REFERENCES
Aljubran A., Elshenawy, M.A., Kandil, M., Zahir, M.N., Shaheen, A., Gad, A., Alshaer, O., Alzahrani, A., Eldali, A., and Bazarbashi, S. 2019. Efficacy of regorafenib in metastatic colorectal cancer: A multi-institutional retrospective study. Clinical Medicine Insights: Oncology. 13:1179554918825447.
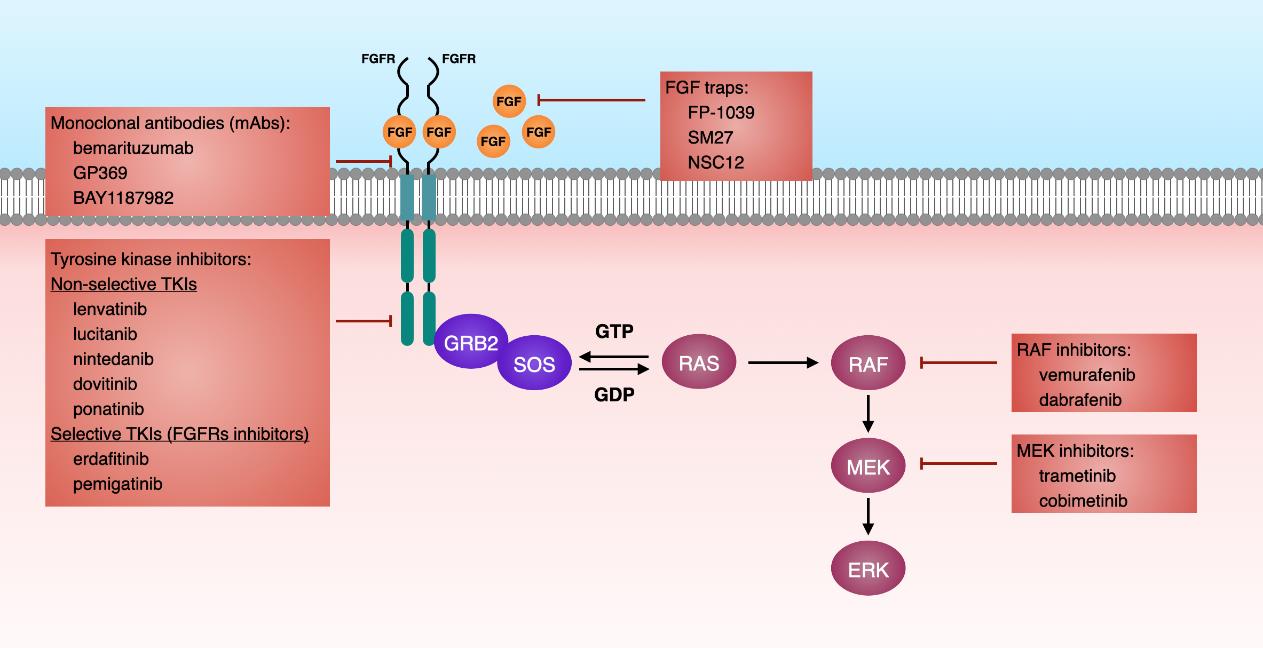
Babina, I.S., Turner, N.C. 2017. Advances and challenges in targeting FGFR signalling in cancer. Nature Reviews Cancer. 17:318-332.
Bartels, S., Adisa, A., Aladelusi, T., Lemound, J., Stucki-Koch, A., Hussein, S., Kreipe, H., Hartmann, C., Lehmannm, U., and Hussein, K. 2018. Molecular defects in braf wild-type ameloblastomas and craniopharyngiomas-differences in mutation profiles in epithelial-derived oropharyngeal neoplasms. Virchows Archiv. 472: 1055-1059.
Bromberg-White, J.L., Andersen, N.J., and Duesbery, N.S. 2012. Mek genomics in development and disease. Briefings in Functional Genomics. 11: 300-310.
Brown, N.A. and Betz, B.L. 2015. Ameloblastoma: A review of recent molecular pathogenetic discoveries. Biomarkers in Cancer. 7s2: BIC.S29329.
Brown, N.A., Rolland, D., McHugh, J.B., Weigelin, H.C., Zhao, L., Lim, M.S., Elenitoba-Johnson, K.S., and Betz, B.L. 2014. Activating fgfr2-ras-braf mutations in ameloblastoma. Clinical Cancer Research. 20: 5517-5526.
Brunet, M., Khalifa, E., and Italiano, A. 2019. Enabling precision medicine for rare head and neck tumors: The example of braf/mek targeting in patients with metastatic ameloblastoma. Frontiers in Oncology. 9:1204.
Burotto, M., Chiou, V.L., Lee, J.M., and Kohn, E.C. 2014. The mapk pathway across different malignancies: A new perspective. Cancer. 120: 3446-3456.
Chae, Y.K., Ranganath, K., Hammerman, P.S., Vaklavas, C., Mohindra, N., Kalyan, A., Matsangou, M., Costa, R., Carneiro, B., Villaflor, V.M., et al. 2017. Inhibition of the fibroblast growth factor receptor (fgfr) pathway: The current landscape and barriers to clinical application. Oncotarget. 8: 16052-16074.
Chang, F., Steelman, L.S., Lee, J.T., Shelton, J.G., Navolanic, P.M., Blalock, W.L., Franklin, R.A., and McCubrey, J.A. 2003. Signal transduction mediated by the ras/raf/mek/erk pathway from cytokine receptors to transcription factors: Potential targeting for therapeutic intervention. Leukemia. 17: 1263-1293.
Davies, H., Bignell, G.R., Cox, C., Stephens, P., Edkins, S., Clegg, S., Teague, J., Woffendin, H., Garnett, M.J., Bottomley, W., et al. 2002. Mutations of the braf gene in human cancer. Nature. 417: 949-954.
Davis, J. and Wayman, M. 2022. Encorafenib and binimetinib combination therapy in metastatic melanoma. Journal of the Advanced Practitioner in Oncology. 13: 450-455.
Daws, S., Chaiyasate, K., and Lehal, A. 2021. Treatment of a braf v600e positive ameloblastoma in a pediatric patient with mek inhibitor monotherapy. FACE. 2: 179-182.
Degirmenci, U., Wang, M., and Hu, J. 2020. Targeting aberrant ras/raf/mek/erk signaling for cancer therapy. Cells. 9: 198.
Derakhshan, S., Aminishakib, P., Karimi, A., Saffar, H., Abdollahi, A., Mohammadpour, H., Kharazi Fard, M.J., and Memarha, A. 2020. High frequency of braf v600e mutation in Iranian population ameloblastomas. Medicina Oral, Patologia Oral, Cirugia Bucal. 25: e502-e507.
Dhanuthai K., Chantarangsu S., Rojanawatsirivej S., Phattarataratip E., Darling M., Jackson-Boeters L., Said-Al-Naief N., Shin H.I., An C.H., Hong N.T. et al. 2012. Ameloblastoma: A multicentric study. Oral Surgery, Oral Medicine, Oral Pathology, and Oral Radiology. 113: 782-788.
Dhillon, A.S., Hagan, S., Rath, O., and Kolch, W. 2007. Map kinase signalling pathways in cancer. Oncogene. 26: 3279-3290.
do Canto, A.M., da Silva Marcelino, B.M.R., Schussel, J.L., Wastner, B.F., Sassi, L.M., Corrêa, L., de Freitas, R.R., Hasséus, B., Kjeller, G., Junior, C.A.L., et al. 2019. Immunohistochemical analysis of braf v600e mutation in ameloblastomas. Clinical Oral Investigations. 23: 779-784.
Effiom, O.A., Ogundana, O.M., Akinshipo, A.O., and Akintoye, S.O. 2018. Ameloblastoma: Current etiopathological concepts and management. Oral Diseases. 24: 307-316.
El-Naggar, A.K., Chan, J.K.C., Grandis, J.R., Takata, T., and Slootweg, P.J. 2017. WHO classcification of haed and neck tumors. International Agency for Research on Cancer (IARC).
Faden, D.L. and Algazi, A. 2016. Durable treatment of ameloblastoma with single agent brafi re: Clinical and radiographic response with combined braf-targeted therapy in stage 4 ameloblastoma. Journal of the National Cancer Institute. 109: djw190.
Fala, L. 2015. Ofev (nintedanib): first tyrosine kinase inhibitor approved for the treatment of patients with idiopathic pulmonary fibrosis. American Health & Drug Benefits. 8(Spec Feature): 101-104.
Fernandes, G.S., Girardi, D.M., Bernardes, J.P.G., Fonseca, F.P., and Fregnani, E.R. 2018. Clinical benefit and radiological response with braf inhibitor in a patient with recurrent ameloblastoma harboring v600e mutation. BMC Cancer. 18: 887.
Goodman, V.L., Rock, E.P., Dagher, R., Ramchandani, R.P., Abraham, S., Gobburu, J.V., Booth, B.P., Verbois, S.L., Morse, D.E., Liang, CY., et al. 2007. Approval summary: Sunitinib for the treatment of imatinib refractory or intolerant gastrointestinal stromal tumors and advanced renal cell carcinoma. Clinical Cancer Research. 13: 1367-1373.
Gültekin, S.E., Aziz, R., Heydt, C., Sengüven, B., Zöller, J., Safi, A.F., Kreppel, M., and Buettner, R. 2018. The landscape of genetic alterations in ameloblastomas relates to clinical features. Virchows Archiv: An International Journal of Pathology. 472: 807-814.
Guo, Y.J., Pan, W.W., Liu, S.B., Shen, Z.F., Xu, Y., and Hu, L.L. 2020. Erk/mapk signalling pathway and tumorigenesis. Experimental and Therapeutic Medicine. 19: 1997-2007.
Hagen, B. and Trinh, V.A. 2014. Managing side effects of vemurafenib therapy for advanced melanoma. Journal of the Advanced Practitioner in Oncology. 5: 400-410.
Johnson, G.L., Stuhlmiller, T.J., Angus, S.P., Zawistowski, J.S., and Graves, L.M. 2014. Molecular pathways: Adaptive kinome reprogramming in response to targeted inhibition of the braf-mek-erk pathway in cancer. Clinical Cancer Research. 20: 2516-2522.
Junttila, M.R., Li, S.P., and Westermarck, J. 2008. Phosphatase-mediated crosstalk between mapk signaling pathways in the regulation of cell survival. ASEB Journal. 22: 954-965.
Katoh, M. and Nakagama, H. 2014. Fgf receptors: Cancer biology and therapeutics. Medicinal Research Reviews. 34: 280-300.
Kaye, F.J., Ivey, A.M., Drane, W.E., Mendenhall, W.M., and Allan, R.W. 2015. Clinical and radiographic response with combined braf-targeted therapy in stage 4 ameloblastoma. Journal of the National Cancer Institute. 107: 378.
Kelppe, J., Thorén, H., Ristimäki, A., Haglund, C., Sorsa, T., and Hagström, J. 2019. Braf v600e expression in ameloblastomas-a 36-patient cohort from helsinki university hospital. Oral Diseases. 25: 1169-1174.
Keshet, Y. and Seger, R. 2010. The map kinase signaling cascades: A system of hundreds of components regulates a diverse array of physiological functions. Methods in Molecular Biology. 661: 3-38.
Kim, G., McKee, A.E., Ning, Y.M., Hazarika, M., Theoret, M., Johnson, J.R., Xu, Q.C., Tang, S., Sridhara, R., Jiang, X., et al. 2014. FDA approval summary: Vemurafenib for treatment of unresectable or metastatic melanoma with the brafv600e mutation. Clinical Cancer Research. 20: 4994-5000.
Kommalapati, A., Tella, S.H., Borad, M., Javle, M., and Mahipal, A. 2021. Fgfr inhibitors in oncology: Insight on the management of toxicities in clinical practice. Cancers (Basel). 13: 2968.
Konchanthes, S. and Chamusi, N. 2018. Desmoplastic ameloblastoma: A report of two cases. Chiang Mai Dental Journal. 39: 127-136.
Lapthanasupkul, P., Laosuk, T., Ruangvejvorachai, P., Aittiwarapoj, A., and Kitkumthorn, N. 2020. Frequency of braf v600e mutation in a group of thai patients with ameloblastomas. Oral Surgery, Oral Medicine, Oral Pathology, and Oral Radiology. 132: e180-e185.
Lawson-Michod, K.A., Le, C.H., Tranesh, G., Thomas, P.C., and Bauman, J.E. 2022. Precision medicine: Sustained response to erdafitinib in fgfr2-mutant, multiply recurrent ameloblastoma. Cancer Reports (Hoboken).e1656.
Liu, F., Yang, X., Geng, M., and Huang, M. 2018. Targeting erk, an achilles' heel of the mapk pathway, in cancer therapy. Acta Pharmaceutica Sinica B. 8: 552-562.
Markham, A. and Keam, S.J. 2020. Selumetinib: first approval. Drugs. 80: 931-937.
Matallanas, D., Birtwistle, M., Romano, D., Zebisch, A., Rauch, J., von Kriegsheim, A., and Kolch, W. 2011. Raf family kinases: Old dogs have learned new tricks. Genes Cancer. 2: 232-260.
Mukhopadhyay, S., Maitra, A., and Choudhury, S. 2021. Selumetinib: The first ever approved drug for neurofibromatosis-1 related inoperable plexiform neurofibroma. Current Medical Research and Opinion. 37: 789-794.
Nair, A., Reece, K., Donoghue, M.B, Yuan, W.V., Rodriguez, L., Keegan, P., and Pazdur, R. 2021. Fda supplemental approval summary: Lenvatinib for the treatment of unresectable hepatocellular carcinoma. Oncologist. 26: e484-e491.
Neville, B.W., Damm, D.D., Allen, C.M., and AC, C. 2016. Odontogenic cysts and tumors. Oral and maillofacial pathology. 4 ed. Elsevier. p. 632-689.
Nguyen, D.T. and Shayahi, S. 2013. Pazopanib: Approval for soft-tissue sarcoma. Journal of the Advanced Practitioner in Oncology. 4: 53-57.
Oh, K.Y., Cho, S.D., Yoon, H.J., Lee, J.I., Ahn, S.H., and Hong, SD. 2019. High prevalence of braf v600e mutations in korean patients with ameloblastoma: Clinicopathological significance and correlation with epithelial-mesenchymal transition. Journal of Oral Pathology & Medicine. 48: 413-420.
Ornitz, D.M. and Itoh, N. 2015. The fibroblast growth factor signaling pathway. Wiley Interdisciplinary Reviews: Developmental Biology. 4: 215-266.
Panyavaranant, P., Teerapakpinyo, C., Pohthipornthawat, N., Oranratanaphan, S., Shuangshoti, S., and Triratanachat, S. 2019. Ras mutation in mucinous carcinoma of the ovary. Asian Pacific Journal of Cancer Prevention. 20: 1127-1132.
Ranjbari, N., Almasi, S., Mohammadi-asl, J., and Rahim, F. 2013. Braf mutations in Iranian patients with papillary thyroid carcinoma. Asian Pacific Journal of Cancer Prevention. 14: 2521-2523.
Saghravanian, N., Salehinejad, J., Ghazi, N., Shirdel, M., and Razi, M. 2016. A 40-year retrospective clinicopathological study of ameloblastoma in Iran. Asian Pacific Journal of Cancer Prevention. 17: 619-623.
Sandoval, S/, Pigazzi, M., and Sakamoto, K.M. 2009. Creb: A key regulator of normal and neoplastic hematopoiesis. Advances in Hematology. 2009: 634292.
Schreiber, M., Kolbus, A., Piu, F., Szabowski, A., Möhle-Steinlein, U., Tian, J., Karin, M., Angel, P., and Wagner, E.F. 1999. Control of cell cycle progression by c-jun is p53 dependent. Genes & Development. 13: 607-619.
Seki-Soda, M., Sano, T., Ito, K., Yokoo, S., and Oyama, T. 2020. An immunohistochemical and genetic study of braf(v600e) mutation in japanese patients with ameloblastoma. Pathology International. 70: 224-230.
Shirley, M. 2018. Encorafenib and binimetinib: first global approvals. Drugs. 78: 1277-1284.
Simanshu, D.K., Nissley, D.V., and McCormick, F. 2017. Ras proteins and their regulators in human disease. Cell. 170: 17-33.
Sweeney, R.T., McClary, A.C., Myers, B.R., Biscocho, J., Neahring, L., Kwei, K.A., Qu, K., Gong, X., Ng, T., Jones, C.D., et al. 2014. Identification of recurrent smo and braf mutations in ameloblastomas. Nature Genetics. 46: 722-725.
Tan, S., Pollack, J.R., Kaplan, M.J., Colevas, A.D., and West, R.B. 2016. Braf inhibitor treatment of primary braf-mutant ameloblastoma with pathologic assessment of response. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 122: e5-e7.
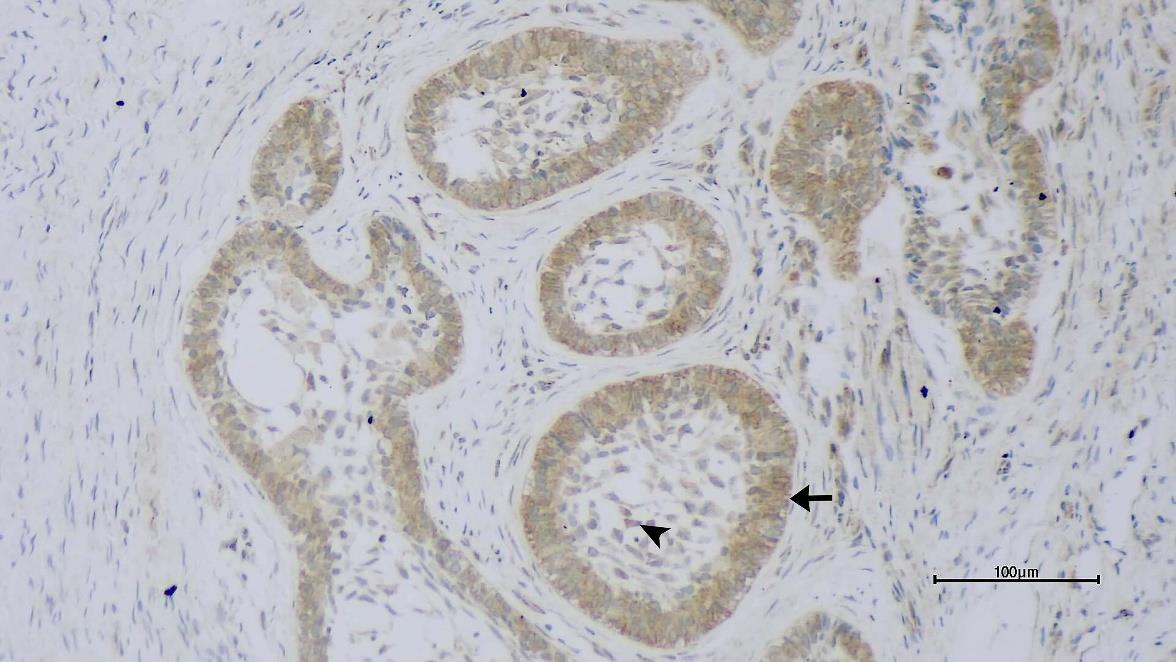
Tang, Y. and Ji, T. 2017. Expression of fibroblast growth factor receptor type 2 in primary and recurrent ameloblastoma are correlated with ameloblastoma clinic characteristics. International Journal of Oral and Maxillofacial Surgery. 46(Supplement 1): 315.
Tran, B. and Cohen, M.S. 2020. The discovery and development of binimetinib for the treatment of melanoma. Expert Opinion on Drug Discovery 15: 745-754.
Turner, N. and Grose, R. 2010. Fibroblast growth factor signalling: From development to cancer. Nature Reviews Cancer. 10: 116-129.
Uehling, D.E. and Harris, P.A. 2015. Recent progress on map kinase pathway inhibitors. Bioorganic & Medicinal Chemistry Letters. 25: 4047-4056.
Weaver, A.N., Francisque, F., and Bowles, D.W. 2020. Tumor regression after treatment with lenvatinib in fgfr2-mutated ameloblastoma. JCO Precision Oncology. 4: 1403-1406.
Welsh, S.J. and Corrie, P.G. 2015. Management of braf and mek inhibitor toxicities in patients with metastatic melanoma. Therapeutic Advances in Medical Oncology. 7: 122-136.
Xie, Y., Su, N., Yang, J., Tan, Q., Huang, S., Jin, M., Ni, Z., Zhang, B., Zhang, D., Luo, F., et al. 2020. FGF/FGFR signaling in health and disease. Signal Transduction and Targeted Therapy. 5, 181.
You, Z., Liu, S.P., Du, J., Wu, Y.H., and Zhang, S.Z. 2019. Advancements in mapk signaling pathways and mapk-targeted therapies for ameloblastoma: a review. Journal of Oral Pathology & Medicine. 48: 201-205.
OPEN access freely available online
Chiang Mai University Journal of Natural Sciences [ISSN 16851994]
Chiang Mai University, Thailand.
https://cmuj.cmu.ac.th