
Effect of Different Resin Cements on Shear Bond Strength between Acrylic Denture Teeth and Resin Composite
Jirat Srihatajati and Pattarawadee Krassanairawiwong*Published Date : 2022-01-21
DOI : https://doi.org/10.12982/CMUJNS.2022.011
Journal Issues : Number 1, January-March 2022
Abstract The purpose of this study was to evaluate the effect of different bonding agents and resin cements on shear bond strength (SBS) between acrylic resin teeth and resin composite. Thirty acrylic teeth were cut along the long axis and embedded in cold-cure acrylic resin. The specimens were randomly divided into 3 groups (n = 10) according to the types of luting agents: Group C (OptiBond FL), Group P (Panavia F2.0), and Group S (Superbond C&B). SBS was measured using the Shimadzu EZ-S Universal Testing Machine. The collected data were analyzed using a one-way ANOVA to determine significant differences with P-value < 0.05. Multiple comparisons of SBS were calculated using the Tukey HSD test at a 95% confidence level. The average SBS values in MPa were 5.78 ± 0.97 for Group C, 13.60 ± 1.20 for Group P, and 17.93 ± 1.24 for Group S. The SBS value for Group S was significantly higher compared to the other groups, while the value for Group C was significantly lower. Group C was categorized as an adhesive failure, while Group S was accounted as a cohesive failure and Group P was shown to be a mixed failure. In conclusion, different resin cements significantly affected the SBS between acrylic resin teeth and resin composite.
Keywords: Acrylic denture tooth, Bonding agent, Resin cement, Resin composite, Shear bond strength
Funding: The authors are grateful for the research funding provided by the College of Dental Medicine, Rangsit University, Thailand.
Citation: Srihatajati, J. and Krassanairawiwong, P. 2021. Effect of different resin cements on shear bond strength between acrylic denture teeth and resin composite. CMU J. Nat. Sci. 21(1): e2022011.
INTRODUCTION
Prosthodontists recognize the need for artificial denture teeth to replace missing natural teeth. (Jyoti et al., 2014). Artificial teeth restore patients’ esthetic, phonic, and masticatory functions. Acrylic resin artificial teeth are widely used due to their realistic form, variety of shades, sufficient hardness, modification ease, and satisfying bonding capacity to acrylic denture base materials (Anusavice and Phillips, 2003). However, they are often criticized for their inefficiency, such as the rapid wearing of the occlusal surfaces, which may cause a change in centric occlusion and vertical dimension leading to temporomandibular joint disturbance and decreased chewing ability (Ghazal and Kern, 1997). Fractured or debonded acrylic denture teeth present a common clinical problem, accounting for 20-33% of denture repairs (Cunningham, 1993). Factors leading to the fragmentation of acrylic teeth include excessively strong bite force or accidental trauma. The repair procedure is commonly time-consuming; therefore, it is crucial to locate required materials that match the original material in strength and color as well as to use repair techniques that are easy, quick, and inexpensive. In general, an immediate in-office repair using auto-cured acrylic resin has inferior color stability, and the usage of heat-cured acrylic resin requires time-consuming laboratory procedures.
Some published studies suggested repairing fractured or debonded denture teeth by visible light-cured composites in the clinic immediately after the incident (Stameisen and Ruffino, 1987). Using resin composite is popular due to its time-saving procedures. Additionally, resin composite has been used to either build up or modify the facial forms of artificial acrylic denture teeth to harmonize the adjoining natural teeth and improve the patient’s facial characteristics (Weiner et al., 1987). In certain cases, resin composite has been used to remodel abraded anatomical artificial posterior teeth to enhance the masticatory function. The success rate of the direct repair technique, such as filling fractures, mainly depends on the resin composite’s adhesion to the acrylic resin artificial teeth (Vergani et al., 1987). Several techniques have been studied to improve the surface bonding of acrylic resin, including forms of mechanical retention such as air abrasion, retention grooves, or box form etching (Cardash et al., 1990). Chemical bonds such as methyl methacrylate monomer (MMA), silane coupling agent, and other bonding agents have also been investigated (Vallittu et al., 1997; Meng et al., 2010; Chatterjee et al., 2011).
However, in some cases, the repair process becomes more complicated, such as when modifying the color of acrylic artificial anterior teeth with indirect composite veneers to improve esthetics. In this process, the first step is to prepare the restorations from the patient’s denture. In the second visit, the prepared veneers are attached to the acrylic denture teeth in a short amount of time. The advantages of this process is that the patient does not have to make multiple visits and leave without a denture. This method also considers esthetics because the resin composite is available in a variety of colors. In some cases, the worn occlusal surfaces of posterior artificial teeth must be repaired; such wear can decrease masticatory efficiency and lead to loss of vertical dimension. Repairs using indirect overlay composite restorations can be done within one visit (Vergani et al., 1987).
An important component of repairs is bond strength. Chalkley et al. (1980) showed that the bond strength between acrylic laminates and resin composites was limited, supported by the finding that the site of failure usually occurred at this interface. Since then, research has investigated methods to increase the bonding force between resin composites and laminates in denture teeth (Chalkey et al., 1980). Boyer and Chalkley, (1982) found a way to enhance the bond strength between acrylic laminates and resin composites by penetrating the acrylic surface with solvent cement. Greater bonding strength could be obtained by applying a liner that was made by mixing acrylic powder and monomer, due to the molecular weight or degree of cross-linking of the liner (Boyer and Chalkley, 1982). Additionally, cementation with adhesive was recognized as a crucial step to enhance the retention of indirect restorations (Vargas et al., 2011).
Resin cements are classified as adhesive cement due to their ability to bond to different substances, such as dentin and enamel, porcelain and other ceramics, gold and other metal alloys, indirect resin composite restorations, and acrylic resins (Caneppele et al., 2010). In addition to retention capacity, resin cements have high tensile strength, high compressive strength, and low solubility (Ferracane et al., 2011; Van, 2002). Despite their importance, there are limited studies about the optimal methods to achieve good adhesion between contaminated polymerized acrylic resins and indirect resin composite restoration by luting cements. The purpose of this study was to observe the effect of different bonding agents and resin cements including OptiBond FL, Panavia F2.0, and Superbond C&B on shear bond strength (SBS) between acrylic resin teeth and resin composite. The null hypothesis was that using different resin cements had no significant effect on SBS between acrylic denture teeth and resin composite.
MATERIALS AND METHODS
Specimen preparation
Acrylic resin artificial maxillary right central incisor teeth (New Ace Anterior, shade A3, Mold S8, Yamahachi Dental Mfg. Co., USA) were placed in silicone mold in labiopalatal manner, exposing 2 mm labial surface to control the depth of the teeth. A marker was used to mark the cut plane prior to the cutting process. The acrylic denture teeth were cut along the long axis by a low-speed diamond saw with underwater cooling (IsoMet 1000; Buehler, Lake Bluff, IL, USA). Each was embedded in cold-cure acrylic resin (Formatray, Kerr Dental Corp., Orange, CA, USA) in a polyvinylchloride ring (diameter 21.4 mm). The surfaces of specimens were polished with wet 600-grit silicon carbide grinding paper by a polishing machine (DPS 3200; Imtech, South Africa) for 15 seconds to establish uniform flat bonding surfaces, then were rinsed with water for 30 seconds and left to dry under ambient laboratory conditions for 24 hours (Figure 1). The specimens were immersed in distilled water at 37°C for 30 days to mimic the environment of the human oral cavity. The specimens were randomly divided into 3 experimental groups, and each group (n = 10) was bonded using different materials.
For the preparation of the resin composite blocks, the resin composite (Filtek TM Z350 XT Universal restorative, shade A1, 3M ESPE, USA) was condensed through the center hole of a cylindrical metal mold 3 mm in diameter and 3 mm in height into two increments. Each layer (1.5 mm.) was cured by a light-curing unit (Astralis 3, Ivoclar Vivadent, Liechtenstein) with a wavelength of 450-470 nm for 40 seconds.
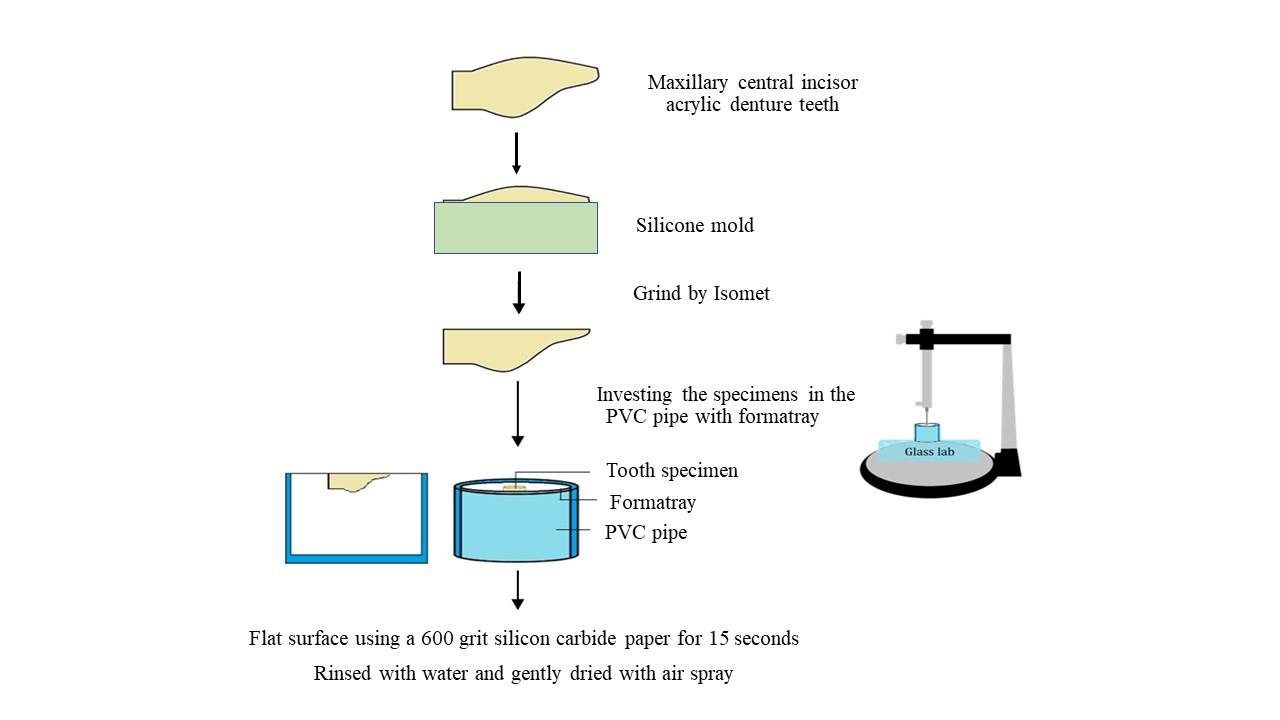
Figure 1. The acrylic denture tooth surface preparation.
Surface preparation
Group C (control group): The metal mold was put on top of a PVC pipe and MMA (Unifast Trad liquid, GC Dental Product Corp., Aichi., Japan) was applied on the surfaces of the specimens for 180 seconds then primed with the OptiBond FL and cured by light for 20 seconds. The resin composite was condensed against teeth surfaces through the mold in two increments (1.5 mm each), and each layer was light-cured for 40 seconds.
Group S: According to the manufacturer’s recommendation, the acrylic resin teeth surfaces were etched with a red activator for 30 seconds, rinsed with water for 15 seconds, dried for 10 seconds, and then treated with MMA for 180 seconds. The metal mold was put on top of the specimen, then the mixed Superbond C&B was applied on the surface and the composite block was located in the metal mold’s hole. A load of 1000 g was placed on the composite block for 180 seconds.
Group P: The acrylic resin teeth surfaces were treated with MMA for 180 seconds then they were luted with Panavia F2.0. The process was carried out according to the manufacturer’s recommendation. The resin composite blocks were located in the hole. A load of 1000 g was placed on the composite block for 180 seconds then cured by light for 40 seconds. The chemical compositions of the bonding agent and resin cements used in this study were shown in table 1.
Table 1. Bonding agent: Resin cements used in this study and their compositions.
|
Material |
Composition |
Manufacturer |
|
OptiBond FL Lot no: 7552090 |
Bis-GMA, HEMA, GDMA, CQ, ODMAB, filler (fumed SiO2, barium aluminoborosilicate, Na2SiF6), coupling factor A174 (approximately 48 wt% filled) |
Kerr Corp., Orange, CA, USA |
|
Panavia F2.0 Lot no: 00058 |
ED Primer II Liquid A: 10 methacryloyloxydecyl dihydrogen phosphate (10-MDP), 2-hydroxyethyl methacrylate
ED Primer II Liquid B: N-Mehacryloyl-5-aminosalicylic acid, catalysts
Paste A:10-methacryloyloxydecyl dihydrogen phosphate, hydrophobic, catalysts, initiators
Paste B: sodium treated glass powder, substituted dimethacrylate
|
Kuraray Medical Inc., Okayama., Japan |
|
Superbond C&B Lot no: ST1 |
Powder: polymethyl methacrylate (PMMA)
Liquid: 4-methacryloyloxylethyl trimellitate anhydride (4-META), methyl methacrylate (MMA)
Red activator: 65% phosphoric acid
Green activator: 10% citric acid, 3%ferric chloride |
Sun Medical, Moriyama., Japan |
The shear bond strength test
Following complete polymerization, the bonded specimens were immersed in distilled water in an incubator (Contherm Scientific Ltd., New Zealand) at 37°C for 24 hours before the experiment was conducted. The SBS test was performed by a universal testing machine (EZ-S, Shimadzu, Japan) with a knife-edge shear testing apparatus. The samples were secured in a horizontal position with the assistance of a metal fixture. A metal blade with 0.25 mm thickness was moved vertically at a cross-head with a speed of 0.5 mm/min to break the bonding surfaces at the tooth and composite interface. The maximum load at the break for each specimen was divided by the bonding area (mm2) to express the bond strength (MPa).
Surface morphologic examination
After the SBS test, the fractured acrylic teeth surfaces were inspected visually with SEM (JSM-5410LV; JEOL, Tokyo, Japan) at 1000X magnification to classify the mode of failure into three categories. Adhesive failure indicated that the debonding occurred between the acrylic resin and the resin cement. Cohesive failure indicated that the debonding occurred in the acrylic resin tooth or resin cement. If the debonding occurred due to both adhesive and cohesive failure in the same specimen, it was classified as a mixed failure.
RESULTS
The Kolmogorov-Smirnov test was used to assess the distribution of experimental results and showed that the data of each group had a normal distribution (P > 0.05). A one-way ANOVA and the Tukey HSD test were used to analyze the results at a confidence level of 95%. The results from the one-way ANOVA showed that the mean SBS between acrylic denture teeth and resin composite was significantly influenced by different resin cements or at least the mean SBS of one group was different from the other groups significantly (P < 0.05) (Table 2).
Table 2. One-way ANOVA results for the shear bond strength among studied groups shows that the significance equal 0.000 or the significant < 0.05 (P – value < 0.05) which illustrates that the average population of at least one group is different from the average of other groups of the population.
|
|
Sum of Squares |
df |
Mean Square |
F |
Sig.* |
|
Between Groups |
757.238 |
2 |
378.619 |
288.931 |
0.000 |
|
Within Groups |
35.381 |
27 |
1.310 |
|
|
|
Total |
792.619 |
29 |
|
|
|
Note: Sum of squares = summation of the squares of the differences from the mean.
df =degree of freedom = the maximum number of values that have the freedom to vary in the sample data.
Mean square = an estimator of variance obtained by dividing the sum of square by the degree of freedom. F= an analysis to find out whether or not the means between two populations are significantly different. Sig.*= statistical significant (P-value < 0.05)
The mean values of the groups were compared using the Tukey HSD test. The results showed that the SBS values of Group C, Group S, and Group P were significantly different among each other (P < 0.05). The SBS value of Group S was found to be the highest (17.93 ± 1.24 MPa), followed by Group P (13.60 ± 1.20 MPa), the lowest, however, was found in Group C (5.78 ± 0.97 MPa). The mean values of the SBS and standard deviations for the experimental groups are illustrated in Figure 2.
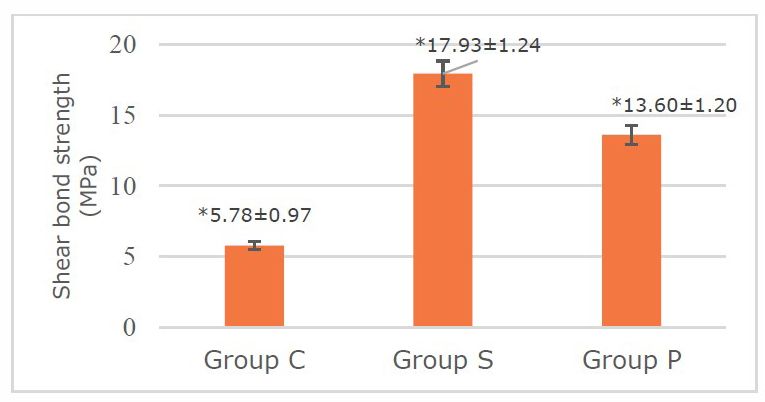
Figure 2. Means and standard deviations of shear bond strength between acrylic resin denture teeth and resin composite using OptiBond FL, Superbond C&B, and Panavia F2.0, respectively. Indicates a significant difference between group (P < 0.05).
The surfaces of acrylic denture teeth observed with SEM at 1000X magnification showed that Group S had the highest surface roughness, followed by group P and group C, respectively. Group C showed the smoothest surface with a small amount of OptiBond FL remained on the surface. Group S showed the highest surface roughness with Superbond C&B covering almost the entire surface of acrylic denture teeth. While Group P with the second highest surface roughness revealed Panavia F2.0 remaining on the surface. This could be implied that the ability to bond Superbond C&B with acrylic denture teeth was superior to other groups. For the classification of the mode of failure by evaluating the resin cement left on the acrylic tooth surface. If resin cement left on the acrylic surface was less than 25%, the sample will be classified as an adhesive failure since that the failure occurred between the acrylic tooth and the bonding agent. If the resin cement left covers 75% of the acrylic surface, it will be classified as a cohesive failure as a result of the failure within the bonding material. If the resin cement left covers between 25% - 75% of the acrylic surface, This specimen will be classified as mixed failure (Moule et al.,2007). So the result of this experiment showed that the mode of failure for all specimens in group C was adhesive failure between the acrylic denture teeth and resin cement. All specimens in Group S demonstrated cohesive failure in adhesive resin cement, while all specimens in Group P showed a mixture of adhesive and cohesive failure (Figure 3).
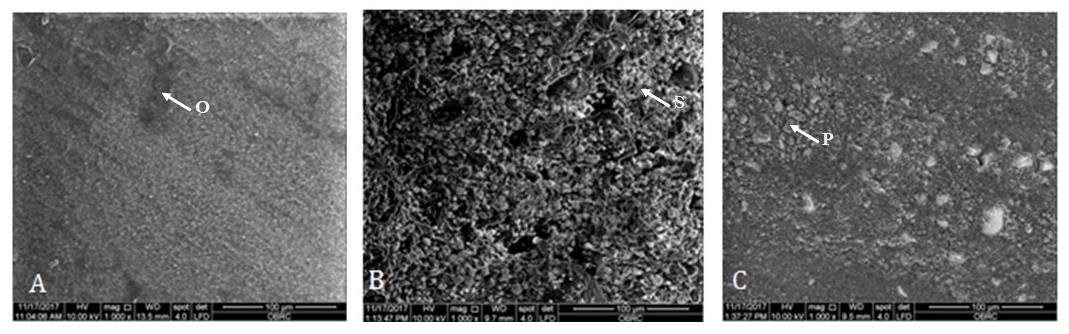
Figure 3. The morphology of the deboned acrylic resin teeth surfaces using SEM at 1000X magnification. (A) Deboned surfaces of acrylic resin denture tooth using OptiBond FL. The O arrow in the figure shows the bonding agent remaining on the surface. (B) Deboned surfaces of acrylic resin denture tooth using Superbond C&B. The S arrow in the figure shows the resin cement cover almost all parts of the acrylic denture surface. (C) Deboned surfaces of acrylic resin denture tooth using Panavia F 2.0. The P arrow in the figure shows the resin cement cover on the acrylic tooth surface more than (A) but less than (B).
DISCUSSION
Experimental results demonstrated significant differences in the SBS between acrylic denture teeth and resin composite when luting with OptiBond FL, Panavia F2.0, and Superbond C&B. All the bonding regimens employed in this study showed a positive effect on SBS values. Superbond C&B showed the highest bond strength value compared with OptiBond FL and Panavia F2.0. Advancements in bonding technology likely contribute to the high success rate of the indirect restoration repair process. Our results support previous studies which found that different resin cements possessed different bonding abilities, particularly that Superbond C&B (total-etch resin cement) was a luting agent that provided the highest SBS in several situations (Nakabayashi et al., 1982; Stamacos and Simon, 2013).
The main components of acrylic denture teeth are polymethyl methacrylate (PMMA) and polyethyl methacrylate (PEMA) in a cross-linked polymer matrix. The degree of modification in these materials is relatively high due to the manufacturer’s hot processing or cross-linking methods (Lagouvardos and Polyzois, 2003). MMA diffuses into the acrylic denture tooth and leads to the swelling of acrylic resin polymer (Vallittu et al., 1997). This process allows the composite to penetrate surface microirregularities and form a mechanical bond (Papazoglous and Vasilas, 1999). Wetting the heat polymerized acrylic resin surface with MMA for 180 seconds has been suggested to dissolve the surface structure of PMMA and turn the polymer into a form of gel. As a result, free double bonds will copolymerize with the composite material and create a cross-linking mechanism, which in turn enhances the chemical bonding between composite and acrylic resin. (Chatterjee et al., 2011).
One of the OptiBond FL components (Table 2) is Bis-GMA. Guzman and Moore (1995) used a Bis-GMA-based bonding agent to increase micromechanical retention between the matrix and exposed filler particles in order to improve the bond strength between the acrylic resin and composite. Muhsin (2017) showed that using MMA with a suitable bonding agent produced greater bonding between acrylic resin and composite than MMA alone.
Two characteristics of Superbond C&B resin may have resulted in its superior bond strength in this experiment. First, Superbond C&B is a total-etch resin cement that uses phosphoric acid to etch dentin and enamel. The etching procedure removes the smear layer, causing the dentinal tubules to open. After this process, the adhesive resin cement is applied to the preparation; this material infiltrates the porosities, acting as a resin tag. The polymerization process of the hybrid layer bonds the cement to the tooth. Superbond C&B contains 4-META (4-Methacryloxyethyl trimellitate anhydride), which promotes the diffusion of monomers into the tooth structure and polymerizes with the MMA to form a co-polymer known as a hybrid layer (resin-impregnated layer) (Nakabayashi et al., 1982). In this experiment, the phosphoric acid cleaned the smear layer and eroded inorganic substances that were part of the acrylic resin compositions, forming microporosities, and implying increased mechanical retention as shown by Lagouvardos and Polyzois (2003). Second, Superbond C&B bonds well to acrylic resins because they possess similar basic structures, namely MMA and PMMA. By contrast, the molecular form of Bis-GMA, which is the main component of OptiBond FL, is larger than the PMMA molecule, decreasing its penetrating ability through the irregular surface of PMMA. The SEM results of Group S showed cohesive failure in the adhesive resin, which could imply that the bonding between the acrylic denture tooth and the adhesive resin was stronger than the bond strength in the resin cement itself.
Panavia F2.0 is self-etch resin cement; its main primer component is 10-MDP (10-Methacryloyloxydecyldihydrogen phosphate), which chemically bonds to the oxide layer of other dental materials, for example, base metal alloys, zirconia, or resin composites. This substance plays an important role in enhancing the bond strength of acrylic resin and composite to dental alloys and titanium (Amaral et al., 2014). The double bonds of the phosphoric acid group of MDP co-polymerize with the resin monomers while the other side chemically bonds with metal atoms. (Bulbul and Kesim, 2010). In particular, MDP is clinically accepted as a bonding heat-cure acrylic resin to titanium (Kim et al., 2009). Correspondingly, the obtained results confirmed that Panavia F2.0 with MDP showed stronger SBS between the acrylic tooth and resin composite than OptiBond FL. The primer of Panavia F2.0 combines a weak acid and a binder which can be applied to the tooth surface without rinsing. The primer dissolves the smear layer, the solvent penetrates through the intertubular dentine, and then a decalcifying process occurred. This mechanism that impregnates the smear layer for bonding is known as the self-etch technique (Amaral et al., 2010). The phenomenon occurs in dentin or enamel; however, in the case of acrylic resin, it did not provide an irregularity on the acrylic teeth surfaces, so there was no effect on the mechanical retention of the acrylic tooth to the adhesive resin in the experiment. This account is supported by the SEM results of Group P, which showed the mode of failure to be mixed, in contrast to the mode of failure in Group S, which was cohesive.
While the SBS value of Group P was significantly lower than Group S, it was dramatically higher than the value of Group C. The SEM of Group C showed adhesive failure, indicating that the bonding between the acrylic resin tooth surface and resin composite was inferior to either bonding in the acrylic tooth or bonding agent itself. Overall, the null hypothesis was rejected, as different resin cements significantly affected SBS between acrylic denture teeth and the resin composite.
CONCLUSION
Within the limits of the experiment, the results can be concluded that bonding with different types of resin cements significantly affected the SBS between acrylic resin teeth and the visible light-cure composite. Superbond C&B showed a significantly higher shear bond strength value than Panavia F2.0 and Panavia F2.0 showed a significantly higher value than OptiBond FL. According to the SEM of the acrylic teeth bonded surfaces, it can be implied that the mode of failure corresponding to the SBS value of each group. In conclusion, Superbond C&B has the highest ability to bond acrylic denture teeth with resin composite compare to Panavia F2.0 and OptiBond FL.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the group of students at the College of Dental Medicine, Rangsit University for helping with the data collection and Miss Rawissada Krassanairawiwong for providing great language help during writing the manuscript.
AUTHOR CONTRIBUTIONS
Jirat Srihatajati and Pattarawadee Krassanairawiwong designed and conducted all of the experiments, performed the statistical analysis and wrote the manuscript. All authors have read and approved of the final manuscript.
CONFLICT OF INTEREST
The authors declare that they hold no competing interests.
REFERENCES
Amaral, M., Belli, R., Cesar, PF., Valandro, LF., Petschelt, A., and Lohbauer, U. 2014. The Potential of novel primers and universal adhesives to bond to zirconia. Journal of Dentistry. 42: 90-98.
Amaral, RC., Stanislawczuk, R., Zander-Grande, C., Gagler, D., Reis, A., and Loguercio, AD. 2010. Bond strength and quality of hybrid layer of one-step self-etch adhesives applied with agitation on dentin. Operative Dentistry. 35: 211-219.
Anusavice, KJ. and Phillips, RW. 2003. Phillip’science of dental material. 11th ed. St Louis; Elsvier Science. 733.
Boyer, D.B. and Chalkley, Y. 1982. Bonding between acrylic laminates and composite resin. Journal of Dental Research. 61: 489-492.
Bulbul, M. and Kesim, B. 2010. The effect of primers on shear bond strength of acrylic resin to different types of metals. Journal of Prosthetic Dentistry. 103: 303-308.
Caneppele, TM., Zogheib, LV., Gomes, I., Kuwana, AS., and Pagani, C. 2010. Bond strength of a composite resin to an adhesive luting cement. Brazilian Dental Journal. 21: 322-326.
Cardash, HS., Applebaum, B., Baharav, H., and Liberman, R. 1990. Effect of retention grooves on tooth-denture base bond. Journal of Prosthetic Dentistry. 64: 492-496.
Chalkley, Y., Boyer, D.B., Johnson, W. 1980. Bond Strength between plastic laminates and restorative resins. AADRProgr and Abst. 1980. No. 635.
Chatterjee, N., Gupta, TK., and Banerjee, A. 2011. A study on effect of surface treatments on the shear bond strength between composite resin and acrylic resin denture teeth. Journal of Indian Prosthodontic Society. 11: 20–25.
Cunningham, J.L. 1993. Bond strength of denture teeth to acrylic bases. Journal of Dentistry. 21: 274–280.
Ferracane, JL., Stansbury, J.W., and Burke, JT. 2011. Self-adhesive resin cements - chemistry, properties and clinical considerations. Journal of Oral Rehabilitatio. 38: 295-314.
Ghazal, M. and Kern, M. 2010. Wear of denture teeth and their human enamel antagonists. Quintessence International. 41: 157-163.
Guzman, A. and Moore, BK. 1995. Influence of surface treatment on bond strength between a heat-activated and a light-activated resin composite. International Journal of Prosthodontics. 8: 179-186.
Jyoti, R.K., and Seshan, S. 2014. Microhardness Evaluation of Nano- Composite Denture Teeth. International Journal of Current Research and Review. 6: 58-61.
Kim, SS., Vang, MS., Yang, HS., Park, SW. and Lim, HP. 2009. Effect of adhesive primers on bonding strength of heat cure denture base resin to cast titanium and cobalt-chromium alloy. Journal of Advanced Prosthodontics. 1: 41-46.
Lagouvardos, PE. and Polyzois GL. 2003. Shear bond strength between composite resin and denture teeth: effect of tooth type and surface treatments. International Journal of Prosthodontics. 16: 499-504.
Meng, GK., Chung, K-H., Fletcher-Stark, ML., and Zhang, H. 2010. Effect of surface treatments and cyclic loading on the bond strength of acrylic resin denture teeth with autopolymerized repair acrylic resin. Journal of Prosthetic Dentistry. 103: 245-252.
Moule C., Angelis F., G.-H. Kim et al. 2007. Resin bonding using an all-etch or self-etch adhesive to enamel after carbamide peroxide and/or CPP-ACP treatment. Aus Dent J. 52: 133–137.
Muhsin, S.A. 2017. Bond strength of repaired acrylic denture teeth using visible light cure composite resin. Open Dentistry Journal. 11, 57-64.
Nakabayashi, N., Kojima, K., and Masuhara, E. 1982. The promotion of adhesion by infiltration of monomers into tooth substrates. Journal of Biomedical Materials Research. 16, 265-73.
Papazoglous, E. and Vasilas, AI. 1999. Shear bond strength between composite and autopolymerized acrylic resin bonded to acrylic resin denture teeth. Journal of Prosthetic Dentistry. 82: 573-578.
Stamacos, C. and Simon, JF. 2013. Cementation of indirect restoration: an overview of resin cements. Compendium of Continuing Education in Dentistry. 34: 42-46.
Stameisen, A.E. and Ruffino, A. 1987. Replacement of lost or broken denture teeth with composites. Journal of Prosthetic Dentistry. 58: 119–120.
Vallittu, PK., Ruyter, IE., and Nat, R. 1997. The swelling phenomenon of acrylic resin polymer teeth at the interface with denture base polymers. Journal of Prosthetic Dentistry. 78: 194-9.
Van, Noort, R. 2002. Introduction to dental materials. 2nd ed. St. Louis, MO: Mosby. 257-278.
Vargas, MA., Bergeron, C., and Diaz-Arnold, A. 2011. Cementing all-ceramic restorations: recommendations for success. Journal of the American Dental Association. 142SuppI 2, 20S-4S.
Vergani, C.E., Giampaolo, E.T., and Cucci, A.L. 1997. Composite occlusal surfaces for acrylic resin denture teeth. Journal of Prosthetic Dentistry. 77: 328–331.
Weiner, S., Krause, A.S., and Nicholas, W. 1987. Esthetic modification of removable partial denture teeth with light-cured composites. Journal of Prosthetic Dentistry. 57: 381–384.
OPEN access freely available online
Chiang Mai University Journal of Natural Sciences [ISSN 16851994]
Chiang Mai University, Thailand
https://cmuj.cmu.ac.th
Jirat Srihatajati and Pattarawadee Krassanairawiwong*
College of Dental Medicine, Rangsit University, Pathumthani 12000, Thailand
Corresponding author: Pattarawadee Krassanairawiwong, E-mail: pattarawadee.p@rsu.ac.th
Total Article Views
Editor: Anak Iamaroon,
Chiang Mai University, Thailand
Article history:
Received: April 19 2021;
Revised: September 6, 2021;
Accepted: October 12, 2021

