
Correlation between Skin Prick Test and Specific IgE of Local Mites Allergen in Atopic Dermatitis Patients: an Indonesian Study
Sylvia Anggraeni, Menul Ayu Umborowati, Damayanti, Anang Endaryanto, and Cita Rosita Sigit Prakoeswa*Published Date : 2022-10-18
DOI : https://doi.org/10.12982/CMUJNS.2022.053
Journal Issues : Number 4, October-December 2022
Abstract There are two methods that can be used to detect the causative of allergen that trigger the occurrence of Atopic Dermatitis (AD): skin prick test (SPT) and specific IgE (sIgE). Indonesia has developed SPT using local allergens extract to be used as an allergen diagnostic tool. This study aims to determine the correlation between local SPT from Indonesia and sIgE of mites. As many as 45 subjects who met the inclusion criteria were included in this study. Skin prick test was evaluated twice, one week apart. The first SPT was done with standard SPT, and second SPT with local SPT. The sIgE examination was examined at the second week, after performing SPT with local allergen extracts. The subjects in this study were 18-60 years old and dominated by females (75.56%). The three diagnostic tools used in this study showed the same clinical relevance (68.89%). From the mites sIgE examination, it was found that Tyrophagus putrescentiae was the most common sensitized allergen found in positive mites SPT (57.78%). The results of this showed significant results (P <0.05) and moderate correlation (r = 0.40-0.69) between sIgE class and wheal diameter of local SPT on mites allergen. This study found that local SPT from Indonesia has good clinical relevance and positive correlation with other diagnostic tools that already exist, therefore can be considered as a diagnostic tool for determining the cause of atopic dermatitis in the future.
Keywords: Atopic dermatitis, Skin prick test, Specific IgE, Human and disease.
Funding: This research was funded by Direktorat Riset dan Pengabdian Masyarakat, Deputi Bidang Penguatan Riset dan Pengembangan Kementerian Riset dan Teknologi/ Badan Riset dan Inovasi Nasional Indonesia.
Citation: Anggraeni, S., Umborowati, M.A., Damayanti, Endaryanto, A., Prakoeswa, C.R.S. 2022. Correlation between skin prick test and specific IgE of local mites allergen in atopic dermatitis patients: an indonesian study. CMUJ. Nat. Sci. 21(4): e2022053.
INTRODUCTION
Atopic dermatitis (AD) is chronic skin inflammation that manifested as recurrent eczematous lesions and intense pruritus which exacerbated by many trigger factors such as allergens, emotional stress, infection, and climate change (Solomon et al., 2019; Langan et al., 2020). Atopic dermatitis frequently associated with other atopic diseases such as allergic rhinitis, asthma, and food allergy (Solomon et al., 2019). Atopic dermatitis is one of the most common skin diseases where almost one fifth of the population of developing countries is affected. It is estimated that AD affects about 15–20% of children and 1–3% of adults (Nutten, 2015; Langan et al., 2020). The prevalence of AD has increased during the past decades, especially in the Europe, United States (US), and Japan. In the US the prevalence of AD in children was reported to be 11.3-12.7% and 6.9-7.6% in adults. The prevalence of AD in Indonesia is estimated at 23.67% (Wicaksana et al., 2017; Torres et al., 2019; Kim et al., 2019).
Mites are one of the most common allergens in the world. They can cause several allergic diseases such as atopic dermatitis, asthma, and allergic rhinitis, which can not only affect the quality of life, but can also cause morbidity and mortality (Taha et al., 2018; Miller, 2019). The most common species of mites found in Indonesia are Dermatophagoides farinae which is commonly found in sofas and Dermatophagoides pteronyssinus which can be found in dust and many stuff such as mattresses, bedding, and stuffed animal (Anggraeni et al., 2021; Huang et al., 2017; Putera et al., 2021). Avoiding exposure to dust mites is recommended by many clinicians for the prevention and treatment of patients with AD (Bumbacea et al., 2020).
There are 2 methods that can be used to detect the causative allergen, which are skin prick test (SPT) and specific IgE (sIgE). In many countries, SPT is considered as gold standard for diagnostic method, while sIgE is a complementary test. Both methods may have the advantages and disadvantages. SPT is inexpensive, quick, and sensitive; while sIgE assay is more specific, but also more expensive and the results cannot come out right away (Kumar et al., 2015; Bignardi et al., 2019). In addition, SPT examination also cannot be performed on patients with dermatographism, pregnant women, infants and toddlers, and currently undergoing certain drug therapy such as antihistamines and beta blockers. Specific IgE antibody testing is an option if there are conditions as mentioned above (Yudhistira et al., 2019).
The cost of imported allergen extracts for SPT, which is considered as the gold standard, is quite high. Furthermore, they are not always available in Indonesia. Therefore, a skin prick test with a local allergen was made. This study aims to determine the correlation between local SPT from Indonesia and sIgE of mites.
MATERIAL AND METHODS
Subject of this clinical trial study were 45 patients of Allergy-Immunology Division Outpatient Clinic of Dr Soetomo General Academic Hospital Surabaya, Indonesia who meet the inclusion and exclusion criteria. The sampling technique for this study was purposive sampling. The sample size were determined by sample size formula for diagnostic test using disease prevalence of 55.2% (Heinzerling et al., 2013; Suwarsa et al., 2017; Negida et al., 2019). The inclusion criteria were patients with AD history, aged 18-64 years old, in good health at the time of examination, and willing to participate in the study by filling out an informed consent form. The exclusion criteria were pregnant women, suffering from atopic dermatitis or other skin diseases at the time of examination, previous history of anaphylactic shock, having a history of chronic disease, or taking certain medications in the past 2 weeks.
The subjects of this study were examined for SPT and the sIgE for mites allergen. Before SPT and the sIgE examination, subject history taking and physical examination was performed. This include the age, gender, self and family history of atopic disease, complete questionnaire of Hanifin Rajka criteria, and history of suspected mites allergy. House dust mites SPT allergen extract used for this study was extracted from Dermatophagoides pteronyssinus. Standard SPT allergen extract was produced by Astromed® dan local SPT allergen extract was produced by Teaching Industry Allergen by Dr.Soetomo Hospital-Universitas Airlangga, Surabaya, Indonesia (Putera et al., 2021). The production of local SPT has 9 steps of manufacturing an allergen extract including comminution, defatting, extraction, clarification, dialysis, concentration, sterilization, standardization, and quality control.
SPT was evaluated twice, one week apart. The first SPT was done on the right volar side of the forearm using standard allergen extracts. The testing area was denoted by a minimum of 3 cm between allergens. In the testing area, the subject’s skin was dripped with standard allergen extracts and then pricked by microlancette (1 microlancette was used for 1 allergen). For the next step, allergen extract was removed promptly with sterile gauze. The results were read after 15-20 minutes. The induration is measured and considered as positive SPT result if its diameter is more than 3 mm, with the induration of positive control is more than 3 mm and negative control less than 3 mm. The second SPT was done 1 week following the first SPT. The same process was repeated on the left volar side of the forearm with new local allergen extracts. Before performing the second SPT, adverse effects from the first SPT was evaluated.
The sIgE examination was examined at second week, after performing SPT with local allergen extracts. Mites allergen consist of Dermatophagoides farinae, Dermatophagoides pteronyssinus, Dermatophagoides microceras, Thyrophagus putrescentiae, and Blomia tropicalis. The sIgE result was considered positive if the concentration is more than 0.35 kU/I. The sIgE test was using Allergy Euroline Atopy Indonesia 1 by Prodia Clinical Laboratory (CAP accredited).
This study used descriptive statistics (mean, minimum, maximum, and percentage) to describe the variables, and Spearman correlation. The result is significant if the p value is less than 0.05. SPSS version 25.0 was used to analyze the statistical data. This study was approved by Ethical Committee of Dr Soetomo Academic General Hospital, Surabaya, Indonesia (1493/KEPK/IX/2019).
RESULTS
Table 1 showed the characteristics of patients in this study. Subject of this study were 45 patients, 75.56% of them were female. The patient’s age range was 18-60 years, with a mean age of 27.2 + 8.016 years. Most patients were in the age group of 21-30 years old (34 patients; 75.56%).
Table 1. Subject characteristics.
|
Characteristics |
Total(%) |
|
Gender |
|
|
Female |
34 (75.56) |
|
Male |
11 (24.44) |
|
Age |
|
|
Mean + SD, years |
27.20 + 8.01 |
|
Range, years |
18 – 60 |
|
Age Group (years old) |
|
|
≤20 |
4 (8.89) |
|
21-30 |
34 (75.56) |
|
31-40 |
4 (8.89) |
|
41-50 |
1 (2.22) |
|
51-60 |
2 (4.44) |
Hanifin Rajka criteria was used to diagnose atopic dermatitis of the subjects in this study. The most common clinical symptom was itchy skin/pruritus, which was complained by 38 patients (84.44%). Furthermore, 37 patients (82.22%) complained of typical morphology and distribution of AD lesions. A total of 22 patients (48.89%) had chronic/chronically-relapsing complaints and 42 patients (93.33%) had history of atopic disease. Dry skin was complained by 29 patients (64.44%) and scaly skin was complained by 15 patients (33.33%). A total of 29 patients (64.44%) admitted that their complaints were influenced by environmental/emotional factor and 21 patients (46.67%) had early age onset of AD.
Atopic history in the patients and their family showed in Figure 1. A total of 42 patients (93.33%) had self-history of atopic disease. Atopic dermatitis was the most common self-history of atopic disease in 31 patients (68.89%) followed by food allergy in 25 patients (55.56%) and rhinitis allergic in 23 patients (51.11%). A total of 24 patients (53.33%) had history of atopic disease in their family. A total of 11 patients (24.44%) had history of food allergy and 9 patients (20%) had history of rhinitis allergy in their family.
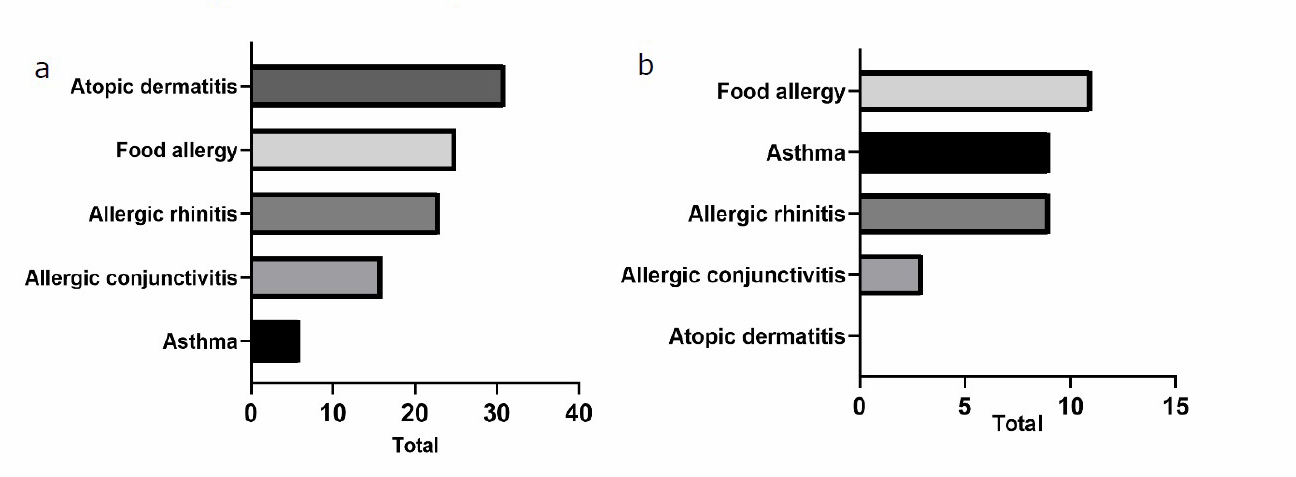
Figure 1. History of atopic disease including self history (a) and family history (b). One subject might have more than 1 answer.
In this study, a total of 33 patients had history of suspected HDM allergy among 45 atopic dermatitis patients diagnosed with Hanifin Rajka criteria. Figure 2 showed the results of local mites SPT, standard SPT, and sIgE and the clinical relevance to history of suspected HDM allergy. It was shown that 26 subjects (57.77%) got positive results from local SPT, 28 subjects (62.22%) got positive results from standard SPT and 23 subjects (51.11%) got at least 1 positive result from sIgE test. The three diagnostic tools used in this study showed the same clinical relevance of 68.89% (31 out of 45) consisted of patients with history of HDM allergy who got positive SPT or sIgE result and patients with no history of HDM allergy who got negative SPT or sIgE result.
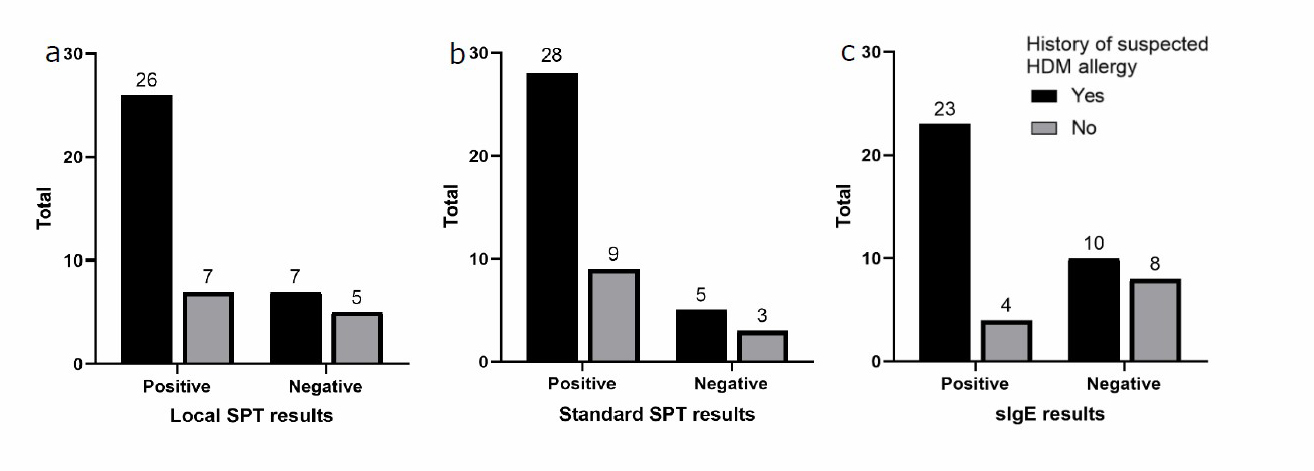
Figure 2. The results of SPT and sIgE and the clinical relevance to the subjects’ history of suspected HDM allergy.
Distribution of mites sIgE results and class of sIgE is shown in Figure 3. From the mites sIgE examination, it was found that Tyrophagus putrescentiae was the most common sensitized allergen (57.78%), followed by Dermatophagoides microceras (48.89%). Specific IgE class consists of 6 classes as follows: Class 0 (0 < sIgE < 0,35 kU/l), Class 1 (0,35 < sIgE < 0,7 kU/l), Class 2 (0,7 < sIgE < 3,5 kU/l), Class 3 (3,5 < sIgE < 17,5 kU/l), Class 4 (17,5 < sIgE < 50 kU/l), Class 5 (50 < sIgE < 100 kU/l), Class 6 (sIgE > 100 kU/l).
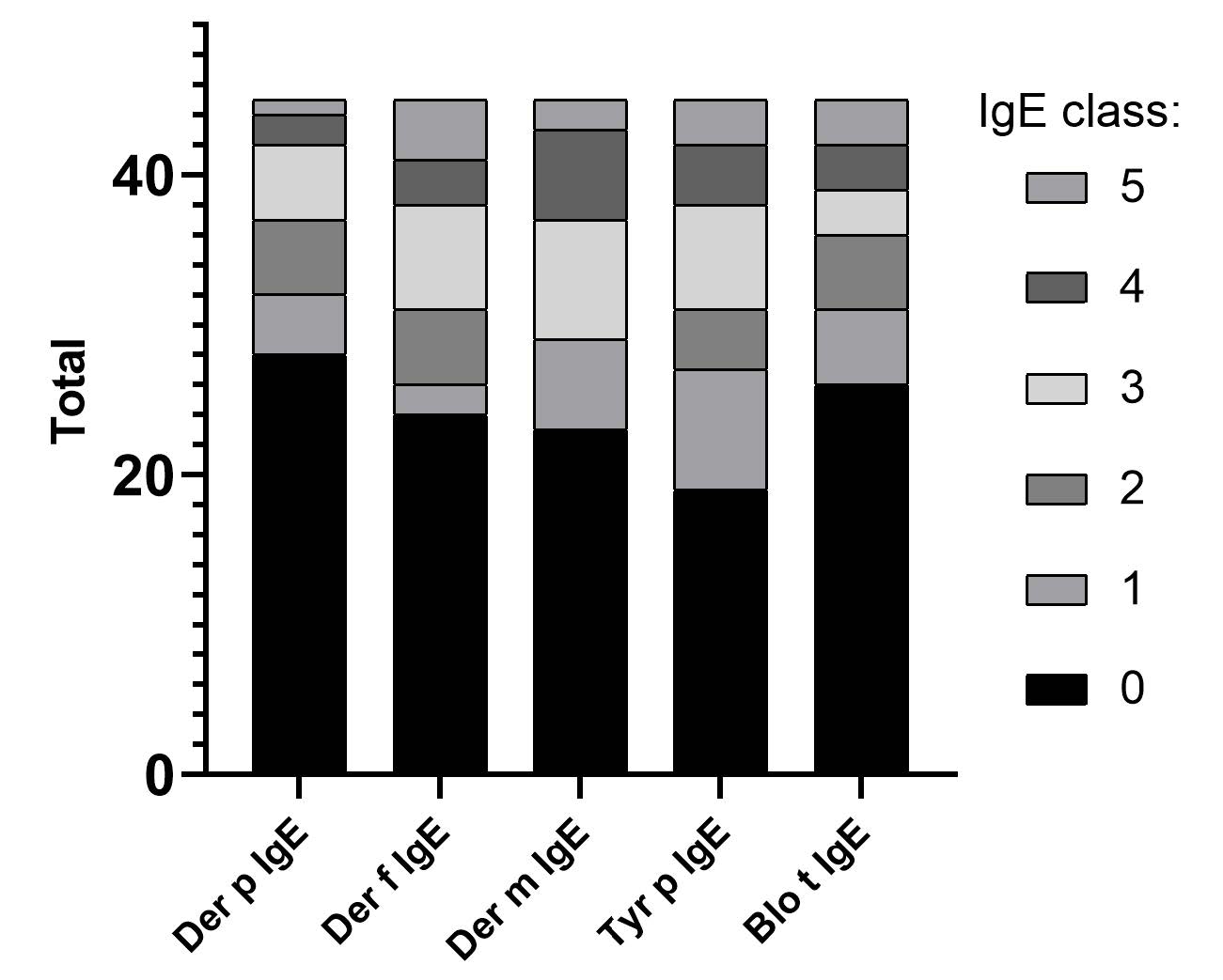
Figure 3. Distribution of mites sIgE sensitization (n=45).
The correlation between sIgE class and wheal diameter of local SPT on mites allergen is shown in Figure 4. All results showed significant results (P <0.001) and moderate correlation (r = 0.40-0.69) using Spearman correlation analysis.
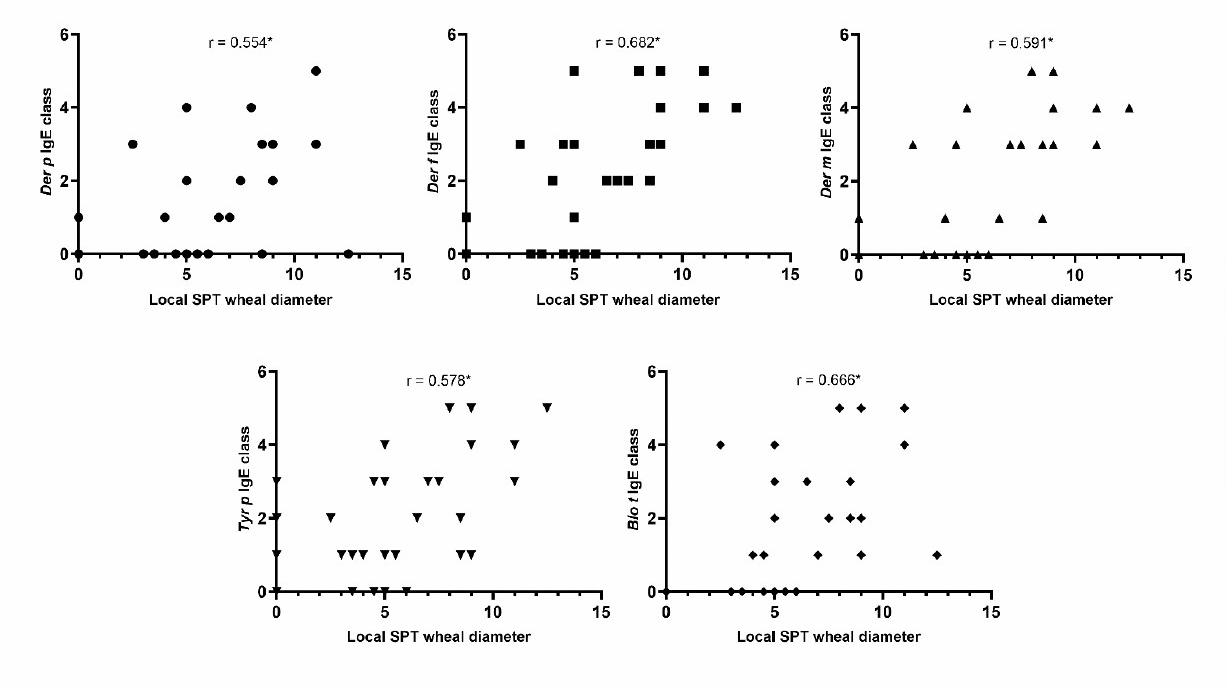
Figure 4. Scatter plot diagrams between sIgE class and local mites SPT wheal diameter (cm). Spearman correlation coefficients (r) are included in the diagrams.*Statistically significant with P<0.001.
DISCUSSION
The subjects in this study were dominated by females, as many as 75.56%. This is in accordance with previous epidemiological studies which said that atopic dermatitis was more common in female than male with a ratio of 1.27-2 : 1.1 (Munthaha et al., 2021; Sendrasoa et al., 2021).
According to Hanifin Rajka's criteria, up to 84.44% of patients reported experiencing itchy symptoms. In accordance with the theory, itching is the most prominent and disturbing symptom of AD so that it can affect the quality of life. Although the etiology of itch in AD is still unclear, multiple studies have demonstrated hyperinnervation of the epidermis, increased levels of several itch mediators/pruritogens, and central sensitization of itch in AD (Rerknimitr et al., 2017; Simpson et al., 2019). Along with itching, the majority of the patients also had lesions typical of atopic dermatitis and had experienced this disease for a long time and repeatedly. The presence of precipitating factors can worsen the symptoms of atopic dermatitis and cause recurrence of this disease. In addition to allergen exposure, emotional and environmental conditions can also influence the recurrence of AD. Low outdoor temperature, pollution / tobacco smoke, and fast food diet are known to be several factors that increase the risk of atopic dermatitis (Nutten, 2015). The same goes for psychological stress. Glucocorticoid changes due to psychological stress can inhibit the synthesis of ceramides, cholesterols, and free fatty acids. This causes the disruption of hydrophobic barrier, resulting in increased water loss from the skin, aggravating AD and other inflammatory skin conditions (Boothe et al., 2017).
From the Hanifin Rajka’s criteria, it was also known that many subjects have dry skin. Dry skin is a manifestation of a damaged skin barrier. The defect in filaggrin gene may have a role in the degradation of the epidermal barrier in AD patients. In the stratum corneum and stratum granulosum, the filaggrin gene encodes structural proteins that aid in the adhesion of keratinocytes which maintains the integrity of the skin barrier and the hydration of the stratum corneum. Due to gene mutations / defects, less filaggrin is produced, resulting in a dysfunctional skin barrier and transepidermal water loss, which causes eczema (Thomsen, 2014; Simpson et al., 2019).
According to the findings of this study, the majority of patients had a personal or family history of atopy. This is consistent with the theory which stated that AD usually coexists with other atopic disorders such as allergic rhinitis, asthma, and food allergy (Solomon et al., 2019). This is also consistent with a prior study that found that 70% of AD patients had a first-degree relative who had atopy (Sendrasoa et al., 2021). The sensitization to HDM detected with local SPT was found in 26 subjects (57.77%). This was similar with a study of adult AD patients in Indonesia that found the sensitization to HDM was 55.2% (Suwarsa, et al., 2017). In normal population, the sensitization to HDM ranged from 17.8% to 26.1% (Sundaru, 2016; Ambarwati and Ferial, 2021)
The assessment of clinical relevance might lead to more useful findings for clinicians and patients, improving the use of information in clinical practice (Armijo-Olivo et al., 2011). The clinical relevance of IgE-mediated sensitizations must be carefully assessed because positive SPTs may not always indicate allergies. A clinician must consider the SPT results along with the patient’s clinical manifestation, history of allergy, and other allergy test if indicated to establish the diagnosis of allergy (Ansotegui et al., 2020). Clinical relevance shows the percentage of relevance between history taking data and examination data, which in this case were the local SPT, standard SPT, and sIgE. These three diagnostic tools showed the same clinical relevance (68.89%). This shows that history taking is very important in initiating diagnosis.
SPT and sIgE were 2 methods used in the examination of IgE-mediated disease. In this study, 2 types of SPT were used, first was standard SPTs that have been used internationally, and second was local SPTs made in Indonesia. In several countries, the SPT standard is considered the gold standard for allergen examination (Kumar et al., 2015). The results of clinical relevance in this study showed that local SPT is equally as effective as standard SPT, as indicated by the same clinical relevance value. The sIgE examination also showed similar results.
Atopic dermatitis is one of the IgE-mediated diseases. IgE binds to immune cells through high-affinity IgE receptors (FcεRI). Atopic dermatitis patients generally have a damaged skin barrier. The disrupting skin barrier increases its permeability to allergens, and facilitates The response through the skin's antigen-presenting cells, which is Langerhans cells. This results in an increase of IgE production, which is responsible for hypersensitivity reactions to allergen exposures (Mondal et al., 2019).
The allergen that will be further discussed in this study is mite allergen. There are several types of mites, such as house dust mites and storage mites. WHO states that house dust mite allergy is a global health problem that affects patients' quality of life. Many species of mites are found in house dust; however, only three of them are very common worldwide: Dermatophagoides pteronyssinus (Der p), Dermatophagoides farinae (Der f) and Euroglyphus maynei (Eur m). They can be found in temperate climates (Ponggalunggu et al., 2015). Meanwhile, Blomia tropicalis (Blo t) and Tyrophagus putrescentiae (Tyr p), which was originally known as storage mites but now also commonly found in house dust, prevalent in tropical and subtropical climates (Santos da Silva et al., 2017; Shen et al., 2020).
Dermatophagoides farinae and Dermatophagoides pteronyssinus are the most common causes of allergy and sensitization to mites and described in many studies (Thomsen, 2014). But this study showed different results. Tyrophagus putrescentiae is the type of mite that causes the most sensitization in the subjects of this study based on the results of sIgE examination. Tyrophagus putrescentiae is a pest of stored products, especially those high in protein and fat content also known as mites that feed on mold that grows on food. Storage mite sensitization primarily work-related was first described in 1979 in Scottish farmers. Storage mites have also been found in some samples of cereal-based food products purchased at food retail outlets, and samples containing storage mites were found after 6 weeks of storage (Jõgi et al., 2020).
The data in this study also showed a positive-moderate correlation between IgE class and wheal diameter in local SPT, which means that the larger the wheal diameter, the higher the IgE class. This is in accordance with research conducted by Visitsunthorn (2017) and Taha (2018) which showed a positive correlation between specific IgE level and wheal diameter in mite allergen SPT results.
CONCLUSION
This study indicates that Indonesian local SPT has positive correlation with other diagnostic tools that already exist, therefore can be considered as a diagnostic tool for determining allergen sensitization in AD patients in the future.
ACKNOWLEDGMENTS
We would like to express our thanks to Direktorat Riset dan Pengabdian Masyarakat, Deputi Bidang Penguatan Riset dan Pengembangan Kementerian Riset dan Teknologi/ Badan Riset dan Inovasi Nasional Indonesia for supporting this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest regarding the publication.
REFERENCES
Ambarwati, R., and Ferial, L., 2021. Analisis paparan alergen tungau debu di lingkungan sekolah terkait dengan sensitisasi alergi di sekolah dasar di serang tahun 2021. Journal of Baja Health Science. 1: 96-106.
Anggraeni, S., Umborowati, M.A., Damayanti, Endaryanto, A., and Prakoeswa, C.R.S., 2021. The accuracy of indonesian new local skin prick test (spt) allergen extracts as diagnostic tool of IgE-mediated atopic dermatitis. Indian Journal of Forensic Medicine and Toxicology. 15: 4278–85.
Ansotegui, I.J., Melioli, G., Canonica, G.W., Caraballo, L., Villa, E., Ebisawa M., et al., 2020. IgE allergy diagnostics and other relevant tests in allergy, a World Allergy Organization position paper. World Allergy Organ Journal. 13: 100080.
Armijo-Olivo, S., Warren, S., Fuentes, J., and Magee, D.J., 2011. Clinical relevance vs. statistical significance: using neck outcomes in patients with temporomandibular disorders as an example. Manual Therapy. 16: 563-572.
Bignardi, D., Comite, P., Mori, I., Ferrero, F., Fontana, V., Bruzzone, M. et al., 2019. Allergen-specific IgE: comparison between skin prick test and serum assay in real life. Allergologie select. 3: 9–14.
Boothe, W.D., Tarbox, J.A., and Tarbox, M.B., 2017. Atopic dermatitis : pathophysiology. Advances in Experimental Medicine and Biology. 1027: 21–37.
Bumbacea, R.S., Corcea, S.L., Ali, S., Dinica, L.C., Fanfaret, I.S., and Boda, D., 2020. Mite allergy and atopic dermatitis: Is there a clear link? (Review). Experimental and Therapeutic Medicine. 20: 3554–60.
Heinzerling L, Mari A, Bergmann KC, Bresciani M, Burbach G, Darsow U, et al., 2013. The skin prick test - European standards. Clinical and Translational Allergy. 3: 1–10.
Huang, F.L., Liao, E.C., and Yu, S.J., 2017. House dust mite allergy: Its innate immune response and immunotherapy. Immunobiology. 223: 300–302.
Jõgi, N.O., Kleppe, Olsen. R., Svanes, C., Gislason, D., Gislason, T., Schlünssen, V. et al., 2020. Prevalence of allergic sensitization to storage mites in Northern Europe. Clinical and Experimental Allergy. 50: 372–382.
Kim, J., Kim, B.E., and Leung, D.Y.M., 2019. Pathophysiology of atopic dermatitis: Clinical implications. Allergy and Asthma Proceedings. 40: 84–92.
Kumar, R., Gupta, N., Kanuga, J., and Kanuga, M., 2015. A comparative study of skin prick test versus serum-specific IgE measurement in indian patients with bronchial asthma and allergic rhinitis. Indian Journal of Chest Diseases and Allied Sciences. 57: 81–85.
Langan, S.M., Irvine, A.D., and Weidinger, S., 2020. Atopic dermatitis. Lancet. 396: 345–360.
Miller, J.D., 2019. The role of dust mites in allergy. Clinical Reviews in Allergy & Immunology. 57: 312–329.
Mondal, P., Dey, D., Saha, N.C., Moitra, S., Saha, G.K., Bhattacharya, S. et al., 2019. Investigation of house dust mite induced allergy using logistic regression in West Bengal, India. World Allergy Organ Journal. 12: 100088.
Munthaha, M.I.A, Widayati, R.I., Afriliana, L., and Candra, A., 2021. Characteristics of atopic dermatitis in puskesmas (public health center) masaran 1 sragen regency. Jurnal Kedokteran Diponegoro. 10:27–34.
Negida, A., Fahim, N. K., & Negida, Y., 2019. Sample size calculation guide - part 4: how to calculate the sample size for a diagnostic test accuracy study based on sensitivity, specificity, and the area under the ROC curve. Advanced Journal of Emergency Medicine. 3: e33.
Nutten, S., 2015. Atopic dermatitis: global epidemiology and risk factors. Annals of Nutrition and Metabolism. 66: 8–16.
Ponggalunggu, W.F., Pijoh, V.D., and Wahongan, G.J.P., 2015. Jenis dan kepadatan tungau debu rumah pada beberapa habitat di rumah penderita penyakit alergi. Journal e-Biomedik. 3: 254–260.
Putera, A.M., Hikmah, Z., Endaryanto, A., Irwanto, and Maramis, M.M., 2021. The role of house dust mite immunotherapy in Indonesian children with chronic rhinosinusitis allergy: A randomized control trial. Heliyon. 7: e06510.
Rerknimitr, P., Otsuka, A., Nakashima, C., and Kabashima, K., 2017. The etiopathogenesis of atopic dermatitis: Barrier disruption, immunological derangement, and pruritus. Inflammation and Regeneration. 37: 1–15.
Santos Da Silva, E., Asam, C., Lackner, P., Hofer, H., Wallner, M., and Silva Pinheiro, C. et al., 2017. Allergens of Blomia tropicalis: an overview of Recombinant Molecules. International Archives of Allergy and Immunology. 172: 203–14.
Sendrasoa, F.A., Ramily, S.L., Razafimaharo, T.I., Ranaivo, I.M., Andrianarison, M., Raharolahy, O. et al., 2021. Atopic dermatitis in adults: A cross-sectional study in the department of dermatology, Antananarivo, Madagascar. JAAD International. 4: 28–31.
Shen, C.Y., Yen, C.Y., Chien, D.K., Tsai, J.J., Yu, S.J., and Liao, E.C., 2020. Influence of storage conditions on the infestation of Tyrophagus putrescentiae and prevalence of mite hypersensitivity in Taiwan. Experimental and Applied Acarology. 80: 381–398.
Simpson, E.L., Leung, D.Y.M., Eichenfield, L.F., and Boguniewicz, M., 2019. Atopic Dermatitis. p. 363–84. In Kang, S., Amagai, M., Bruckner, A.L., Enk, A.H., Margolis, D.J., McMichael, A.J., et al. [eds] Fitzpatrick’s Dermatology 9th ed. McGraw-Hill Education, New York.
Solomon, I., Ilie, M.A., Draghici, C., Voiculescu, V.M., Căruntu, C., Boda, D., et al., 2019. The impact of lifestyle factors on evolution of atopic dermatitis : An alternative approach (Review). Experimental and Therapeutic Medicine. 17: 1078–84.
Sundaru, H., 2006. House dust mite allergen level and allergen sensitization as risk factors for asthma among student in Central Jakarta. Medical Journal of Indonesia. 15(1): 55-9. doi: 10.13181/mji.v15i1.213
Suwarsa, O., Sormin, E. R., Sutedja, E., & Dharmaji, H. P., 2017. The positive skin prick test not correlate with disease severity and quality of life in atopic dermatitis patients. Berkala Ilmu Kesehatan Kulit Dan Kelamin. 29: 229–233.
Taha, A.A.E.R., Etewa, S.E., Abdel-Rahman, S.A., Al Ghandour, A.M.F., Atta, A.H., and Darwish, A.M., 2018. House dust mites among allergic patients at the Allergy and Immunology Unit, Zagazig University: an immunologic and serologic study. Journal of Parasitic Diseases. 42: 405–15.
Thomsen, S.F., 2014. Atopic dermatitis: Natural history, diagnosis, and treatment. ISRN Allergy. 2014: 354250.
Torres, T., Ferreira, E.O., Gonçalo, M., Mendes-bastos, P., Selores, M., and Filipe, P., 2019. Update on atopic dermatitis. Orden Dos Médicos. 32: 606–613.
Visitsunthorn, N., Sripramong, C., Bunnag, C., and Jirapongsananuruk, O., 2017. Comparison between specific IgE levels and skin prick test results of local and imported American cockroach, dog, cat, dust mites and mold allergen extracts. Asian Pacific Journal of Allergy and Immunology. 35: 60–65.
Wicaksana, M.A., Suwarsa, O., and Dwiyatnaningrum, F., 2017. Quality of life in families with children with atopic dermatitis. Althea Medical Journal. 4: 335–339.
Yudhistira, Sukartini, N., Immanuel, S., and Rengganis, I., 2019. Evaluasi pemeriksaan imunoglobulin E spesifik menggunakan immunoblot assay dengan baku emas skin prick test. Cermin Dunia Kedokteran. 46: 91–97.
OPEN access freely available online
Chiang Mai University Journal of Natural Sciences [ISSN 16851994]
Chiang Mai University, Thailand.
https://cmuj.cmu.ac.th
Sylvia Anggraeni1, 2, Menul Ayu Umborowati2, Damayanti2, Anang Endaryanto3, and Cita Rosita Sigit Prakoeswa4,*
1 Researcher, Doctoral Program of Medical Science, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia.
2 Researcher, Department of Dermatology and Venereology, Faculty of Medicine Universitas Airlangga/ Dr. Soetomo General Academic Hospital, Surabaya, Indonesia.
3 Professor, Department of Pediatric, Faculty of Medicine Universitas Airlangga/ Dr. Soetomo General Academic Hospital, Surabaya, Indonesia.
4 Professor, Department of Dermatology and Venereology, Faculty of Medicine Universitas Airlangga/ Dr. Soetomo General Academic Hospital, Surabaya, Indonesia.
Corresponding author: Cita Rosita Sigit Prakoeswa, E-mail: cita-rosita@fk.unair.ac.id
Total Article Views
Editor: Veerasak Punyapornwithaya,
Chiang Mai University, Thailand
Article history:
Received: June 2, 2022;
Revised: July 15, 2022;
Accepted: August 9, 2022;
Published online: August 23, 2022

