars for a duration of 10 seconds. The particles were delivered in a circular motion, originating from a distance of 10 mm from the specimens (Yaseen Hasan and Moudhaffar Ali, 2018; Al Taweel et al., 2021). Following the sandblasting process, the specimens were immerse in an ultrasonic cleaner containing distilled water for a duration of 10 minutes (Nakhaei et al., 2016).
The gap between the bonded surfaces of the shear bond specimens were filled using Detax silicone soft liner figure 2. Process for the soft liner was carried out in accordance with the manufacturer's instructions.
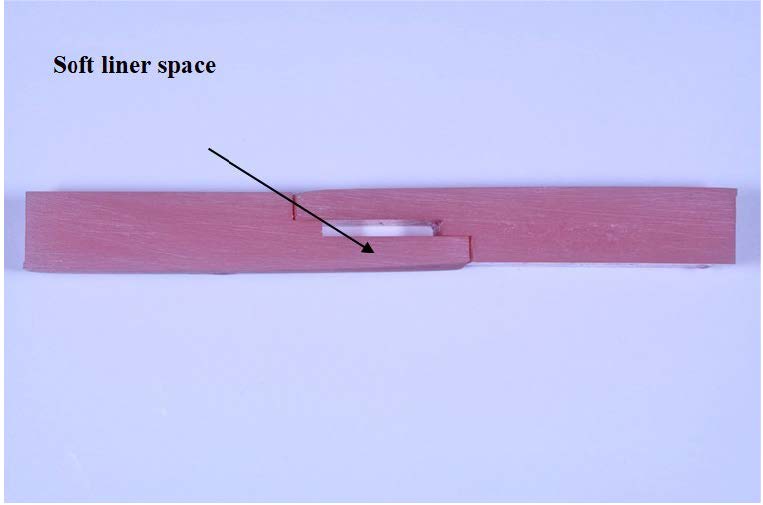
Figure 2. Shear bond strength acrylic specimen.
The measurement of surface roughness test was conducted using a profilometer model TR220 (China). Three measurements was taken, the stylus of the device made contact with the surface of the specimen at three distinct locations. The calculated mean of the three recorded measurements was obtained and subsequently denoted as the roughness value (Nakhaei et al., 2016).
The surface morphology of specimens was examined using a Scanning Electron Microscope (model Inspect S50, FEI. Japan) at 250× magnification. Representative images were captured to evaluate surface topography.
The shear bond strength test was performed with the assistance of an Instron testing machine (Laryee.china), with a load cell capacity of one hundred kilograms and a cross-head speed of half a millimeter per minute, as described by (Wang et al., 1996). The separation force was computed, and the shear bonding strength of each specimen was evaluated using the provided equation.
Shear Bond strength=F (N)/A (mm2).
* F represents the maximum failure force in Newtons.
* A represents the specimen's cross-sectional area in square millimeters (mm2).
The mode of failure in bonded region was conducted using a stereomicroscope set at a magnification level of 10 times. According to Ariff et al. (2025) cohesive, adhesive, or mixed failure was the classification system used. If the amount of reline material on the acrylic surface was more than 50%, it was considered a cohesive failure. The lack of reline material on the acrylic surface, in contrast, was indicative of adhesive failure. When the amount of reline material on the acrylic surface was less than 50%, it was considered a mixed failure.
Statistical analysis
Data were analyzed using one-way ANOVA followed by Games-Howell post hoc test to identify differences between groups. The level of statistical significance was set at P<0.05. Statistical analysis was performed using SPSS software (version 26, USA).
RESULTS
The SEM pictures of both the material for untreated and sand-blasted groups are shown in (Figure 3) The image of the untreated heat cure and 3D printed denture base material surfaces demonstrates an array of parallel scratches that are uniformly distributed and result from the finishing process of sand paper abrasion, while the sand-blasted specimen surfaces for both materials developed prominent irregularities as well as lots of small pits, cavities, and depressions. The 3D sand-blasted group exhibited broader and deeper cavities compared to sand-blasted heat-cured.
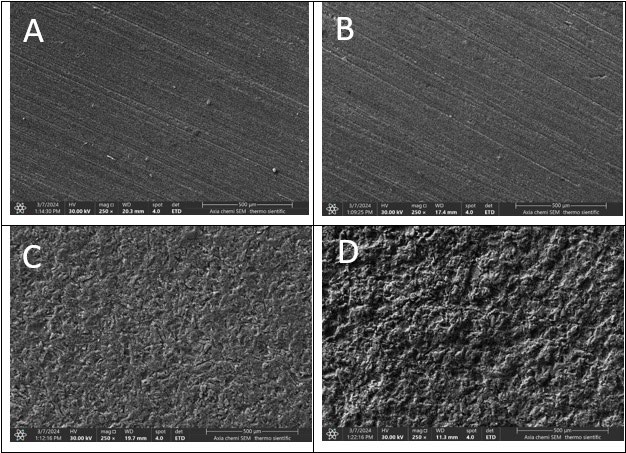
Figure 3. Scanning electron microscope at magnification 250x: A) HCC = heat-cured control, B) 3DC = 3D-printed control, C) HCS = heat-cured sandblasted, D) 3DS = 3D-printed sandblasted.
A one-way ANOVA test was run, and the results showed that the groups differed significantly (P = 0.0001). Figures 4 and 5, respectively, provide the descriptive statistics for the roughness test and shear bond strength test for each group.
The roughness test result show that sand blast groups have higher significantly (P<0.001) roughness mean than control groups for both materials.
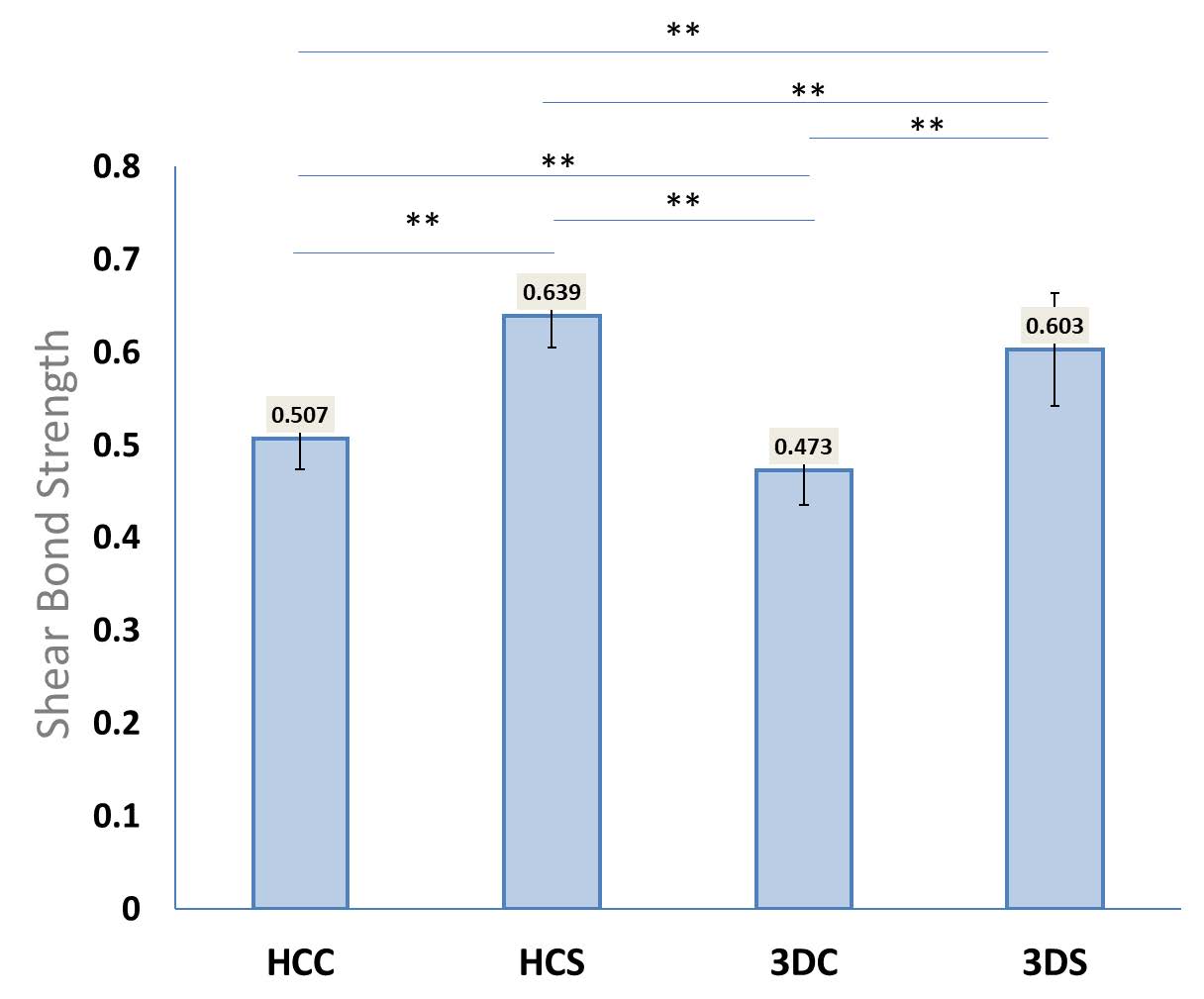
Figure 4. displays the average and standard deviation values of shear bond strength for each group as evaluated by the universal testing equipment.
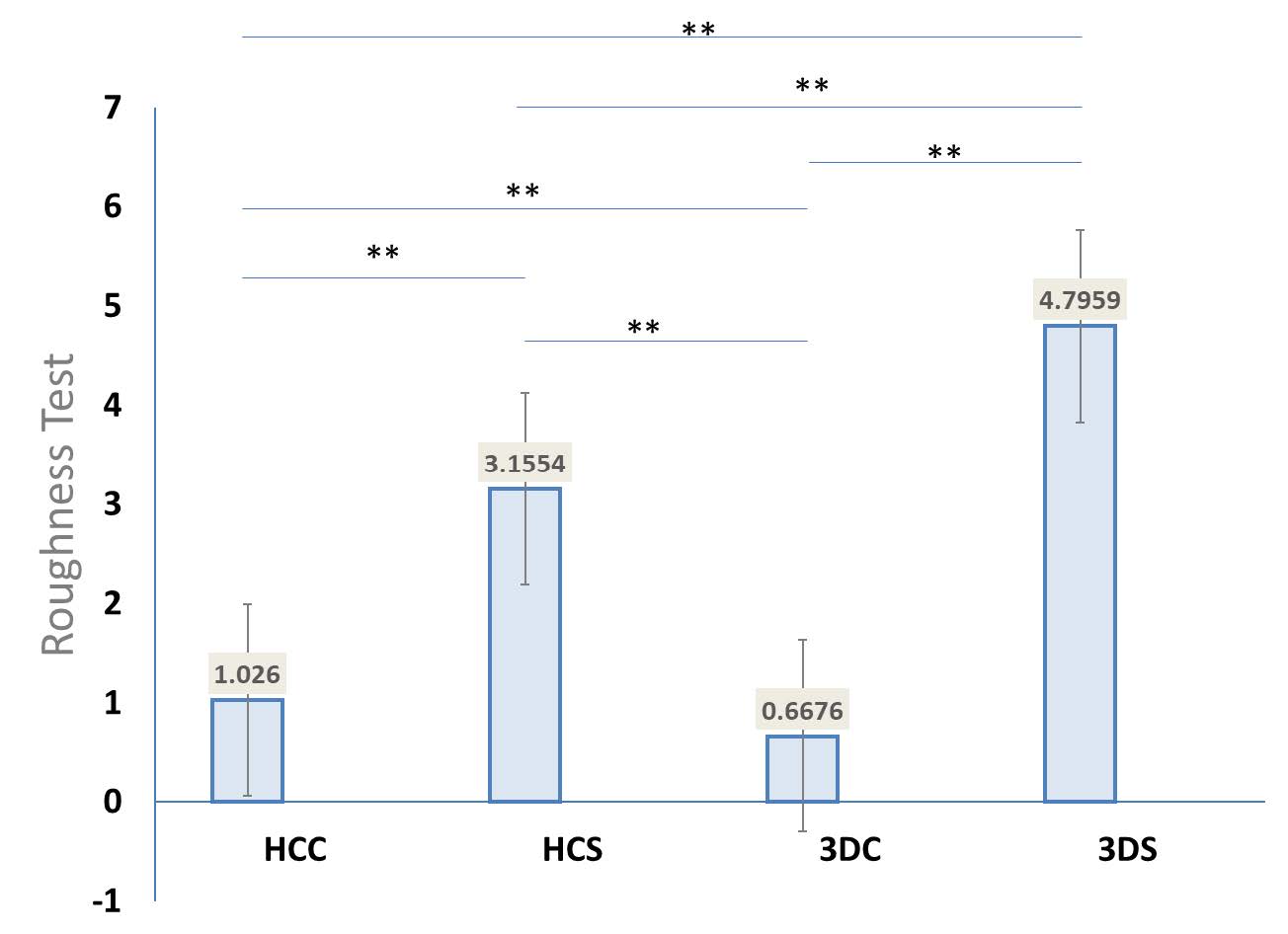
Figure 5. exhibits the average and standard deviation of roughness test results for each group obtained from the profilometer machine.
The result demonstrate that sandblast groups show higher mean shear bond strength than control groups for both material.
According to the results of the Games-Howell test for shear bond strength and roughness, the differences between each group are shown in Table 1.
Table 1. Games-Howell post-hoc test.
|
Test |
Shear bond strength |
Roughness test |
|||||||
|
Statistics |
Mean difference |
SD |
P-value |
Mean difference |
SD |
P-value |
|
||
|
Heat Cure Control vs. Heat Sand |
–0.1324 |
0.0151 |
0.0000* |
–2.1294 |
0.0792 |
0.000* |
|
||
|
Heat Cure Control vs. 3D Control |
0.0341 |
0.0161 |
0.1880 |
0.3584 |
0.0379 |
0.000* |
|
||
|
Heat Cure Control vs. 3D Sand |
–0.0965 |
0.0220 |
0.0030* |
–3.7699 |
0.0806 |
0.000* |
|
||
|
Heat Sand vs. 3D Control |
0.1665 |
0.0164 |
0.0000* |
2.4878 |
0.0719 |
0.000* |
|
||
|
Heat Sand vs. 3D Sand |
0.0359 |
0.0222 |
0.4000 |
–1.6405 |
0.1011 |
0.000* |
|
||
|
3D Control vs. 3D Sand |
–0.1306 |
0.0229 |
0.0000* |
–4.1283 |
0.0733 |
0.000* |
|
||
|
Note: * The mean difference is significant at the 0.05 level.
|
|||||||||
The cohesive, adhesive and mixed percentage are presented in Figure 6.
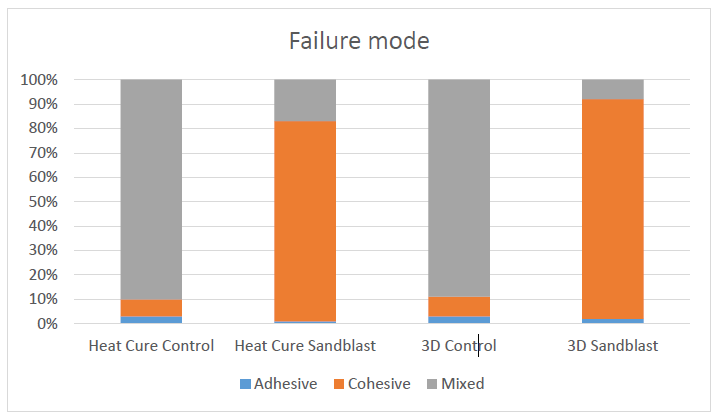
Figure 6. The cohesive, adhesive and mixed percentage.
DISCUSSION
The long-term functional success and survival of a denture liner is dependent on forming a strong and durable bond to the underlying denture base (Imirzalioglu et al., 2010).
Many Factors that impact the bond strength of denture liners are: force direction, type of denture base, adhesive agent properties, liner manufacture method, and denture liner thickness (Demir et al., 2011).
In the present study, two materials of denture base and soft liners were used. Changing the denture base and lining material chemical composition cannot be achieved since it is an inherent property of the material, therefore the bonding quality was improved by sandblasting of the printed denture base using (100 µm) aluminum oxide airborne abrasive. This treatment showed increase in the shear bonding strength of the silicone based soft liner to the conventional and printed denture base.
Surface roughness plays a pivotal role in the bonding between soft liner and acrylic denture base, with a larger surface area promoting superior adhesion.
The study observed a substantial roughness increase in the treated groups compared to the control, a finding consistent with the outcomes reported by Hamedirad et al. (2021) on heat cure acrylic and Shaaban et al. (2023) on 3D printed acrylic following sandblasting with 125 µm aluminum oxide.
The research findings revealed that the 3D control group exhibited significantly lower roughness than the control group of heat-cured acrylic, corroborating the findings of Fiore et al. (2022) and Falahchai et al. (2023). The reduced surface roughness in 3D-printed resin may be attributed to a layer thickness of approximately 50 µm per layer, as noted in the study by Gad et al. (2022). Moreover, the printing orientation, as highlighted by Shim et al. (2020), also influences 3D surface roughness.
The 3D printed less hardness than heat cured acrylic this might be associated to the level of residual monomers as residual monomer content was found to adversely affect the surface hardness (Al‐Dwairi et al., 2023). A notable difference emerged between the two sandblast groups, show that 3D printed acrylic exhibited significantly higher roughness than the heat-cured counterpart. This discrepancy can be attributed to variations in composition and manufacturing processes. Distinct molecular structures or surface characteristics may influence responses to sandblasting due to factors such as polymerization methods, polymer chain arrangement, and post curing process (AlZaher et al., 2020; Gad et al., 2022).
Aluminum oxide particles create favorable irregularities, including pits and fissures, as shown previously by SEM analysis, which contributes to improving the mechanical bonding of adhesive materials.
Shear bond strength test findings indicate a difference between the sandblasted groups and control groups for both materials. Conversely, no differences were observed between the heat-cured and 3D materials in both the control and sandblast groups. Notably, sandblast treatment resulted in a notable increase in shear bond strength for both materials.
The enhancement in shear bond strength due to sandblast treatment can be attributed to the alumina-blasting treatment, which increased shear bond strength when applied to either the base or tooth surfaces, or both. This increase result from the abrasion effect achieved by aluminum oxide particles impacting the surface, thereby increasing its total surface energy and creating irregularities and undercuts. These micromechanical retention pits contribute to enhanced bond strength. Additionally, alumina-blasting augments bond strength by increasing the total bonding area, leading to an improvement in shear bond strength (Chung et al., 2008; AlZaher et al., 2020).
Koseoglu et al. (2023) revealed that the increase in the bond strength is usually associated with a change in the mode of failure. In this study show that significantly observed between control (mixed failure) and sand blasted specimens (cohesive failure) for both material.
Mert et al. (2023) suggested, in their research, that relined 3D-printed specimens exhibited significantly lower shear bond strength compared to conventional and milled groups. No distinctions in shear bond strengths were identified between the milled and conventional groups. However, it is crucial to acknowledge a limitation in Mert's study: no specific pre-treatment or bonding procedures were applied to the 3D-resin group samples. This lack of treatment might have influenced the shear bond strength of these samples due to the differing chemical composition from CAD-CAM milled PMMA and conventional PMMA.
Study by Park and Lee (2022) found that displaying adhesive failure and resulting in low shear bond strength. It is postulated that a significant amount of material detached when denture lining material was used without additional surface treatment on 3D-printed dentures.
Recent studies have investigated strategies to improve the bond strength of soft liners and relines to denture bases, particularly in 3D‑printed materials. Pereira et al. (2025) demonstrated that 50 µm alumina air abrasion can make the bond strength of 3D‑printed bases comparable to heat‑polymerized ones, while a 180‑second monomer immersion produced the highest bond strength and enhanced resistance to aging after 10,000 cycles. Complementing these findings, Sturzenegger et al. (2025) emphasized that multi-step pretreatment—combining air abrasion with chemical conditioning—optimizes reline bonding in printed dentures. Similarly, Tugut et al. (2024) reported that bond strength varies depending on the denture base material and aging conditions, with conventional, milled, and printed bases showing frequent adhesive failures when no pretreatment is applied. Collectively, these studies highlight that surface conditioning and chemical treatment are crucial for achieving durable bonds, particularly in 3D‑printed denture bases.
Limitation
A limitation of this research is that the tests were done without thermocycling and cyclic load on specimens, and the number of specimens used was limited. Another limitation is that the studies did not mimic the oral environment, which includes saliva and masticatory forces that affect bond strength. Therefore, more clinical evaluation is necessary.
CONCLUSION
The sandblast treatment was shown to be efficient at enhancing roughness, with more of an effect noticed in 3D-printed acrylic as compared to heat-cured acrylic. Also, sandblasting significantly improves the shear bond strength of both materials, with no noticeable variation in bond strength between the two materials.
ACKNOWLEDGEMENTS
The authors thank the College of Dentistry, University of Baghdad for providing instruments.
AUTHOR CONTRIBUTIONS
Mohammed Taqi assisted in conducting the experiments, performed the statistical analysis and data visualization and wrote the manuscript. Bayan Saleem designed and conducted all of the experiments and wrote the manuscript. All authors have read and approved of the final manuscript.
CONFLICT OF INTEREST
The authors declare that they hold no competing interests.
REFERENCES
Abdul-Baqi, H.J., Safi, I.N., Nima Ahmad, A., and Fatalla, A.A. 2022. Investigating tensile bonding and other properties of yttrium oxide nanoparticles impregnated heat-cured soft-denture lining composite in vitro. Journal of International Society of Preventive and Community Dentistry. 12(1): 93–99. https://doi.org/10.4103/jispcd.JISPCD_274_21
Abduo, J. 2013. Occlusal schemes for complete dentures: A systematic review. The International Journal of Prosthodontics. 26(1): 26–33. https://doi.org/10.11607/ijp.3168
Adwar, H.S., Ahmed, S.A., and Hamad, F.H. 2025. Association of oral manifestations with iron deficiency anemia: A case-control study. Natural and Life Sciences Communications. 24(1): e2025006. https://doi.org/10.12982/NLSC.2025.006
Al Taweel, S.M., Al-Otaibi, H.N., Labban, N., AlFouzan, A., and Shehri, H.Al. 2021. Soft denture liner adhesion to conventional and CAD/CAM processed poly(methyl methacrylate) acrylic denture resins-an in-vitro study. Materials. 14(21): 6614. https://doi.org/10.3390/ma14216614
Alabady, A.A. and Khalaf, B.S. 2023. Effect of Nd: YAG laser surface treatment on wettability of thermoplastic acrylic in comparison with heat-cure acrylic resin. Al-Bayan Journal for Medical and Health Sciences. 2(1): 9–17.
Al‐Dwairi, Z.N., Al Haj Ebrahim, A.A., and Baba, N. 2023. A comparison of the surface and mechanical properties of 3D printable denture‐base resin material and conventional polymethylmethacrylate (PMMA). Journal of Prosthodontics. 32(1): 40–48. https://doi.org/10.1111/jopr.13491
Alharbi, N., Wismeijer, D., and Osman, R. 2017. Additive manufacturing techniques in prosthodontics: Where do we currently stand? a critical review. The International Journal of Prosthodontics. 30(5): 474–484. https://doi.org/10.11607/ijp.5079
Ali, M.F. and Taha, G.I. 2024. Gingival crevicular fluid volume and protein concentration: A biomarker tool for predicting periodontal diseases progression and severity. Natural and Life Sciences Communications. 23(4): e2024055. https://doi.org/10.12982/NLSC.2024.055
Alkinani, G.A. 2014. Evaluation of shear bond strength between thermosens as relining material and different denture base materials. Journal of Baghdad College of Dentistry. 26(4): 28–31. https://doi.org/10.12816/0015251
AlZaher, Z.A., Almaskin, D.F., Qaw, M.S., Abu Showmi, T.H., Abualsaud, R., Akhtar, S., and Gad, M.M. 2020. Chemo-mechanical approach to improve repair bond strength of denture teeth. International Journal of Dentistry. 2020: 1–8. https://doi.org/10.1155/2020/8870361
Ariff, I.M., Wong, K.J., Gan, K.W., Israr, H.A., and Tamin, M.N. 2025. Progressive damage analyses of patch repaired composites using acoustic emission and digital image correlation. International Journal of Adhesion and Adhesives. 104111. https://doi.org/10.1016/j.ijadhadh.2025.104111
Chung, K.‐H., Chung, C.Y., Chung, C.Y., and Chan, D.C.N. 2008. Effect of pre‐processing surface treatments of acrylic teeth on bonding to the denture base. Journal of Oral Rehabilitation. 35(4): 268–275. https://doi.org/10.1111/j.1365-2842.2007.01779.x
Demir, H., Dogan, A., Dogan, O.M., Keskin, S., Bolayir, G., and Soygun, K. 2011. Peel bond strength of two silicone soft liners to a heat-cured denture base resin. Journal of Adhesive Dentistry. 13(6): 537. https://doi.org/10.3290/j.jad.a19813
Falahchai, M., Ghavami-Lahiji, M., Rasaie, V., Amin, M., and Neshandar Asli, H. 2023. Comparison of mechanical properties, surface roughness, and color stability of 3D-printed and conventional heat-polymerizing denture base materials. The Journal of Prosthetic Dentistry. 130(2): 266.e1-266.e8. https://doi.org/10.1016/j.prosdent.2023.06.006
Fareed Al-Sammraaie, M. and A Fatalla, A. 2023. The effect of ZrO2 NPs addition on denture adaptation and diametral compressive strength of 3D printed denture base resin. Nanomedicine Research Journal. 8(4): 345–355. https://doi.org/10.22034/nmrj.2023.04.003
Fiore, A.D., Meneghello, R., Brun, P., Rosso, S., Gattazzo, A., Stellini, E., and Yilmaz, B. 2022. Comparison of the flexural and surface properties of milled, 3D-printed, and heat polymerized PMMA resins for denture bases: An in vitro study. Journal of Prosthodontic Research. 66(3): JPR_D_21_00116. https://doi.org/10.2186/jpr.JPR_D_21_00116
Gad, M.M., Fouda, S.M., Abualsaud, R., Alshahrani, F.A., Al‐Thobity, A.M., Khan, S.Q., Akhtar, S., Ateeq, I.S., Helal, M.A., and Al‐Harbi, F.A. 2022. Strength and surface properties of a 3D‐printed denture base polymer. Journal of Prosthodontics. 31(5): 412–418. https://doi.org/10.1111/jopr.13413
Hamedirad, F., Alikhasi, M., and Hasanzade, M. 2021. The effect of sandblasting on bond strength of soft liners to denture base resins: A systematic review and meta-analysis of in vitro studies. International Journal of Dentistry. 2021: 1–17. https://doi.org/10.1155/2021/5674155
Hatamleh, M.M., Maryan, C.J., Silikas, N., and Watts, D.C. 2010. Effect of net fiber reinforcement surface treatment on soft denture liner retention and longevity. Journal of Prosthodontics. 19(4): 258–262. https://doi.org/10.1111/j.1532-849X.2009.00566.x
Imirzalioglu, P., Karacaer, O., Yilmaz, B., and Ozmen, I. 2010. Color stability of denture acrylic resins and a soft lining material against tea, coffee, and nicotine. Journal of Prosthodontics. 19(2): 118–124. https://doi.org/10.1111/j.1532-849X.2009.00535.x
Koseoglu, M., Tugut, F., and Akin, H. 2023. Tensile bond strength of soft and hard relining materials to conventional and additively manufactured denture‐base materials. Journal of Prosthodontics. 32(S1): 74–80. https://doi.org/10.1111/jopr.13608
Lee, S. 2016. Prospect for 3D printing technology in medical, dental, and pediatric dental field. The Journal of the Korean Academy of Pedtatric Dentistry. 43(1): 93–108. https://doi.org/10.5933/JKAPD.2016.43.1.93
Mert, D., Kamnoedboon, P., Al-Haj Husain, N., Özcan, M., and Srinivasan, M. 2023. CAD-CAM complete denture resins: Effect of relining on the shear bond strength. Journal of Dentistry. 131: 104438. https://doi.org/10.1016/j.jdent.2023.104438
Mustafa, S.B. and Hamad, T.I. 2015. The effect of plasma treatment on shear bond strength of high impact acrylic resin denture base lined with two types of soft lining materials after immersion in distilled water and denture cleanser. Journal of Baghdad College of Dentistry. 27(4): 44–51. https://doi.org/10.12816/0024063
Nakhaei, M., Dashti, H., Ahrari, F., Vasigh, S., Mushtaq, S., and Shetty, R.M. 2016. Effect of different surface treatments and thermocycling on bond strength of a silicone-based denture liner to a denture base resin. Journal of Contemporary Dental Practice. 17(2): 154–159. https://doi.org/10.5005/jp-journals-10024-1819
Panda, S.K., Reddy, N., Manual, L., Krishna, C., Jagadeesh, K.N., Saidath, K., and Babaji, P. 2021. An in vitro evaluation of tensile bond strength of soft liners bonded to different denture base resins. Annals of African Medicine. 20(2): 116–120. https://doi.org/10.4103/aam.aam_30_20
Park, S.-J. and Lee, J.-S. 2022. Effect of surface treatment on shear bond strength of relining material and 3D-printed denture base. The Journal of Advanced Prosthodontics. 14(4): 262–270. https://doi.org/10.4047/jap.2022.14.4.262
Pereira, A.L., de Souza, B.B., de Miranda, L.M., Curinga, M.R., de Sousa, L.C., de Queiroz, E.É., Barão, V.A., and Carreiro, A.d. 2025. Evaluation of the bond strength, surface roughness and wettability between 3D-printed denture base resin and denture lining material with different surface treatments. Journal of Clinical and Experimental Dentistry. 17: e249–e258. https://doi.org/10.4317/jced.62350
Rajaganesh, N., Sabarinathan, S., Azhagarasan, N., Shankar, C., Krishnakumar, J., and Swathi, S. 2016. Comparative evaluation of shear bond strength of two different chairside soft liners to heat processed acrylic denture base resin: An in vitro study. Journal of Pharmacy and Bioallied Sciences. 8(5): 154. https://doi.org/10.4103/0975-7406.191948
Saponaro, P.C., Yilmaz, B., Heshmati, R.H., and McGlumphy, E.A. 2016. Clinical performance of CAD-CAM-fabricated complete dentures: A cross-sectional study. The Journal of Prosthetic Dentistry. 116(3): 431–435. https://doi.org/10.1016/j.prosdent.2016.03.017
Shaaban, S., Bekheet, S., Abdallah, S., and Mahmoud, T. 2023. Effect of sandblasting surface treatment on the bond strength and surface roughness between the 3D-printed denture base and silicon-based soft liner. Egyptian Dental Journal. 69(3): 2175–2184. https://doi.org/10.21608/edj.2023.208104.2532
Shim, J.S., Kim, J.-E., Jeong, S.H., Choi, Y.J., and Ryu, J.J. 2020. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. The Journal of Prosthetic Dentistry. 124(4): 468–475. https://doi.org/10.1016/j.prosdent.2019.05.034
Sturzenegger, S., Srisanoi, K., Stillhart, A., and Srinivasan, M. 2025. Improving reline bonding in 3D-printed dentures: An experimental in vitro study. Journal of Dentistry. 160: 105873. https://doi.org/10.1016/j.jdent.2025.105873
Taha, G.I., Talib, E.Q., Abed, F.B., and Hasan, I.A. 2024. A review of microbial pathogens and diagnostic techniques in children’s oral health. Sri Lanka Journal of Child Health. 53(4): 355–359. https://doi.org/10.4038/sljch.v53i4.11043
Talib, E.Q. and Taha, G.I. 2024. Involvement of interlukin-17A (IL-17A) gene polymorphism and interlukin-23 (IL-23) level in the development of peri-implantitis. BDJ Open. 10(1): 12. https://doi.org/10.1038/s41405-024-00193-9
Tallgren, A. 1972. The continuing reduction of the residual alveolar ridges in complete denture wearers: A mixed-longitudinal study covering 25 years. The Journal of Prosthetic Dentistry. 27(2): 120–132. https://doi.org/10.1016/0022-3913(72)90188-6
Tugut, F., Koyu, T., and Turkyilmaz, O. 2024. Comparison of bond strength of soft denture liner on denture base materials produced by different methods and effect of thermocycling. Journal of Advanced Oral Research. 15(2): 124–130. https://doi.org/10.1177/23202068241269854
Tzeng, J.-J., Yang, T.-S., Lee, W.-F., Chen, H., and Chang, H.-M. 2021. Mechanical properties and biocompatibility of urethane acrylate-based 3D-printed denture base resin. Polymers. 13(5): 822. https://doi.org/10.3390/polym13050822
Wang, X., Powers, J.M., and Connelly, M.E. 1996. Color stability of heat‐activated and chemically activated fluid resin acrylics. Journal of Prosthodontics. 5(4): 266–269. https://doi.org/10.1111/j.1532-849X.1996.tb00510.x
Yaseen Hasan, W. and Moudhaffar Ali, M. 2018. Evaluation of thermal conductivity and some other properties of heat cured denture soft liner reinforced by halloysite nanotubes. Biomedical and Pharmacology Journal. 11(3): 1491–1500. https://doi.org/10.13005/bpj/1516
Zeid Abood, A. 2016. Measuring the shear bound strength on acrylic resin veneer to metal surface of nickel (a comparative study). Tikrit Journal for Dental Sciences. 4(2): 141–148. https://doi.org/10.25130/tjds.4.2.8
OPEN access freely available online
Natural and Life Sciences Communications
Chiang Mai University, Thailand. https://cmuj.cmu.ac.th
Mohammed Taqi Sohail Wadi* and Bayan Saleem Khalaf
Department of Prosthodontics, College of Dentistry, University of Baghdad, Bab Al-Muadham, Baghdad, 1417, Iraq.
Corresponding author: Mohammed Taqi Sohail Wadi, E-mail: mohammed.taqi2301m@codental.uobaghdad.edu.iq
ORCID iD:
Mohammed Taqi Sohail Wadi: https://orcid.org/0009-0004-5186-3487
Bayan Saleem Khalaf: https://orcid.org/0000-0003-2288-4241
Total Article Views
Editor: Anak Iamaroon,
Chiang Mai University, Thailand
Article history:
Received: June 9, 2025;
Revised: September 21, 2025;
Accepted: October 2, 2025;
Online First: October 10, 2025

