
Social Cognitive Theory-based Interventions on Healthy Lifestyles for Hypertensive Patients: A Systematic Review
Wachira Suriyawong and Noppamas PipatpiboonPublished Date : 2022-07-11
DOI : https://doi.org/10.12982/CMUJNS.2022.040
Journal Issues : Number 3, July-September 2022
Abstract Effective strategies to promote a long-term healthy lifestyle among hypertensive patients remain unclear. Social cognitive theory (SCT)-based interventions have demonstrated some effectiveness in promoting sustainable lifestyle change in this population. This systematic review aims to synthesize randomized controlled trials (RCTs) examining the effect of SCT-based interventions on healthy lifestyles, including physical activity [PA] and/or diet adherence [DA], in hypertensive patients. Four electronic databases (CINAHL, PubMed, Scopus, and Web of Science) were searched to identify RCTs that: 1) targeted hypertensive patients; 2) reported PA and/or DA as proximal outcomes; and 3) included an intervention guided by the SCT. Narrative and tabulation synthesis were conducted to present the effects of the SCT-based interventions. Fifteen studies were included in this systematic review with 3,388 hypertensive patients (mean age = 52.21, 68.70% female). Findings were inconsistent for the SCT-based interventions targeting multiple behaviors, including DA and PA. Multiple-component interventions, including PA training and identification of PA barriers through group discussion, had a greater effect size on PA improvement (d = .93–.99) than interventions without these components (d = .29–.44). Interventions with a longer duration (> 12 weeks), greater length of time for sessions (150 minutes/session), and higher session frequency (2 days/week) were more effective on DA change (d = .65) than interventions with a shorter duration (< 12 weeks), shorter session length (60–90 minutes), or lesser session frequency (monthly meeting) (d = .09–.51).
Keywords: Social cognitive theory, Hypertension, Physical activity, Diet adherence
Citation: Suriyawong, W. and Pipatpiboon, N. 2022. Social cognitive theory-based interventions on healthy lifestyles for hypertensive patients: a systematic review. CMU J. Nat. Sci. 21(3): e2022040.
INTRODUCTION
Hypertension (high BP), estimated to cause more than 10 million deaths per year, is predicted to reach almost 40% of the world adult population in 2050. The World Health Organization [WHO] reported that only one of every five hypertensive adults has their blood pressure (BP) under control. This problem is a major public health concern because failure to control BP can result in the development of severe cardiovascular disease, including heart failure, myocardial infarction, and diminished quality of life (American Heart Association, 2021).
Diet adherence (DA) and physical activity (PA) play an effective role in BP control for hypertensive patients. The Eighth Joint National Committee proposes that an effective strategy for controlling BP for hypertensive patients includes adopting healthy lifestyles, suggesting PA and DA as the first line of treatment. In addition, DA and PA can reduce the need for pharmacological therapy, improve the effect of antihypertensive medicines, and lower overall cardiovascular risk (Bond Brill, 2011). Numerous systematic reviews and meta-analyses offer evidence of the effects of DA and PA intervention on controlling BP and reducing cardiovascular risk among hypertensive patients. These studies found that PA (moderate to vigorous intensity) decreased the mean of systolic and diastolic BP by 5–12 mmHg and 1–6 mmHg, respectively (Cornelissen and Smart, 2013; Semlitsch et al., 2013; Conceicao et al., 2016). DA interventions, including low-salt and low-fat diets, have been shown to lower the mean of systolic BP by about 3.2–7.62 mmHg and diastolic BP by approximately 2.5–4.22 mmHg (Saneei et al., 2014; Gay et al., 2016; Filippou et al., 2020). Despite the benefits of DA and PA changes on BP control, hypertensive patients' adherence to these guidelines remains suboptimal, comparable to the general population.
Several DA and PA interventions have been shown to improve hypertension patients' health, although little is known about which interventions are the most effective. Behavioral interventions guided by theoretical approaches have been found to be more effective than non-theoretical approaches (Glanz and Bishop, 2010). In addition to providing a framework for intervention design and evaluation, theoretical research sheds light on the mechanisms of behavior change and the factors that determine success or failure (Abraham and Michie, 2008). One theory commonly used to guide behavior change interventions and found to be helpful for understanding the reasons why individuals adopt and sustain their health behaviors is Social Cognitive Theory (SCT) (Bandura, 1998).
The main constructs of SCT include perceived: 1) self-efficacy (SE) or individuals’ confidence in controlling behaviors; 2) outcome expectancies (OE): benefits and cost about maintaining their own health behaviors; and 3) social support (SS). Within SCT constructs, SE plays a critical role to directly maintain individuals’ behaviors through believing in their ability to use skills successfully when facing barriers (Bandura, 1998). Individuals with high SE can effectively apply skills to motivate themselves to sustain their behavior when facing barriers (Bandura, 1987). For instance, individuals with high SE are likely to use goal-setting skills to motivate themselves to overcome personal barriers, such as lack of time, to achieve their goal of sustaining PA (Mbambo et al., 2019). Another SCT construct, OE, influences individuals’ motivation to engage in positive behavior (Bandura, 1998). Individuals can maintain healthy behaviors when they envision the benefits associated with these actions (Resnick et al., 2013). Lastly, SS is an environmental factor in SCT used to understand individuals’ behaviors (Bandura, 1987). There are two essential aspects of SS: 1) structural support, which consists of the number and types of connections within an individual’s social network, and 2) functional support including emotional, informational and instrumental support from family, peers, or others (Sherbourne and Stewart, 1991). Strengthening social networks by building supportive relationships helps individuals maintain their healthy behaviors (i.e., setting up contracts with peers to achieve PA goals, doing PA as a group) (Cohen et al., 2000).
Although recent meta-analyses of healthy lifestyle interventions showed that SCT-based interventions significantly improved DA or PA, these studies were limited to healthy elderly (Young et al., 2014) and cancer patients (Stacey et al., 2015). Little is known about whether SCT-based interventions can improve DA and PA in other populations or about the constructs, components, and intervention characteristics associated with enhanced DA and PA. Presently, no comprehensive reviews were found that examined both PA and DA interventions for hypertensive individuals. While substantial data exist to support the effect of DA and PA on health outcomes, for example blood pressure control, there is a need to examine interventions to understand how to encourage hypertensive individuals to adopt positive, sustainable lifestyle changes.
Thus, the aims of this systematic review were to: 1) synthesize randomized controlled trials (RCTs) assessing the effectiveness of SCT-based interventions on DA and/or PA change; and 2) describe effective approaches to guide future study aimed at designing effective healthy lifestyle interventions for hypertensive patients.
MATERIAL AND METHODS
Data Sources and Search Strategy
This systematic review was conducted following the Cochrane Collaboration methodology (Higgins et al., 2019). The study’s findings were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline (Moher et al., 2009). The initial search strategy, developed by the first author with professional guidance from a university health science librarian, was used to identify relevant published studies testing the effectiveness of Social Cognitive Theory-based interventions on healthy lifestyles in hypertensive patients. Four electronic databases were searched: the Cumulative Index of Nursing and Allied Health Literature (CINAHL) (1989-2021), PubMed (1981-2021), Scopus (1981-2021), and Web of Science (1981-2021). The keywords for investigation were utilized: (((“social cognitive theory” OR “self-efficacy” OR “social support” OR “outcome expectation” OR “outcome expectations” OR “outcomes expectancy” OR “outcomes expectancies”) AND (“healthy lifestyle” OR “nutrition” OR “physical activity” OR “sleep*” OR “diet” OR “Diet[Mesh]” OR “exercis*” OR “Exercise”[Mesh])) AND (“hypertens*”)) AND “intervent*” NOT (“child*” OR “adolescen*”). Additionally, hand-searching from Google Scholar was used to find relevant studies from reference lists cited to ensure an extensive search for all international studies meeting the eligibility criteria.
Eligibility Criteria
Published articles following the criteria were included in this review if they: (1) primarily targeted hypertensive patients above age 18; (2) were RCTs; (3) investigated the effect of the intervention guided by any construct of the Social Cognitive Theory (e.g., self-efficacy, outcome expectations, or social support) on PA and/or on DA; (4) compared the outcomes between an intervention group and a control /comparison group; and (5) were peer-reviewed papers. Studies were excluded if they: were (1) secondary analyses; (2) protocol papers; (3) not published in English language (due to the cost and time needed to translate them) (Arksey and O'Malley, 2005); or (4) review studies; or included (5) participants with diabetes or other cardiovascular diseases (i.e., heart failure, myocardial infarction) or (6) a small sample size (n < 10) in either the experimental or control/comparison groups (see Table 1).
|
Table 1. Keywords searched using the PICOS framework.
|
||||
|
PICOS Framework |
Keywords |
Inclusion Criteria |
Exclusion Criteria |
|
|
Population |
Adult with hypertension |
Hypertens* NOT child* OR adolescen*
|
Targeting hypertensive patients aged > 18
|
· Involved participants aged under 18 · Involved hypertensive patients with other cardiovascular diseases (i.e., heart failure, myocardial infarction) |
|
Intervention |
The intervention guided by SCT |
Social cognitive theory OR self-efficacy OR social support OR outcome expectation OR outcome expectations OR outcomes expectancy OR outcomes expectancies |
Intervention was guided by any of the constructs of SCT (self-efficacy, outcome expectations, or social support)
|
-
|
|
Comparison |
Control group |
intervent* |
Compared the outcomes between an intervention group and a control/comparison group |
Studies without a control group |
|
Outcomes |
Healthy lifestyles (PA and/or DA) |
Healthy lifestyle OR nutrition OR physical activity OR diet OR Diet [Mesh] OR exercis* OR Exercise[Mesh] |
Primary outcome of PA and/or DA |
Did not report the outcome change (PA or/and DA) |
|
Study design |
RCTs |
intervent* |
Randomised controlled trials (RCTs)
|
· Correlational study design · Secondary analysis · Protocol paper · Review study · Participants in either control or intervention < 10 |
Study Selection
Following the import of 446 references from the initial search into Covidence software and the removal of 122 duplicates, 330 remained. Two authors (WS and NP) independently screened the remaining titles and abstracts in accordance with the eligibility criteria. After excluding 311 studies that did not meet the inclusion criteria, both independent authors reviewed the full texts of the 19 remaining studies. Consensus between the two authors was used to settle disagreements about their findings. A PRISMA flow chart was used to present the search strategy (Figure 1).
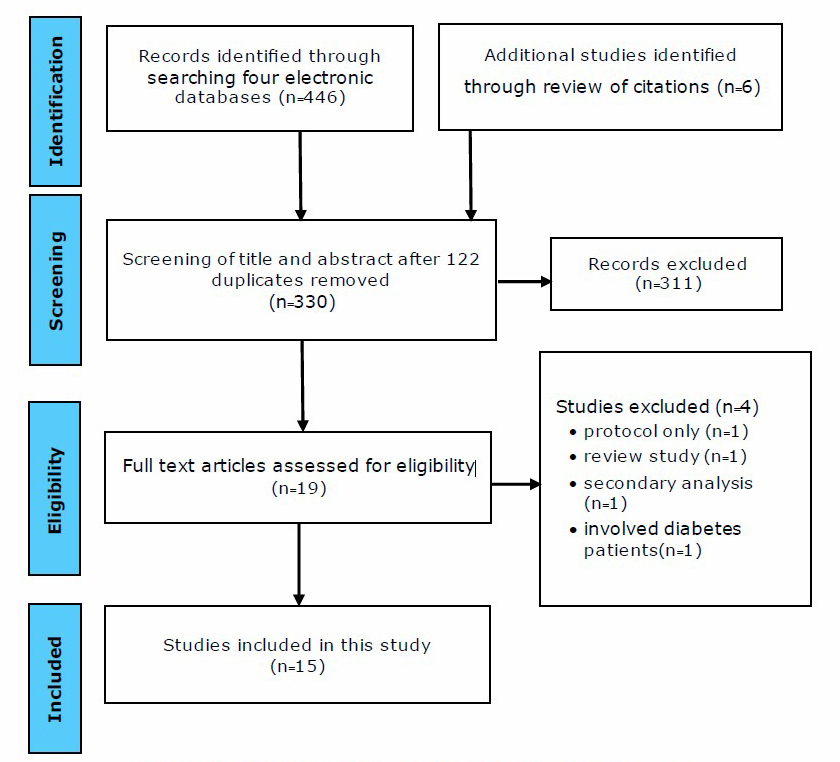
Figure 1. PRISMA Flow chart of the search process.
Data Extraction
The first author (WS) created a data extraction form based on the Consolidated Standards of Reporting Trials (CONSORT) checklist and checked the extracted data. The data extraction table was employed to present each study’s data, as follows: (1) author(s) and year of publication; (2) country; (3) sample size and characteristics of subjects; (4) intervention components; (5) duration of follow-up; (6) outcome measures; and (7) key findings, and how the SCT constructs were operationalized and evaluated. The second author (NP) independently verified the extracted data. Discrepancies were discussed until consensus was reached.
Quality Appraisal and Risk of Bias
The risk of bias for each potential study was assessed using the following six domains of the Cochrane Risk of Bias Tool for Randomized Control Trials (Higgins et al., 2019): (1) selection: randomly assign group; (2) performance; (3) detection; (4) attrition; (5) reporting; and (6) other biases. Risk of bias was classified into three categories: low risk, high risk, and insufficient information.
Data Synthesis
Narrative and tabulation synthesis were used to present the effect of the interventions guided by the construct of the SCT and to describe the main findings of the included studies.
RESULTS
Study Selection
A total of 446 records were found in the databases, and six additional studies were identified from reference lists of systematic reviews. After removing duplicates (n = 122), 330 studies guided by SCT and focused on improving healthy lifestyles (PA and/or DA) among hypertensive patients were identified. In the first step of study selection, the first and the second authors independently reviewed the titles and abstracts of the 330 remaining studies. The first and second authors then reviewed all decisions, discussed any discrepancies, and mutually agreed to include 19 studies. In the second step, the 19 full-text articles were independently read in their entirety and screened by the first and second authors. Discrepancies were resolved, and a consensus was reached between the first and second authors to exclude four of the 19 studies and retain 15. The details of the included 15-study is represented in Table 3. Figure 1 depicts a flow diagram of the search process from study identification to study selection for the review.
Risk of Bias Assessment
The assessment of risk of bias for the 15 independent studies is summarized in Table 2 using six quality indicators following categories from the Cochrane Collaboration tool: 1) random sequence generation, 2) allocation concealment, 3) blinding of participants/personnel, 4) blinding of outcome assessment, 5) incomplete outcome data, and 6) selective outcomes reporting (Higgins et al., 2019). The two independent review authors agreed-upon assessments regarding each risk of bias item are provided as percentages for each of the 15 studies, as noted in Figure 2. Numerous studies lacked sufficient details to permit assessment of the likelihood of bias, most notably with the random sequence generating method (n = 9, 60%), allocation concealment (n = 12, 80%), and outcome assessment blinding (n = 11, 73%). Only six studies (40%) explicitly stated the random sequence generation method, which involved a computer random number generator (Burke et al., 2008; Li et al., 2019; Mensorio et al., 2018; Schlenk et al., 2020); drawing of lots (Daniali et al., 2017); or sealed envelopes (Lee et al., 2007). Three studies conducted interventions in the same setting between two groups (intervention and control), increasing the risk of inadequate subject concealment (Daniali et al., 2017; Li et al., 2019; Meurer et al., 2019). The blinding of outcome assessment indicated that data collectors/interviewers in only three studies were blinded during the data collection procedure (Svetkey et al., 2005; Lee et al., 2007; Schlenk et al., 2020). The assessment of the risk of bias in completing outcome data showed almost all studies clearly reported the attrition rate or the reason for withdrawal of participants, which was reported to be < 20% of participants lost (n = 11, 73%).
|
Table 2. Quality indicators for assessing risk of bias (n=15) |
|||||||
|
No |
First Author (year) |
Random Sequence Generation |
Allocation Concealment |
Blinding of Participants/personnel |
Blinding of Outcome Assessment |
Incomplete Outcome Data |
Selective Outcomes Reporting |
|
1 |
Burke (2008) |
Yes (computer-generated random) |
Unclear |
Unclear |
No |
Unclear |
No |
|
2 |
Cornélio (2016) |
Unclear |
Unclear
|
No (Difference in study context) |
No
|
No |
No |
|
3 |
Daniali (2016) |
Yes (drawing lots) |
No (both groups conducted intervention at the same setting) |
Unclear |
No |
No |
No |
|
4 |
Farazian(2019) |
Unclear |
Yes |
Unclear |
No |
Unclear |
No |
|
5 |
Gallegos-Carrillo (2017) |
Unclear |
Unclear
|
No |
No |
Unclear |
No |
|
6 |
Gerage (2017) |
Unclear |
Unclear |
Unclear |
Yes |
No |
No |
|
7 |
Gómez-Pardo(2016) |
Unclear |
Unclear |
Unclear |
No |
No |
No |
|
8 |
Lee(2007) |
Yes (sealed envelopes) |
Yes |
Yes |
Yes (blinded interviewers) |
No |
No |
|
9 |
Li (2019) |
Yes (computer-generated random) |
No (both groups conducted intervention at the same setting) |
No |
No |
No |
No |
|
10 |
Mensorio (2019) |
Yes (computer-generated random) |
Unclear |
Unclear |
No |
No |
No |
|
11 |
Meurer (2019) |
Unclear |
No (both groups conducted intervention at the same setting) |
Unclear |
No |
No |
No |
|
12 |
Miao (2020) |
Unclear |
Unclear |
Unclear |
No |
Unclear |
Unclear |
|
13 |
Migneault (2012) |
Unclear |
Yes (different settings: online vs face to face)
|
Yes |
Unclear |
No |
No |
|
14 |
Schlenk (2020) |
Yes (computer-generated random) |
Unclear
|
Unclear |
Yes (blinded interviewers) |
No |
No |
|
15 |
Svetke (2005) |
Unclear |
Unclear |
Unclear |
Yes (blinded interviewers) |
No |
No |
Table 3. Intervention details, outcomes measures, and key findings (n=15)
|
First author (year) |
Country |
Sample |
IG: Intervention (component, intensity, duration)
|
CG intervention |
Duration/ follow-up |
Outcome measures |
Key findings |
|
Diet Adherence (DA) Outcome |
|||||||
|
Cornélio (2016) |
Brazil |
Participants: N = 92 Mean age: 59.9 Sex: Female 100% Duration of HTN: > 6 months |
Component: 1) Group discussion led by nurses: how to overcome barriers, 2) diet education: alternative ingredients (low salt), 3) verbal encouragement via phone call Intensity:12 sessions over 12 weeks Duration: 60-90 minutes |
Usual care |
12 weeks/none |
· Self-reported: using salt < 4 g. per day · 24-hour urinary sodium excretion |
· Significant decrease in salt consumption between two groups after intervention (d = .51), but not for the reduction in 24-hour urinary sodium excretion |
|
|
|
|
|
|
|
|
|
|
Svetke (2005) |
USA |
Participants: N = 304 Mean age: 52.0 Sex: Female 63.5 % Duration of HTN: > 6 months |
Component: 1) health education: DASH diet, 2) skill training (self-monitoring, goal-setting), 3) individual counselling, and 4) social support Intensity: 18 monthly face to face session over 18 months Duration: not reported |
Usual care: received a single 30-min individual advice session at the time of randomization |
18 months/6 months |
· 24-hr urine collection for excretion of sodium |
· Significant decrease in sodium excretion between two groups at follow-up (d = 0.21) |
|
Physical Activity (PA) Outcome |
|||||||
|
Burke (2008) |
Australia |
Participants: N = 241 Mean age: not reported Sex: Female 55.6 % Duration of HTN: > 3 months |
Component: 1) health education: costs and benefits of PA, 2) skills training: goal setting, time management, and 3) social support Intensity:16 sessions over 16 weeks Duration: not reported |
Usual care |
16 weeks/1 year |
· Self-recorded: hours per week spent in exercise of at least moderate intensity |
· Significant increase in time spent in PA among two groups after intervention (p = .04), but not for follow-up |
|
Gallegos-Carrillo (2017) |
Mexico |
Participants: N = 232 Mean age: 51.05 Sex: Female 70.3% Duration of HTN:< 5 years |
Component:1) health education: PA prescription based on the patient’s preferences and functional capacity, 2) group-based PA training (moderate intensity), 3) individual behavioral counseling to promote increased PA via fitness instructors Intensity: 16 educational sessions and 48 sessions of PA training over 16 weeks Duration: 1 hour group-based PA sessions, but not reported in educational sessions |
Usual care + health education: PA benefits, and 2) counselling session weekly (15 minutes/ patient) |
16 weeks/6 months |
· ActiGraph GT3X accelerometers |
· Significant increase in walking immediately after intervention (d = .26) and follow-up (d = .21) between two groups. · Leisure time PA was significantly different between two groups after intervention (d = .45) and follow-up (d = .41)
|
|
Lee (2007) |
Taiwan |
Participants: N = 184 Mean age: 71.3 Sex: Female 58.4 % Duration of HTN: not reported |
Component:1) health education: benefits of increased walking, ideas for overcoming perceived barriers (from others' experiences of success), and sharing practical information gleaned from others about pleasant walking routes and pedometer usage, 2) PA training (walking) Intensity: not reported Duration: not reported |
Usual care |
6 months/ none |
· Pedometer |
· 51.6% of participants in the intervention group reported more walking after the intervention than the control group (8.6%) |
|
Schlenk (2021) |
USA |
Participants: N = 182 Mean age: 64.7 Sex: Female 73.1 % Duration of HTN: Mean=13.78 year |
Component:1) health education: PA and hypertension management, 2) skill training (goal-setting, self-monitoring) Intensity: 6 weekly face to face educational sessions, and 9 biweekly telephone skill-training sessions over 6 months Duration:60-65 minutes for educational sessions, 15-20 minutes for telephone skill training sessions |
Usual care: health education according to the National Institute on Aging |
6 months/6 months |
· ActiGraph
|
· Significant increase in fitness walking between two group after intervention (d = 5.92) and follow-up (d = 5.54) |
|
DA and PA Outcome |
|||||||
|
Daniali (2016) |
Iran |
Participants: N = 146 Mean age: 53.12 Sex: Female 100% Duration of HTN: at least 6 mo. |
Component:1) health education: benefits of PA and DA, 2) skills training: goal-setting to maintain PA (low to moderate intensity) and DA (DASH diet), 3) verbal persuasion (sending SMS twice a week), 4) group-based PA training (aerobic exercise) Intensity: 6 educational (via face to face) and PA training sessions over 6 weeks Duration: 2-2.5 hours per session |
Usual care |
6 weeks/6 months
|
· 6-items Physical Activity Scale: stretching exercise, walking, swimming, use of sports equipment, and other aerobic exercise in the past week · 13-item The DASH Diet Questionnaire |
· Significant increase in PA at 6 weeks (d = .93) and at 6 months (d = .63) between two groups · DA was significantly greater for IG than CG at 6 weeks (d = .65), but increase was not maintained at 6 months (p = .28) |
|
Farazian (2019) |
Iran |
Participants: N = 60 Mean age: 60.65 Sex: Female 43.3% Duration of HTN: > 1 year |
Component:1) health education: DA and PA recommendation for BP control, 2) verbal persuasion (encourage patients to maintain their success in maintaining DA and PA via family), 3) group discussion between researcher, family, and patients about the barriers to maintaining PA and DA, 4) training self-monitoring skills (using a booklet) Intensity:4-week educational session weekly Duration: 45 minutes/session |
Usual care |
4 weeks/1 month |
· 29-item The Self-care Questionnaire for Hypertensive Patients: adherence to medication (3 items), low-salt diet (12 items), physical activity (2 items), smoking and alcohol use (2 items), and weight management (10 items). |
· Significant increase in PA immediately after intervention (d = .99) and follow-up (d = .99) for intervention group, compared to control group. · No significant between-group difference in DA immediately or after intervention (p = .11) |
|
Gerage (2017) |
Brazil |
Participants: N = 52 Mean age: 58.0 Sex: Female 48.1% Duration of HTN: > 3 months |
Component:1) health education: lifestyle changes (PA+DA), 2) skills training: time-management, problem-solving, goal-setting, and self-monitoring Intensity: 12 educational sessions over 12 weeks, Duration: 90 minutes educational session |
Usual care + education: 90 minutes about basic healthy recommendations for hypertensive patients (at the beginning of the intervention)
|
12 weeks/ none |
· ActiGraph GT3X accelerometers · The Brazilian Dietary Frequency Questionnaire |
· Significant increase in PA for intervention group at post-intervention (d = 0.29), as compared to control group. · Significant increase in DA at post intervention (d = 0.51) between two groups |
|
Gómez-Pardo (2016) |
Spain |
Participants: N = 543 Mean age: 42.1 Sex: Female 71 % Duration of HTN: not reported |
Component:1) health education via trained peer educators: physical, nutritional, and psychological aspects of lifestyle change, 2) Peer activity: discussion about diet control, and exercise engagement, brain storming. Intensity: monthly face to face meeting over 12 months Duration: each meeting took 60-90 minutes |
Usual care+ education about health and psychology professionals: motivation to change, physical activity, healthful diet, smoking cessation, stress management, and self-control of BP.
|
12 months/ 1 year |
· The standardized International Physical Activity Questionnaire (IPAQ) · The PREDIMED (Primary Prevention of Cardiovascular Disease with a Mediterranean Diet) |
· No significant between-group difference in PA or DA (p > .05). |
|
Li (2019) |
China |
Participants: N = 462 Mean age: 61.5 Sex: Female 63.4 % Duration of HTN: not reported |
Component:1) health education: common HTN problems, complication prevention, and healthy lifestyle, 2) discussion on WeChat application about the contents related to health education, 3) skill training: BP monitoring Intensity: 24 weekly educational and discussion chat sessions Duration: patients dependently spent their time reading the provided content over the 6 months, each weekly discussion chat lasted approximately 1 hour over 6 months |
Usual care + health lectures and one chronic disease follow-up every three months.
|
6 months/ none |
33-items The Hypertension Patients Self-Management Behavior Rating Scale (HPSMBRS): medication adherence (4 items), condition monitoring (4 items), diet management (10 items), exercise management (3 items), work–rest management (5 items), and emotion management (7 items) |
· Significant increase in DA between two groups at post intervention (Adjusted mean difference = 4.2) · No significant improvement of PA between two groups at post intervention (p = .389)
|
|
Mensorio (2019) |
Spain |
Participants: N = 106 Mean age: 53.1 Sex: Female 44.3 % Duration of HTN: not reported |
Component:1) health education: healthy lifestyle change, and 2) skill training: self-observation, self-instruction, behavioral recording, stimulus control, self-reinforcement, problem-solving, and homework Intensity: 8 sessions (web-based): 3 educational sessions (weekly sessions), 5 skill-training sessions every two weeks Duration: not reported |
Usual care+ medical consultations focused on reducing cardiovascular risk factors.
|
3 months/ 12 months |
· Dutch Eating Behaviours Questionnaire (DEBQ) · IPAQ |
· Significant increase in PA between two groups after intervention (d = .44) but no difference at follow-up · Significant increase in DA between two groups after intervention (d = .09) and follow-up (d = 0.15)
|
|
Meure (2019) |
Brazil |
Participants: N = 291 Mean age: 62 Sex: Female 90.7 % Duration of HTN: not reported |
Component: 1) health education: healthy lifestyles change, 2) skill training: self-monitoring and goal-setting for healthy lifestyle changes, 3) group discussion about identification of social support, such as friends and family who could support the change or PA barriers, and 4) PA training (aerobic exercise) Intensity:12 weeks with 12 sessions (face to face) Duration: 60 minutes/session |
Usual care + health education |
3 months/none |
· ActiGraph · Self-reported: dietary habits (daily meals, time devoted to eating, and dietary intake) |
· Significant increase in MVPA between two groups after intervention (d = .32) · IG had higher consumption of vegetables than CG (p < .01)
|
|
Miao (2020) |
China |
Participants: N = 156 Mean age: 67.4 Sex: Female 52.3 % Duration of HTN: not reported |
Component: home visiting education: self-care management, skills training: goal-setting and self-monitoring Intensity: bi-weekly session of home visits over 16 weeks Duration: 60 minutes per session |
Usual care + health education leaflets |
16 weeks/none |
· Self-care Behaviors |
· Significant increase in PA and salt restriction between two groups after intervention (p < .001) |
|
Migneault (2012)
|
USA |
Participants: N = 337 Mean age: 56.3 Sex: Female 70.3 % Duration of HTN: > a year |
Component: 1) health education: diet and PA recommendation, 2) instrumental support (pedometer and digital weight scale), and 3) deliver automated telephone counseling messages. Intensity:32 educational sessions via telephone Duration: 20-minute educational session via telephone over 32 weeks |
Usual care |
8 months/12 months |
· 7-day physical activity recall · The picture-sort Food Frequency Questionnaire |
· Significant difference in change of diet quality scores between groups after intervention (p < .01) · No significant difference between groups in leisure time or MVPA after intervention |
Note: HTN = Hypertension; IG = Intervention group; CG = Control group

Figure 2. Risk of bias graph: Review of authors’ judgments about each risk of bias item presented as percentages across the 15 included studies.
Overall Study Characteristics
Of the 15 reviewed RCT studies, most were conducted in the U.S. (n = 3, 20%) and Brazil (n=3, 20%), followed by China (n = 2, 13%); Spain (n = 2, 13%); Iran (n = 2, 13%); and Australia, Mexico, and Taiwan (n = 1 per country). The sample sizes ranged from 52 (Gerage et al., 2017) to 543 participants (Gomez-Pardo et al., 2016). The total 3,388 hypertensive patients' ages ranged from 18–88 years with a mean age of 52.21; about 68.70% of patients were female. Five studies (26%) recruited newly diagnosed patients (duration of hypertension < 1 year) (Svetkey et al., 2005; Burke et al., 2008; Cornelio et al., 2016; Daniali et al., 2017; Gerage et al., 2017). The duration of hypertensive diagnosis ranged from 3 months (Burke et al., 2008) to 16 years (Schlenk et al., 2020). Study outcomes included DA and PA together (n = 9, 60%), PA only (n = 4, 27%), and DA only (n = 2, 13%).
DA Outcome
Two RCTs targeted DA alone (13%). Hypertensive patients’ DA referred to their adherence to a low-sodium diet. Both DA-only interventions used the objective measure of 24-hr urine collections for excretion of sodium to assess DA, while one of the two studies also measured DA using a self-reported questionnaire. A total of 396 hypertensive patients were included, with 81.75% being female. The two studies (Svetkey et al., 2005; Cornelio et al., 2016) reported a moderate effect on decreasing salt and/or increasing vegetable and fruit consumption between intervention and control groups (d = .21–.51). The intervention components differed across the two studies, but both included face-to-face DA education and social support from family or healthcare professionals. Other components of the studies included: 1) skills training: self-monitoring and attainable goal-setting (Svetkey et al., 2005); 2) individual counseling (Svetkey et al., 2005); and 3) verbal encouragement (Cornelio et al., 2016). The intervention lasted 12 weeks (Cornelio et al., 2016) to 18 months (Svetkey et al., 2005), and intervention frequency ranged from once a week (Cornelio et al., 2016) to once a month (Svetkey et al., 2005). When reported, intervention periods lasted between 60 and 90 minutes (Cornelio et al., 2016).
PA Outcomes
Four RCTs targeted PA alone (27%) with a total of 839 hypertensive patients. Their mean age was 61.43, and 63.68% were female. Time since diagnosis, which was reported in three studies, ranged from three months to 18 years (Burke et al., 2008; Gallegos-Carrillo et al., 2017; Schlenk et al., 2020). In the four studies assessing PA, outcomes such as moderate to vigorous physical activity (MVPA, n = 3, 75%) and leisure physical activity (LPA, n = 1, 25%) were measured. To assess MVPA, three studies utilized objective measures (ActiGraph GT3X accelerometers) (Gallegos-Carrillo et al., 2017; Schlenk et al., 2020), or pedometers (Lee et al., 2007), while a remaining study used a self-reported questionnaire (Burke et al., 2008). The duration of intervention ranged from 16 to 24 weeks, with an average of 12 weeks. Interventions were delivered once a week to three days a week, with the majority occurring at least once a week. All four RCTs included face-to-face PA education as the intervention component. However, other intervention components that differed across these four RCTs included: 1) skills training [attainable goal-setting] (Burke et al., 2008; Schlenk et al., 2020), self-monitoring (Schlenk et al., 2020), and time management (Burke et al., 2008); 3) PA training in the group or individually (Lee et al., 2007; Gallegos-Carrillo et al., 2017); 4) individual PA counseling (Gallegos-Carrillo et al., 2017); and 5) social support (Burke et al., 2008).
Effect sizes for PA change, when the behavior was assessed using an objective measure (ActiGraph GT3X accelerometers), were reported in two studies (d = .26–.59). An intervention including PA skill training (i.e., attainable goal-setting, self-monitoring) within PA educational sessions had a larger effect size on PA improvement (d = .59: (Schlenk et al., 2020)) than an intervention focusing only on PA educational sessions (d = .26; (Gallegos-Carrillo et al., 2017)) after the intervention was completed and at long-term follow up (6 months after intervention had ended). However, one nonsignificant finding in PA improvement at follow-up (1 year) among hypertensive patients was presented using a self-reported questionnaire with a single item: hours per week spent in PA (Burke et al., 2008).
DA and PA Outcomes
Nine RCTs targeted both DA and PA (60%). DA was defined as hypertensive adherence to a low-sodium and/or low-fat diet using a self-reported questionnaire, whereas PA was operationalized as MVPA and LPA measured by objective measures (ActiGraph GT3X accelerometers) and a self-reported questionnaire. The nine studies included a total of 2,153 hypertensive participants with a mean age of 55.2; 69.89% were female. Four of the nine studies (44%) reported time since diagnosis that ranged from 3 months to one year (Migneault et al., 2012; Daniali et al., 2017; Gerage et al., 2017; Farazian et al., 2019). The most frequently used intervention duration was 12 weeks (n = 3, 33%) (Gerage et al., 2017; Mensorio et al., 2018; Meurer et al., 2019), and interventions ranged from 4 weeks (Farazian et al., 2019) to 1 year (Gomez-Pardo et al., 2016) with an average of 20.28 weeks. Frequency of intervention delivery varied with most being offered once a week (n = 6, 67%), followed by once a month (n = 2, 22%) and two days a week (n = 1, 11%). When reported, intervention periods ranged from 20 minutes (Migneault et al., 2012) to 150 minutes (Daniali et al., 2017), with 58.88 minutes being the average. All nine RCTs included health education in DA and PA as the intervention component, while most of them (67%) consisted of skills training for maintaining DA and PA: self-monitoring (Gerage et al., 2017; Mensorio et al., 2018; Farazian et al., 2019; Meurer et al., 2019; Miao et al., 2020), attainable goal setting (Daniali et al., 2017; Gerage et al., 2017; Meurer et al., 2019; Miao et al., 2020), time management (Gerage et al., 2017), and problem-solving (Gerage et al., 2017; Mensorio et al., 2018). Other intervention components were included: 1) verbal encouragement (Daniali et al., 2017; Farazian et al., 2019); 2) group-based PA training (Daniali et al., 2017); 3) group discussion: overcoming any barriers to maintain PA or DA (Farazian et al., 2019; Gomez-Pardo et al., 2016; Li et al., 2019; Meurer et al., 2019); 4) instrumental support (Migneault et al., 2012); and 5) individual counseling (Migneault et al., 2012).
Six studies noted a significant increase in PA after the intervention (d = .29–.99), while three studies, all of which provided < 60 minutes of the intervention and monthly contact, showed no significant PA change (P > .05). Three of the six studies provided one-month, six-month, and 12-month follow-up measures following the intervention. The likelihood of improved PA change after intervention and follow-up did not significantly increase based on the intervention's duration, time period, or frequency. For instance, a study with 150 minutes intervention periods provided once a week over six weeks reported a similar effect size (d = .93) (Daniali et al., 2017) compared to a study with 45-minute intervention periods delivered on a shorter time frame (4 weeks) and frequency (once a week) (d = .99) (Farazian et al., 2019). However, the strength that the effect size had on PA change was different according to the intervention component. Two studies with high effect size on PA improvement (d > .93–.99) applied group discussion to identify the PA barriers (Farazian et al., 2019) and PA skills training (Daniali et al., 2017) into their intervention components.
Seven of nine interventions examining the effect of the intervention on DA improvement resulted in a significant increase in DA (d = .09–.65). Overall, these significant findings were reported using self-reported questionnaires. To be effective in improving DA, an intervention duration of at least six to 32 weeks was needed. However, it is essential to note that the intervention's duration, session frequency, and session time period have a different effect on DA change among hypertensive patients. An extended session time period of 150 minutes for the intervention (Daniali et al., 2017) had a greater effect size on DA improvement (d = .65) than an intervention session lasting 60–90 minutes (d = .09-.51) (Gerage et al., 2017; Mensorio et al., 2018). In contrast, nonsignificant increases in DA were found in a study with a 4-week intervention duration (Farazian et al., 2019) and in another study with a low frequency of intervention sessions: monthly meeting with participants (Gomez-Pardo et al., 2016).
Theoretical framework
Table 4 illustrates the operationalization of SCT constructs among 15 studies. Six studies (40%) applied SCT alone to guide the interventions (Gomez-Pardo et al., 2016; Daniali et al., 2017; Gallegos-Carrillo et al., 2017; Gerage et al., 2017; Mensorio et al., 2018; Schlenk et al., 2020). Three studies (20%) were based on Bandura's self-efficacy theory alone (Lee et al., 2007; Farazian et al., 2019; Li et al., 2019). In addition, SCT was combined with the Transtheoretical Model (Svetkey et al., 2005; Burke et al., 2008; Migneault et al., 2012; Cornelio et al., 2016; Meurer et al., 2019), Theory of Planned Behavior (Burke et al., 2008), Health Belief Model (Burke et al., 2008), and Motivational Interviewing (Migneault et al., 2012). The most assessed construct of SCT was self-efficacy (n = 10, 90%); followed by social support (n = 7, 63%), and outcome expectancies (n = 1, 9%) respectively.
In DA-only interventions, self-efficacy was commonly operationalized. DA education (Cornelio et al., 2016) and skills development (self-monitoring and goal-setting) (Svetkey et al., 2005) were used to increase self-efficacy: mastery experience or participants' confidence or ability to successfully achieve their DA. In one study, social support was operationalized as emotional support (encouragement or concern) provided by a clinical psychologist to assist participants in maintaining their DA (Svetkey et al., 2005). No study operationalized outcome expectancies.
In PA-only interventions, self-monitoring was frequently operationalized to increase self-efficacy (Lee et al., 2007; Schlenk et al., 2020). For example, participants used a pedometer (Lee et al., 2007) or accelerometer (Schlenk et al., 2020) to track their step count or PA level and then recorded it in their log for self-monitoring of their PA behavior. Three studies operationalized social support (Burke et al., 2008; Gallegos-Carrillo et al., 2017; Schlenk et al., 2020); however, only one study detailed how social support was operationalized (Gallegos-Carrillo et al., 2017). No study operationalized outcome expectancies.
In interventions involving multiple behaviors, goal-setting (Gomez-Pardo et al., 2016; Daniali et al., 2017; Gerage et al., 2017; Meurer et al., 2019) was regularly operationalized. Generally, goal-setting was operationalized by having participants record their success in PA or DA in a diary log/handbook record to evaluate their PA and DA achievement goals. Only one study used the SMART technique (specific, measurable, attainable, reasonable, and with specific timeframes) to assist participants in establishing an attainable goal for DA and PA improvement (Daniali et al., 2017). Three studies operationalized social support in terms of informational (Gomez-Pardo et al., 2016), instrumental (Migneault et al., 2012), and companionship support (Gerage et al., 2017); however, one study was unable to provide a clear description of how social support was operationalized in the intervention (Meurer et al., 2019).
Table 4. Social cognitive theory constructs operationalized
|
Study |
Theoretical basis |
Operationalization of SCT constructs |
How SCT constructs were operationalized |
Construct measures |
Key findings |
|
Diet Adherence (DA) Outcome |
|||||
|
Cornélio (2016) |
SCT and TTM |
self-efficacy: mastery experience, identification of barriers, and verbal persuasion |
- Each participant received instruction in how to prepare a meal using a low-salt diet cookbook; how to use a spoon to measure the amount of salt (develop mastery experience); and how to identify cooking barriers through group discussion using the cookbook. - During the reinforcement telephone calls, the verbal persuasion technique was used. |
Self-efficacy in performing low-salt diet with 5-items |
The IG significantly increased their self-efficacy to use less than 4 g of salt per day when cooking compared to the CG |
|
Svetkey (2015) |
SCT and TTM |
self-monitoring, goal-setting, social support |
- Participants were encouraged to set an attainable goal for achieving DA: weight loss of approximately 15 lbs. over a six-month period, dietary sodium intake of no more than 100 mmol/day and use of a DA log to track their sodium diet intake. - A clinical psychologist provided emotional support to the participants in order to maintain their DA. |
Not reported |
Not reported |
|
Physical Activity (PA) Outcome |
|||||
|
Burke (2008) |
SCT, TTM, TPB, and HBM |
self-efficacy: mastery experience, identification of PA barriers, goal setting, time management and social support. |
- Participants were educated in person about the benefits of PA for controlling blood pressure (mastery experience). - Participants were encouraged to identify barriers to engaging in PA and work with the PA counselor to develop strategies for overcoming PA barriers. - Goal setting, time management and social support was not described in detail. |
- Self-efficacy for diet and physical activity developed by Plotnikoff and Higginbotham - Social support developed by Thoits: support from friends, relatives, spouses, and co-workers |
Significant increase in self-efficacy for dietary change between two groups after intervention (d = 20.055) and at follow-up (d = 0.054) |
|
Gallegos-Carrillo (2017) |
SCT |
self-efficacy: mastery experience; vicarious learning; verbal encouragement, social support |
- Participants received education about the benefits of PA and advice on how to increase PA levels safely and gradually, as well as training to perform MVPA in a group setting (mastery experience). - Participants received individual counseling (15 minutes/patient) to encourage them to maintain their PA (verbal encouragement). - Participants were encouraged to participate in MVPA with their family or peers, as desired. |
- Social support developed by Sallis et al: assessed the level of support from family and friends that study participants perceived. - Self-efficacy during leisure time, walking, and planned PA developed by Fernández-Cabrera: assessed with a questionnaire previously developed. |
Significant increase in self-efficacy between two groups after intervention (p < .001) |
|
Lee (2007) |
Bandura’s self-efficacy theory |
self-efficacy: mastery experience; vicarious learning; verbal encouragement; emotional state/ physiological feedback, self-monitoring |
- The intervention strategy incorporated four sources of self-efficacy, the majority of which were obtained through dialogue with a public health nurse. These included identifying performance accomplishments; vicarious learning from successful others and the public health nurse; and recognizing positive and challenging negative interpretations of physiological and emotional responses to walking. - Self-monitoring was operationalized by having participants record their daily steps in their PA log using a pedometer. |
Self-Efficacy for Exercise Scale developed by Resnick and Jenkins: 9-items |
Significant increase in the mean of self-efficacy between two groups after intervention (mean difference 1.3, 95% CI = 0.5 to 2.0, p = 0.001) |
|
Schlenk (2021) |
SCT |
self-efficacy: mastery experience; vicarious learning; verbal encouragement; emotional state/ physiological feedback, outcome expectancy, goal setting, self-monitoring, social support |
- Self-monitoring and setting DA and PA (150 min/week) goals were operationalized by using a 7-day e-diary log and by wearing an accelerometer. - Outcome expectations in PA were conducted by a registered nurse over the phone (15-20 minutes) to help participants visualize their health outcomes after intervention and encourage them to perform their PA. - Self-efficacy strategies (mastery, modeling, verbal persuasion, and physiological feedback) were incorporated into all intervention sessions, which included: 1) learning about OA and hypertension, 2) getting started with fitness walking, 3) being physically active while in pain, 4) using hot and cold compression to reduce pain after walking, 5) dealing with unpleasant sensations, 6) avoiding risks associated with PA, 7) utilizing peer support, and 8) using self-talk to regain control over pain. |
- Self-efficacy to perform behaviors to self-manage pain: 11-items - Outcome Expectation in Perceived Therapeutic Efficacy (PTE) Scale: 10 items with an 11-point Likert scale
|
Nonsignificant increase in self-efficacy (p = .365) and outcome expectancy (p = .12) between two groups after intervention and follow-up |
|
DA and PA Outcome |
|||||
|
Daniali (2016) |
SCT |
goal-setting, self-efficacy: mastery experience |
Goal setting based on SMART goals (specific, measurable, achievable, realistic, and time-related) was used to help participants increase their self-efficacy and set their goals to achieve their DA and PA goals. |
Self-efficacy scale developed by Lorig: 6 items with a 10-point Likert scale |
Significant increase in self-efficacy between two groups after intervention (p < .001) and follow-up (p = .005) |
|
Farazian (2019) |
Bandura’s self-efficacy theory |
self-efficacy: mastery experience; vicarious learning; verbal encouragement; emotional state/ physiological feedback |
The intervention strategy included four sources of self-efficacy which were primarily delivered through lecture and discussion with the interventionist. These were the following: set attainable goals to maintain PA or DA that are easier to accomplish; vicarious learning from two patients' successful experiences in disease control; verbal encouragement from the researcher via phone call; and patients were given a worksheet of achievable personal goals to stimulate them and reduce the impact of failure experiences. |
Not reported |
Not reported |
|
Gerage (2017) |
SCT |
self-efficacy: mastery experience, social support, goal-setting |
- PA/DA education and goal-setting was used to enhance the achievement to maintain healthy habits (build mastery experience). - Identified the main sources of support from peers or family to help them sustain DA and PA |
- The Self- Efficacy for Exercise Scale (18 items) - Self-Efficacy for Eating Habits (30 items) - Social Support for Physical Activity with 6 items |
Only perception of social support was significantly changed between two groups after intervention (p > .05) |
|
Gómez-Pardo (2016) |
SCT |
social support: informational support, self-efficacy: mastery experience, self-monitoring, goal-setting |
- Peers who were trained about healthy lifestyle changes by healthcare providers delivered knowledge and skill to participants (social support: informational support). - Identified the barriers to maintaining healthy lifestyles and reducing cardiovascular risk through group discussion; used this to enhance self-efficacy (mastery experience) and shared their success in maintaining a healthy lifestyle from their own experience (vicarious experience). - Used a health handbook to record the participants’ lifestyle behavior, health parameters, and immediate goals at each meeting. |
Not reported |
Not reported |
|
Li (2019) |
Bandura’s self-efficacy theory |
self-efficacy: mastery experience; verbal encouragement; emotional state/ physiological feedback |
All Web-based intervention sessions included self-efficacy strategies (mastery, modeling, verbal persuasion, and physiological feedback): 1) established a goal for maintaining PA and DA; 2) received verbal encouragement via phone call from a registered nurse; 3) gained knowledge from peers about how to maintain healthy habits; and 4) developed the ability to manage emotions. |
The Hypertension Self-Efficacy Scale with 15-items |
Self-efficacy did not differ between the two groups after intervention (p = .086) |
|
Mensorio (2019) |
SCT |
self-efficacy: mastery experience |
The intervention strategy included mastery experience to increase self-efficacy through education about what a healthy lifestyle involves and learning techniques on how to achieve it on a day-to-day basis. |
Self-Efficacy Questionnaire General (GSES-12) with 10 items |
Nonsignificant increase in self-efficacy between two groups after intervention and follow-up (p > .05) |
|
Meure (2019) |
SCT and TTM |
self-efficacy: mastery experience; vicarious experience, goal setting, self-monitoring, social support, outcome expectancies |
- Participants were provided individual feedback for their monitoring of healthy habits to increase their confidence to maintain healthy habits (mastery experience). - Self-monitoring of DA and PA was accomplished through the use of pedometers and written records, resulting in self-motivated and guided action to accomplish predetermined goals (goal setting), identification of social support: such as friends and family members who could assist with the changes, and identification of individual barriers, outcome expectations, confronting changes in PA, and dietary habits. The meetings were held in conversation circles, which enable group members to reflect on, debate, and share their experiences with a subject (informational support and vicarious learning). |
Not reported |
Not reported |
|
Miao (2020) |
Bandura’s self-efficacy theory and the Chronic Care Model |
self-efficacy |
Participants learned self-management for hypertension control through illustrated, simple educational booklets to increase their ability and confidence in self-care behaviors: DA and PA. |
Not reported |
Significant increase in self-efficacy between two groups after intervention (p = .015) |
|
Migneault (2012)
|
SCT, MI, and TTM |
self-efficacy: mastery experience, self-monitoring, social support: tangible/instrumental support |
- The intervention provided a foundation for health education and skill development in order to boost participants' confidence in performing healthy habits via phone. - Instrumental support was provided in the form of a pedometer and a digital weight scale to assist participants in evaluating (self-monitoring). - Self-monitoring was operationalized by having participants record their daily steps in their PA log using a pedometer. |
Not reported |
Not reported |
Note: SCT: Social Cognitive Theory; TTM: Transtheoretical Model; HBM: Health Belief Model; MI: Motivational Interviewing; TPB: Theory of Plan Behavior
DISCUSSION
The purposes of this systematic review were to synthesize current SCT-based literature on DA and/or PA interventions for hypertensive patients and to describe effective ways for assisting hypertensive patients in sustaining their healthy lifestyles. The findings of this review suggest that SCT-based interventions were successful in improving hypertensive patients' DA and/or PA. The effect size between .26–.59 for PA-only interventions can be interpreted as small to medium. These values were similar to other systematic reviews of SCT-based interventions among obese populations (Olander et al., 2013; Young et al., 2014) and cancer patients (Stacey et al., 2015) that focused on a single health behavior outcome (PA) (d = 0.33–.54) (Stacey et al., 2015). However, the limited number of SCT-based interventions targeting DA-only change made it difficult to compare its effectiveness to other studies.
This systematic review showed that the ideal duration for PA-only interventions is at least 16 weeks including 16 contacts with participants lasting 60–90 minutes per session for PA improvement. This finding was consistent with a previous systematic review of 48 PA-RCTs in obese populations, which concluded that 12-week interventions with at least 12 contacts were recommended to maximize the intervention's effect on improving PA in both the short (> 6 months) and long term (> 12 months) (Samdal et al., 2017). When the intervention targeted DA and PA together, the multiple-behavior interventions had a longer duration (average 20.28 weeks) and more time spent per session (150 minutes per session) than DA- or PA-only interventions. This finding was consistent with a previous review, which showed a positive relationship between the intensity of intervention (duration, number of contacts with participants) and DA plus PA improvement in patients with type 2 diabetes (Greaves et al., 2011). Thus, it is essential to note that the intervention intensity (i.e., duration, time spent, and contact) should be increased in proportion to the outcome measured. Due to the limitation of DA-only interventions studies (n = 2), the relationship between intervention intensity (duration or duration of the intervention) and DA improvement remains unclear.
Based on effect size, a multiple-behavior intervention (DA and PA) had a stronger effect than a single-behavior intervention, including DA or PA alone as the outcome. Similarly, a systematic review conducted in healthy adult populations reported that PA effects were strongest in multiple-behavior interventions, including tobacco cessation and healthy diet eating, compared to single-behavior interventions (Prochaska and Prochaska, 2011). Moreover, prior research conducted among 400 adults with a high cardiovascular disease risk reported that increasing regular PA was associated with higher healthy eating behaviors (low-fat and low-salt diets) (P < .05) (Pavicic Zezelj et al., 2019). Possibly, an increase in one healthy behavior may be associated with improvement in overall health behavior.
Prior systematic reviews targeting SCT-based interventions and DA and/or PA reported that two main components, health education and skill training, effectively enhanced PA and/or DA for cancer patients (Stacey et al., 2015) or healthy elderly (Young et al., 2014). Additionally, education and skill training should be regarded as potential components of behavioral change interventions that might assist individuals in overcoming barriers and performing/maintaining behavior over time (Arlinghaus and Johnston, 2018). When comparing the effect sizes of PA improvement between PA-only interventions that had single or multiple components, interventions with higher effect sizes had multiple intervention components, such as PA skill training (self-monitoring in PA) and identification of PA barriers through group discussion. Likewise, a systematic review on RCTs for promoting PA among European adolescents found that a multiple-component intervention, including education and discussion of PA barriers with family/peers, generally resulted in larger effect sizes than a single component intervention with PA education only (Crutzen, 2010). Furthermore, a systematic evaluation of PA interventions among obese participants (Mage = 49.1) indicated that interventions that included self-monitoring had a higher effect size on PA improvement (d = .804), compared to those that did not (d = .524) (Olander et al., 2013). However, the limited number of studies implementing a DA-only intervention precludes comparing the effect size of DA change between these studies' intervention components (n = 2).
Within the SCT construct, self-efficacy was frequently operationalized in SCT, but other constructs (outcome expectancies, social support) were rarely operationalized as an intervention component. Attainable goal-setting and self-monitoring were commonly operationalized and used to enhance self-efficacy resulting in DA and/or PA change. Recent systematic reviews found that self-efficacy, self-monitoring of behavior, and goal-setting were all associated with DA and PA improvement among certain populations, including cancer and diabetes patients (Greaves et al., 2011; Stacey et al., 2015).
Strengths and Limitations
This review has strengths and limitations. A strength is that it provides significant evidence to support the effect of DA and/or PA change interventions based on SCT for hypertensive patients and offers suggestions for effective intervention design. Second, it describes how SCT constructs were operationalized in hypertensive patients' DA and/or PA interventions, which is an important step towards determining exactly what and how to intervene to contribute to intervention success or failure. Furthermore, this comprehensive search did not exclude existing studies based on publication year and participants' characteristics such as age or gender. However, there are some limitations of this review. First, the search was limited to studies published in the English language, which may limit the ability to generalize the findings to other groups, such as Asians, who reside in countries in which English is not the predominant language. Second, operationalizing outcome expectancies was difficult due to the limitations of the included studies. Lastly, most interventions included samples with more females and with durations of hypertension greater than one year, which reduces the generalizability of the findings to hypertensive males and patients who are within their first year of having hypertension. Lastly, utilizing meta-analysis to examine the pooling effect of SCT-based interventions on healthy lifestyle change is recommended as a future study to provide more solid evidence.
Implications
This systematic review found that SCT-based interventions can significantly improve DA and PA of hypertensive patients. Single or multiple-behavior interventions applying skills development (i.e., self-monitoring, goal-setting) demonstrated significant PA change with medium effect size after the intervention and at follow-up. Thus, skill development may be a critical component for improving DA and/or PA in intervention. Multiple-behavior (DA and PA) interventions resulted in greater improvement in DA and PA outcomes than single-behavior interventions. Multiple-behavior interventions tended to have a longer duration (at least 6 weeks) and higher time spent per session (150 minutes per session) than single-behavior interventions. Thus, to achieve the anticipated DA and PA increase, longer duration and greater time spent in each session of a multiple-behavior intervention may be necessary to achieve a significant change in DA and PA.
CONCLUSION
SCT-based interventions have been found to be beneficial in promoting DA and/or PA among hypertensive patients. However, as demonstrated in this systematic review, DA and/or PA interventions may be more effective if the intervention includes skill development (i.e., attainable goal-setting, self-monitoring) to improve self-efficacy as the main SCT construct. The extent to which theoretical constructs are applied and evaluated in future SCT-based interventions should be provided in order to determine the components of SCT-based interventions that are effective.
ACKNOWLEDGEMENTS
The authors wish to express their gratitude to Dr. Lorraine B. Robbins for her insightful comments on the final draft and to Jessica Sender for her assistance with the search strategy. Additionally, we would like to express our appreciation to the publication center of Chiang Mai University's faculty of nursing for proofreading this work.
AUTHOR CONTRIBUTIONS
Wachira Suriyawong: Conceptualization, Formal analysis, Investigation, Writing – Original draft, Writing – Review & Editing, Visualization, Project administration Noppamas Pipatpiboon: Investigation. All authors have read and approved the final draft of this manuscript.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
REFERENCES
Abraham, C., and Michie, S. 2008. A taxonomy of behavior change techniques used in interventions. Health Psychol. 27: 379-387.
American Heart Association [AHA]. 2021. Heart disease and stroke statistics—2021 update. Circulation. 2021;143:e254–e743
Arksey, H., and O'Malley, L. 2005. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology. 8:19-32.
Arlinghaus, K.R., and Johnston, C.A. 2018. Advocating for behavior change with education. American Journal of Lifestyle Medicine. 12:113-116.
Bandura, A. 1987. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: PrenticeHall.
Bandura, A. 1998. Health promotion from the perspective of social cognitive theory. Psychology and Health. 13: 623-649.
Bond Brill, J. 2011. Lifestyle intervention strategies for the prevention and treatment of hypertension: A review. American Journal of Lifestyle Medicine. 5: 346-360.
Burke, V., Beilin, L.J., Cutt, H.E., Mansour, J., and Mori, T.A. 2008. Moderators and mediators of behaviour change in a lifestyle program for treated hypertensives: A randomized controlled trial (adapt). Health Education Research. 23: 583-591.
Cohen, S., Underwood, L. G., & Gottlieb, B. H. 2000. Social support measurement and intervention: A guide for health and social scientists. Oxford University Press.
Conceicao, L.S., Neto, M.G., do Amaral, M.A., Martins-Filho, P.R., and Oliveira Carvalho, V. 2016. Effect of dance therapy on blood pressure and exercise capacity of individuals with hypertension: A systematic review and meta-analysis. International Journal of Cardiology. 220: 553-557.
Cornelio, M.E., Godin, G., Rodrigues, R.C., de Freitas Agondi, R., Alexandre, N.M., and Gallani, M.C. 2016. Effect of a behavioral intervention of the saldavel program to reduce salt intake among hypertensive women: A randomized controlled pilot study. European Journal of Cardiovascular Nursing. 15: e85-94.
Cornelissen, V.A. and Smart, N.A. 2013. Exercise training for blood pressure: A systematic review and meta-analysis. Journal of the American Heart Association. 2: e004473.
Crutzen, R. 2010. Adding effect sizes to a systematic review on interventions for promoting physical activity among european teenagers. International Journal of Behavioral Nutrition and Physical Activity. 7: 29.
Daniali, S.S., Eslami, A.A., Maracy, M.R., Shahabi, J., and Mostafavi-Darani, F. 2017. The impact of educational intervention on self-care behaviors in overweight hypertensive women: A randomized control trial. ARYA Atheroscler. 13: 20-28.
Farazian, F., Emami Moghadam, Z., Heshmati Navabi, F., and Behnam Vashani, H. 2019. Effect of self-care education designed based on bandura's self-efficacy model on patients with hypertension: A randomized clinical trial. Evidence Based Care. 9.
Filippou, C.D., Tsioufis, C.P., Thomopoulos, C.G., Mihas, C.C., Dimitriadis, K.S., Sotiropoulou, L.I., Chrysochoou, C.A., Nihoyannopoulos, P.I., and Tousoulis, D.M. 2020. Dietary approaches to stop hypertension (dash) diet and blood pressure reduction in adults with and without hypertension: A systematic review and meta-analysis of randomized controlled trials. Advances in Nutrition. 11: 1150-1160.
Gallegos-Carrillo, K., Garcia-Pena, C., Salmeron, J., Salgado-de-Snyder, N., and Lobelo, F. 2017. Brief counseling and exercise referral scheme: A pragmatic trial in mexico. American Journal of Preventive Medicine. 52: 249-259.
Gay, H.C., Rao, S.G., Vaccarino, V., and Ali, M.K. 2016. Effects of different dietary interventions on blood pressure: Systematic review and meta-analysis of randomized controlled trials. Hypertension. 67: 733-739.
Gerage, A.M., Benedetti, T.R.B., Ritti-Dias, R.M., Dos Santos, A.C.O., de Souza, B.C.C., and Almeida, F.A. 2017. Effectiveness of a behavior change program on physical activity and eating habits in patients with hypertension: A randomized controlled trial. Journal of physical activity and health. 14: 943-952.
Glanz, K. and Bishop, D.B. 2010. The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health. 31: 399-418.
Gomez-Pardo, E., Fernandez-Alvira, J.M., Vilanova, M., Haro, D., Martinez, R., Carvajal, I., Carral, V., Rodriguez, C., de Miguel, M., Bodega, P. et al. 2016. A comprehensive lifestyle peer group-based intervention on cardiovascular risk factors: The randomized controlled fifty-fifty program. Journal of the American College of Cardiology. 67: 476-485.
Greaves, C.J., Sheppard, K.E., Abraham, C., Hardeman, W., Roden, M., Evans, P.H., Schwarz, P., and Group, I.S. 2011. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 11: 119.
Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., and Welch, V.A. 2019. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons.
Lee, L.L., Arthur, A., and Avis, M. 2007. Evaluating a community-based walking intervention for hypertensive older people in taiwan: A randomized controlled trial. Preventive Medicine. 44: 160-166.
Li, X., Li, T., Chen, J., Xie, Y., An, X., Lv, Y., and Lin, A. 2019. A wechat-based self-management intervention for community middle-aged and elderly adults with hypertension in guangzhou, china: A cluster-randomized controlled trial. International Journal of Environmental Research and Public Health. 16.
Mbambo, S. W., Tlou, B., & Dlungwane, T. P. 2019. Factors associated with physical activity amongst patients with hypertension in two community health centres in Mgungundlovu health district, KwaZulu-Natal, 2018. South African Family Practice. 61: 234-238.
Mensorio, M., Cebolla, A., Rodilla, E., Palomar, G., Lison, J.F., Botella, C., Fernández-Aranda, F., Jimenez-Murcia, S., and Baños, R. 2018. Analysis of the efficacy of an internet-based self-administered intervention (“living better”) to promote healthy habits in a population with obesity and hypertension: An exploratory randomized controlled trial. International Journal of Medical Informatics. 124.
Meurer, S.T., Lopes, A.C.S., Almeida, F.A., Mendonca, R.D., and Benedetti, T.R.B. 2019. Effectiveness of the vamos strategy for increasing physical activity and healthy dietary habits: A randomized controlled community trial. Health Education and Behavior. 46: 406-416.
Miao, J.H., Wang, H.S., and Liu, N. 2020. The evaluation of a nurse-led hypertension management model in an urban community healthcare: A randomized controlled trial. Medicine (Baltimore). 99: e20967.
Migneault, J.P., Dedier, J.J., Wright, J.A., Heeren, T., Campbell, M.K., Morisky, D.E., Rudd, P., and Friedman, R.H. 2012. A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive african-americans: A randomized controlled trial. Annals of Behavioral Medicine. 43: 62-73.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D.G., and Group, P. 2009. Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. PLOS Medicine, 6: e1000097.
Olander, E.K., Fletcher, H., Williams, S., Atkinson, L., Turner, A., and French, D.P. 2013. What are the most effective techniques in changing obese individuals' physical activity self-efficacy and behaviour: A systematic review and meta-analysis. International Journal of Behavioral Nutrition and Physical Activity. 10: 29.
Pavicic Zezelj, S., Kendel Jovanovic, G., and Kresic, G. 2019. The association between the mediterranean diet and high physical activity among the working population in croatia. Medycyna Pracy. 70: 169-176.
Prochaska, J.J., and Prochaska, J.O. 2011. A review of multiple health behavior change interventions for primary prevention. American Journal of Lifestyle Medicine. 5.
Resnick, B. 2013. Self-efficacy. In S. J. Peterson & T. S. Bredow (Eds.), Middle range theories: Application to Nursing Research (3rd ed., pp. 82-95). Philadelphia, PA:Wolters Kluwer Health.
Samdal, G.B., Eide, G.E., Barth, T., Williams, G., and Meland, E. 2017. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. International Journal of Behavioral Nutrition and Physical Activity. 14: 42.
Saneei, P., Salehi-Abargouei, A., Esmaillzadeh, A., and Azadbakht, L. 2014. Influence of dietary approaches to stop hypertension (dash) diet on blood pressure: A systematic review and meta-analysis on randomized controlled trials. Nutrition, Metabolism and Cardiovascular Diseases. 24: 1253-1261.
Semlitsch, T., Jeitler, K., Hemkens, L.G., Horvath, K., Nagele, E., Schuermann, C., Pignitter, N., Herrmann, K.H., Waffenschmidt, S., and Siebenhofer, A. 2013. Increasing physical activity for the treatment of hypertension: A systematic review and meta-analysis. Sports Medicine. 43: 1009-1023.
Schlenk, E.A., Fitzgerald, G.K., Rogers, J.C., Kwoh, C.K., and Sereika, S.M. 2020. Promoting physical activity in older adults with knee osteoarthritis and hypertension: A randomized controlled trial. Journal of Aging and Physical Activity. 29: 207-218.
Sherbourne, C. D., & Stewart, A. L. 1991. The MOS social support survey. Social Science & Medicine (1982). 32: 705–714.
Stacey, F.G., James, E.L., Chapman, K., Courneya, K.S., and Lubans, D.R. 2015. A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. Journal of Cancer Survivorship. 9: 305-338.
Svetkey, L.P., Erlinger, T.P., Vollmer, W.M., Feldstein, A., Cooper, L.S., Appel, L.J., Ard, J.D., Elmer, P.J., Harsha, D., and Stevens, V.J. 2005. Effect of lifestyle modifications on blood pressure by race, sex, hypertension status, and age. Journal of Human Hypertension. 19: 21-31.
Young, M.D., Plotnikoff, R.C., Collins, C.E., Callister, R., and Morgan, P.J. 2014. Social cognitive theory and physical activity: A systematic review and meta-analysis. Obesity Reviews. 15: 983-995.
OPEN access freely available online
Chiang Mai University Journal of Natural Sciences [ISSN 16851994]
Chiang Mai University, Thailand
https://cmuj.cmu.ac.th
Wachira Suriyawong and Noppamas Pipatpiboon
Department of Public Health, Faculty of Nursing, Chiang Mai University, Chiang Mai, 50200
Corresponding author: Wachira Suriyawong, E-mail: Wachira.s@cmu.ac.th
Total Article Views
Editor: Veerasak Punyapornwithaya
Chiang Mai University, Thailand
Article history:
Received: February 8, 2022;
Revised: April 18, 2022;
Accepted: April 18, 2022;
Published online: April 27, 2022

