
Dental Setting Design Guideline Adaptation in the COVID-19 Pandemic in Northern Thailand
Piyadech Arkarapotiwong and Sumavalee Chindapol*Published Date : 2022-01-21
DOI : https://doi.org/10.12982/CMUJNS.2022.007
Journal Issues : Number 1, January-March 2022
Abstract Criteria for dental clinic design in Thailand are recommended by the Design and Construction Division, Department of Health Service Support, Ministry of Public Health. During the Coronavirus disease pandemic (COVID-19), there were several procedures regarding dental operations and infection prevention suggested by researchers and international health organizations, including the Centers for Disease Control and Prevention (CDC), and the World Health Organization (WHO). However, some criteria still have discrepancies in practice, since they have no definite correct answers. This research describes the dental clinic redesign for COVID-19 control using dental setting design guidelines in both Thailand and foreign countries. The re-designed planning of the clinic was reviewed by dentists, engineers, and physicians. The issue of concern is the cost and the design’s value in the disinfection of facilities. Significant proven methods of disinfection are used in this paper, including functional re-consideration, negative air pressure rooms, filters, Ultra-Violet devices, and ozonators. This research contributes to the literature by providing a functional diagram for dental clinic adjustment in the COVID-19 situation. The 12 air changes per hour (ACH) ventilation combined with management protocol ensures that patients’ safety is a priority and provides a feasible option for adaptation in a developing country such as Thailand.
Keywords: Architectural design, COVID-19, Dental clinic, Guideline, Planning
Funding: The authors are grateful for the research funding provided by the the Office of Strategy Management, Chiang Mai University, Chiang Mai, Thailand.
Citation: Arkarapotiwong, P. and Chindapol, S. 2022. Dental Setting Design Guideline Adaptation in the COVID-19 Pandemic in Northern Thailand. CMU J. Nat. Sci. 21(1): e2022007.
INTRODUCTION
COVID-19 is categorized as a respiratory infection disease like SARS, which should be prevented using the same protocol (WHO, 2020). It has infected easily with the airborne and could be up to 110 days prolonged detection in some cases (Kewcharoenwong et al, 2021). The dentists have been diagnosed of COVID-19 over time in the US due to diffusion of dental service (Araujo et al, 2021). COVID-19 infections in dental units can be spread by dental instruments, creating a visible spray with particle droplets of water, saliva, blood, microorganisms, and other debris. To limit the infectiousness of these factors, the virus in the droplet needs to be eliminated using a disinfecting mouth rinse (Centers for Disease Control and Prevention [CDC], 2020a). The instruments include rotary dental and surgical instruments, such as handpieces or ultrasonic scalers and air-water syringes. The CDC (2020a) recommends two main procedures for providing dental services: one, for patients who are not suspected and two, for patients who are suspected or confirmed with COVID-19 infections. For the confirmed COVID-19 patients, there are many protocols and the standard surgery room to follow (Grelat et al, 2020). However, for the no-confirmed COVID-19 patients, there is a gap to response in terms of dental service and renovation design.
The typical dental setting consists of three zones: public, clinical, and staff zones (US Department of Veterans Affairs, 2014a). To encounter COVID-19 pandemic, the dental clinic requires several procedures (CDC, 2020a). The public zone is for patients and customers. For viral control, this area should have all unnecessary items removed and be cleaned hourly. The clinical zone includes operatory, consultation, sterilization, and laboratory areas. During the COVID-19 situation, the operatory area requires closed ventilation. It is recommended that consultations be done remotely whenever possible, with limited in-person visits to reduce density in the clinic (General Dental Council, 2020). Sterilization of the dental equipment should be performed regularly, while air sterilization with a high efficiency particulate air (HEPA) filter, Ultra-Violet (UV) ray, and other hygienic systems should be included to combat airborne infection. The laboratory area can be the dirtiest area in a dental setting. It should be completely separate from the operatory and sterilization areas. Many small dental clinics have no laboratory or heavy sterilization and use outsourced services (Malkin, 2002). The staff zone includes the meeting areas, doctor’s office, pantry, storage space, and restrooms. Most dental clinics in Thailand are not designed with a full compartment between dental units or with adequate ventilation for respiratory diseases control. They have an open plan in which several dental units sharing the same air ventilation system that lacks a UV light air purifier or HEPA filter. Also, a specific protocol for dental waste management is not available in Thailand. Thus, virus infection control in these dental settings is problematic and costly.
The dental clinic examined in this study was designed in 2018 for the Senior Wellness Complex project, Chiang Mai University. The clinic has all three zones, with an X-ray room in the clinical zone. Before construction, the clinic plan and system were analyzed and redesigned because of the COVID-19 pandemic risk in 2021.
MATERIALS AND METHODS
Objectives
1. To evaluate the dental clinic case with literature including criteria, guidelines, research, and experts’ perspective related to COVID-19 infection prevention in dental clinics.
2. To redesign the dental clinic utilizing COVID-19 prevention guidelines.
Research methodology
This research used the qualitative observational method for dentistry (Edmunds & Brown, 2012) and was conducted in three main steps. First, a preliminary survey with literature and interviews was conducted in a conventional dental setting. Second, the conventional dental clinic design was reviewed by ten experts, including dentists, engineers, and physicians. These experts were sampled purposively from executive staff members involved in lessening the effect of COVID-19 on the organization’s facilities. The respondents were 52 years old on average, with seven males and three females. Third, the dental clinic was re-designed according to certain criteria, guidelines, and research and was reviewed by the same experts. The conventional dental clinic design and re-design settings were compared and discussed by the same experts in regard to the appropriate dental clinic design under COVID-19 conditions. Using a semi-structured interview and over a 3-month period, the experts were asked their opinions of both the conventional and re-designed dental clinic plans, including specific questions on the functional arrangement and circulation plan of the space for dental services, the quality of the ventilation system, the control of medical waste, materials, and contagion management. They were also asked about the best practices for dental clinic adjustment under COVID-19 conditions. The study concerns both official recommendations in Thailand and foreign countries. Small dental clinic design with two to three dental units were considered in this study. Ten dental clinics were surveyed as representatives of a conventional setting. Only one dental clinic was surveyed as a COVID-19-appropriate re-designed dental clinic because very few clinics have been renovated in Chiang Mai. Medium and large dental clinics are beyond the scope of this study. The study concentrated on functional arrangements and circulation plans, ventilation systems, and medical waste management for COVID-19 infectious control in dental clinics.
Review: Dental clinic environmental guidelines for the COVID-19 pandemic
In Thailand, there are no regulations implemented on the treatment of COVID-19 patients in dental settings. The Ministry of Public Health (CCSA, 2020) has recommended different treatments for two patient groups: confirmed positive COVID-19 patients and uninfected patients. Confirmed positive COVID-19 patients who have severe and urgent symptoms should be treated in the dental operation room with negative air pressure. Healthy patients who have a confirmed negative COVID-19 result, have not had contact with a confirmed positive patient, and pass the COVID-19 history screening should be treated while maintaining high protection for staff and other patients. High protection includes personal protective equipment (PPE) suits for all dental staff members, film-wrapped equipment, 12–24 air changes per hour (ACH) with a HEPA filter in the dental room, and a limited number of patients at any given time (CDC, 2020a). However, no recommendations have been made regarding the adaptation of the physical setting, including ventilation. Most recommendations concern management protocols intended to limit infection. Thus, this study considers architectural adaptation as part of infectious control in a dental setting.
Functional arrangement and circulation plan
The conventional functional arrangement and circulation plan may act to decrease the risk of infection. As mentioned, the conventional planning of a dental setting has three functional zones. Such planning should allow the circulation between patients and staff to be separated (Figure 1a). The clinical zone should be directly accessible to the outside to allow for hygienic waste management. For COVID-19 infection control, some functions require more careful attention, such as the patient waiting area and clean–dirty circulation for staff. Also, the complete separation of the circulation of patients and staff should be prioritized. A full compartment between two dental units is strongly recommended; each unit should have closed ventilation to limit infection diffusion (CDC, 2020a). Although there are several recommendations for dental settings in COVID-19 conditions (Figure 1b), no definite functional arrangement has been advised.
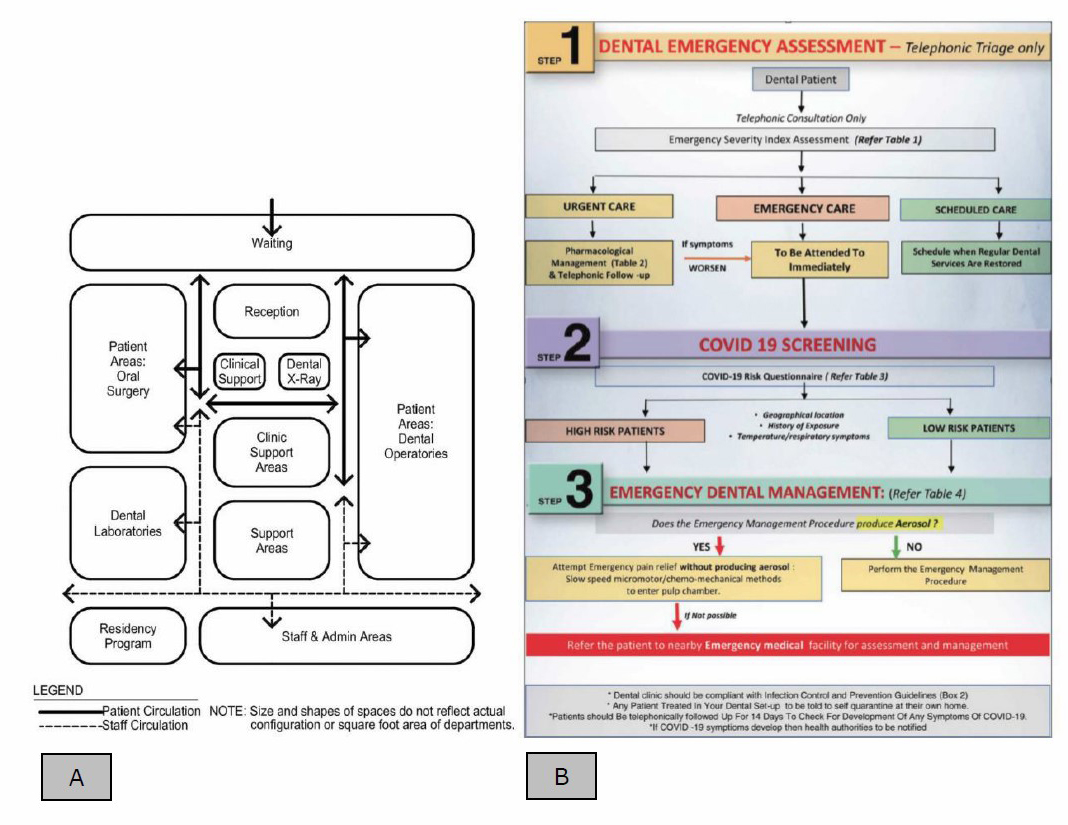
Figure 1. A. Functional arrangement diagram in conventional dental settings (US Department of Veterans Affairs, 2014b); B. dental service decision-making diagram for dental settings in COVID-19 conditions (Krithikadatta et al, 2020).
Management Guidelines.
Several protocols have been recommended by the CDC and by scholars. CDC (2020a) recommendations provide for routine dental healthcare delivery during the COVID-19 pandemic and for a suspected COVID-19 patient. For routine dental services, appointments and remote consultation are suggested. Screen COVID-19 risk and triage all patients before treatment. All dental staff should wear full PPE or level C-PPE during dental operations. The dental operatory set must be sterilized between patients. For COVID-19 patient dental services, only emergency dental operation cases are serviced. The enhanced PPE, and full procedure should follow the CDC’s Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic (CDC, 2020b).
Other concerns in dental clinic management include minimizing the number of visitors, 2-meter social distancing, removal of all unnecessary items in the waiting area, and frequent cleaning of ‘high touch’ surfaces such as reception counters, door handles, and lift buttons (Jamal et al, 2020). Patients and visitors are also advised to wear face masks always. For environmental control, scholars advise an initial or tele-screen area prior to the visit, an automatic gate, and an always-open entrance gate to reduce contact with ‘high touch’ surfaces (Parihar et al, 2020). In the operating room, all equipment surfaces should be protected by single-use disposable barriers, and they must be disposed of in biomedical waste after use (Giudice, 2020). The used PPE suits are also considered and treated as biomedical contaminated items. Decontamination, disinfection, and sterilization procedures for all equipment, handpieces, and surfaces were strictly performed after use during the COVID-19 pandemic.
Ventilation system.
Three main factors related to airborne transmission are ventilation rate, flow direction, and airflow pattern. The ventilation requirement in a hospital is a minimum rate of 12 ACH with negative pressure in bronchoscopy, triages area, and radiology waiting rooms, while only 6 ACH is required in a treatment room (ASHRAE, 2020). The 12 ACH should continue for 23 minutes and 35 minutes for airborne-contaminant removal efficiencies of 99% and 99.9%, respectively (CDC, 2020a). It is reported that the dental staff would be safe if they always wore a HEPA mask in a room with 3 ACH and if they wore a surgical mask in a room with 24 ACH (Gammaitoni and Nucci, 1997).
The Dental Association of Thailand provided guidelines for dental clinics during the COVID-19 pandemic. The Thai Design and Construction (Division Design and Construction Division, 2020a; 2020b) recommends 12 ACH and 24 ACH in conventional and new dental clinics, respectively. The dental unit renovated for COVID-19 patients requires a negative air pressure in the room with 12 ACH and 100% fresh air intake. The fresh air inlet is installed above the dentist’s head, and wind direction flows to the foot of the dental chair. The exhaust air grille should be installed below seat level (Figure 2). Enclosure of the dental unit needs to be sealed from leakage, including the ceiling-to-wall connection, doors and windows connections. The ventilation system demands double walls and prefilters, medium filters, and HEPA filters with UVC radiation. The dental staff also need to wear PPE or Power Air Purifying Respiratory (PARP) suits during services. Thai Medical Department (2019).
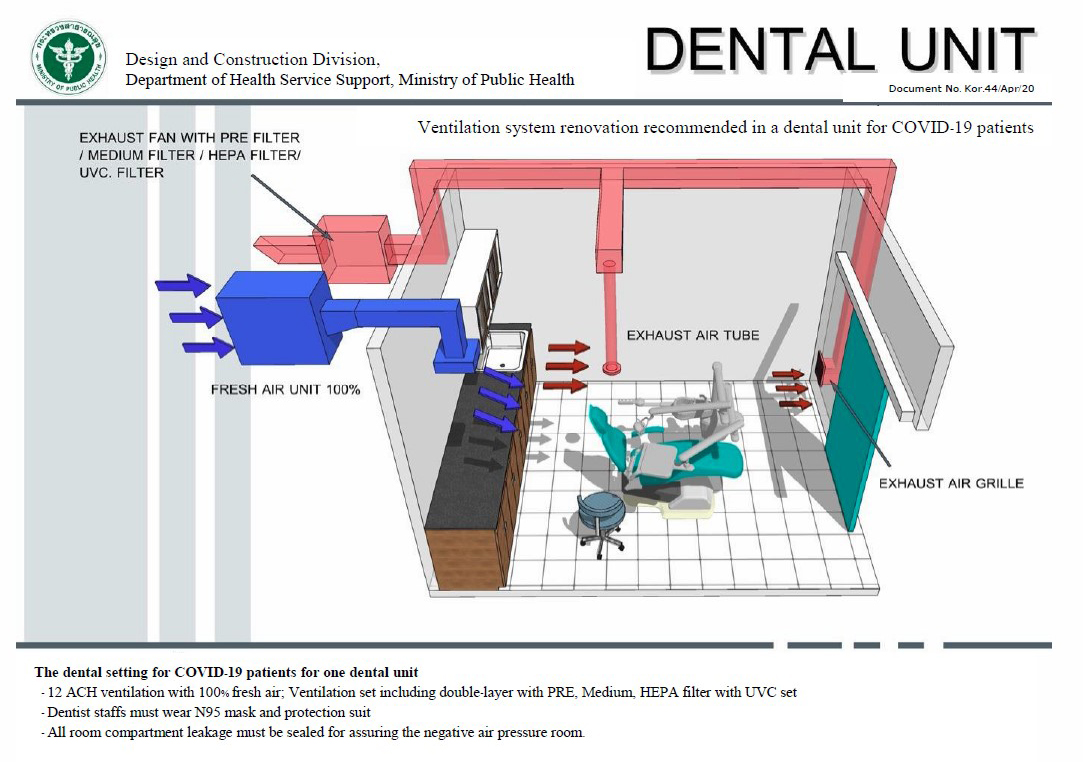
Figure 2. Ventilation system recommended in a dental unit for COVID-19 patients (Copyright 2020 by Design and Construction Division, 2020a).
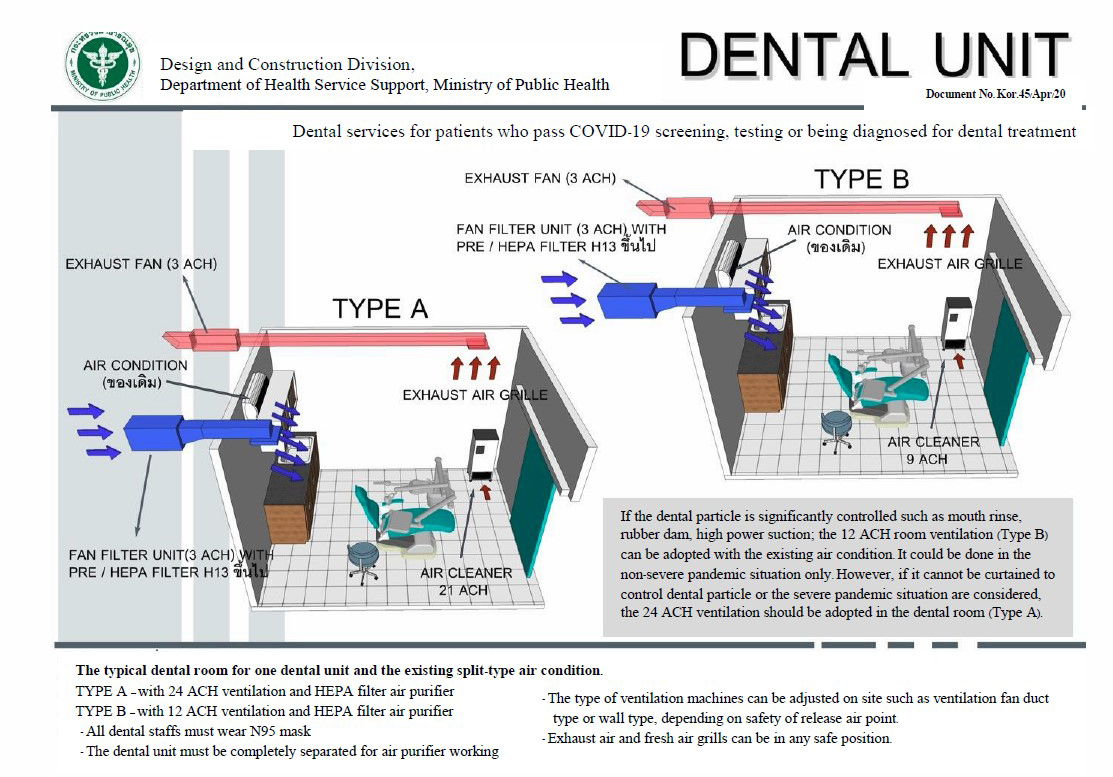
Figure 3. Ventilation system recommended in a dental unit: Type A–high speed ventilation with 24 ACH (TYPE A) and type B (TYPE B)–medium speed ventilation with 12 ACH (Copyright 2020 by Design and Construction Division, 2020b).
Material considerations.
Some metals have been reported to reduce virus contagion. Metal like copper has antiviral properties. Its alloys such as brass and bronze, are also considered antimicrobial. It takes 40 minutes on a brass surface and 2 hours on a (70/30) copper-nickel alloy surface to inactivate SARS-CoV-2 (Ren et al, 2020).
Waste management.
Medical waste during the COVID-19 pandemic should be disposed of in the medical waste oven in a routine way. However, there would be more waste to manage, since the PPE, such as masks and single-use disposable barriers, are also infectious. Medical waste collection bins and boxes should be labeled according to type, where infectious waste must be separated from sharps, toxic, hazardous, and sanitary waste (Isha, 2020; Krishnan and Pandain, 2016). Medical infectious waste must be strictly disposed of using double-layer red medical waste packaging following official infectious waste management instructions (Ministry of Interior, 2020). Coronavirus lifespans are different depending on the surface, ambient temperature, and the amount of virus. Research suggests that Coronavirus can survive three hours in aerosol, four hours on copper, 24 hours on cardboard, two to three days in stainless steel, and three days in plastic (Chin et al, 2020; Doremalen et al, 2020; Ye et al, 2016). Dental wastewater of COVID-19 patients can theoretically survive three days in sewage. Therefore, wastewater treatment from dental clinics should require disinfection procedures.
Other equipment reported to reduce contagion.
There are several types of equipment used in disinfection during the COVID-19 pandemic, such as vacuum cleaners, HEPA/Ultra – low Prenatraion Air (ULPA) filters, UV light, ozone, and air ionizers. Portable vacuum cleaners are reported to significantly reduce virus aerosols (Hudyono et al, 2020) (Figure 4) and oral bacterial aerosols (Teanpaisan et al, 2001). The use of extra vacuums for aerosol-generating procedures is recommended together with high-volume regular suction (Peng et al, 2020). A central vacuum system with a rate of 28.5 liters per minute is reported to reduce 36% of aerosols (Liu et al, 2019). HEPA filters alone may not be effective for capturing viruses since the HEPA filter scale is 0.3 µm while virus particles are less than 0.1 µm (Rupf et al, 2015). The extra vacuum cleaner requires HEPA filters, charcoal filters, and UV sterilization to absorb and disinfect the aerosol during the dental treatment. The output of the vacuum can be disinfected by releasing it outdoors since the virus is inactivated in high temperature in a tropical country. However, there is inadequate proof of its efficiency.
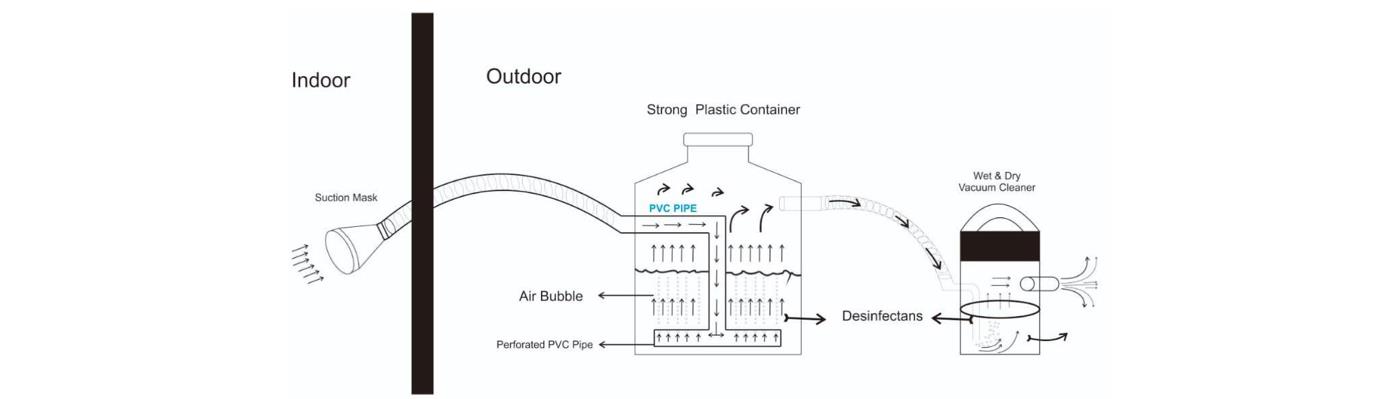
Figure 4. The vacuum cleaner used to reduce aerosol for dental operations (Hudyono et al, 2020).
Theoretically, HEPA filters can capture 99.97% particles larger than 0.3 μm, and ULPA filters capture 99.99% of particles larger than 0.12 µm. HEPA filters capture droplets and ULPA filters capture other smaller particles. Although the HEPA filter scale is greater than 0.3 µm, staked prefilter mechanisms, such as diffusion, interception, inertial impaction, and electrostatic attraction, help a HEPA filtration system reduce the bioaerosol level in environments like dental environments (Dehghani et al, 2018). Air purifiers with high volume are also recommended for use with HEPA14 and UV light (Miglani et al, 2002).
UV spectrums used for sterilization include UV far (190-200 nm), UVC (220–290 nm), and UVB (290–320 nm) (Tobiska and Nusinov, 2005). UVC germicidal lamps (220–290 nm) are mainly used in sterilization procedures, including environments and surfaces. The 253.7 nm wavelength shows the best results for maximum absorption of a virus DNA molecule at 260 nm (Cumbo et al, 2020). UV radiation can restructure the nucleic acid of the virus cells but it seems less effective on viruses with RNA or DNA, depending on the cell wall thickness of viruses. UV rays also affect the viruses associated with water or surface contamination (Tseng and Li, 2005).
UV light with wavelengths of 200–228 nm significantly inactivates SARs-CoV-1 and MERS-CoV (Bedell et al, 2016). UVC can disinfect viruses using two main technologies: mercury UV and pulsed xenon UV. It is recommended to use the 40 µW/cm2 UV lamp at the center of the work area to disinfect and decontaminate the viruses (Brian, Harrington and Valigosky, 2007). UV device efficiency is measured using four parameters: dosimetry, environmental studies, in vitro studies, and clinical outcome data. Portable UV light devices are beneficial for the whole dental clinic, including reception areas, dental assistant counters, and other small equipment surfaces. However, UV light requires time to inactivate the virus infection (IUVA, 2020). Although UV rays seem quite handy for sterilization, their disadvantages are negative side effects on human skin and the damage or discoloration of surfaces, particularly plastic ones. In dental clinics, when one operating room is occupied, another one can be treated by UV rays (Cumbo et al, 2020).
Ultraviolet Germicidal Irradiation (UVGI) applications are provided to disinfect water, surfaces, and air. UVGI has been officially suggested by the CDC (2003) for sterilization in the hospital since 1994. This paper suggests using UVGI irradiation in upper-room air since it can be performed while dental activities are ongoing with no harm to humans. Upper-room UVGI relies on upper-lower air circulated with a ventilation system. Suggested UVGI values at the fixture are 200-340 µW/cm2 at 2.30 m and 0.2-0.4 µW/cm2 at 1.70 m. Although it seems to be quite a convenient strategy, UVGI technology has been used in Thailand for 10 years in a sterilized cabinet rather than the upper-room UVGI. However, UVGI disinfects in lightened areas. It needs to be combined in a circulated ventilation system to clean the whole room (Figure 5).
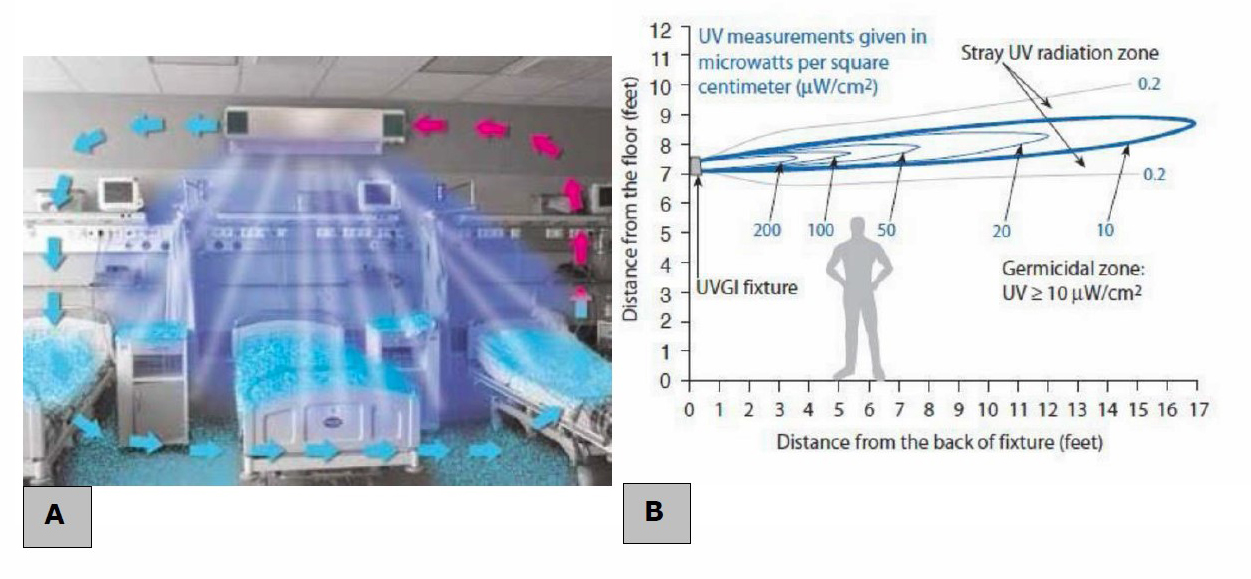
Figure 5. UVGI with circulated ventilation system (A) and its performance (B) (Ampornaramveth, 2020).
Ozone is widely known for its antiviral and antimicrobial properties. It can immediately damage lipid molecules of viruses, including SARS and COVID-19 viruses, up to 99% (Hudson, Sharma and Petric, 2007). Ozone is effective on all surfaces, textures, materials, and liquids. A great degree of inactivation is reported at a relative humidity of 70% or above (Cumbo et al, 2020). However, during 20 minutes of oxidation, ozone with a 0.1 ppm concentration in the air is toxic. During that time, it was toxic for human respiratory tissues and plant tissues (Lippmann, 1989). Similar to UV rays, dental operating rooms need 20 minutes for sterilization. The rooms can be occupied by patients and ozonators.
Air ionizers can reduce bacterial and viral infections by electric field sterilization. Air ionizer devices, called electron wind generators (EWG), can irreversibly damage the cellular film of microbes in the air, significantly reduce the spread of infectious viruses, and break down double stranded virus DNA (Hagbom et al, 2015). High voltage fields are recommended, from 5–15 Kvolt (Grabarczyk, 2001). EWG technology seems effective in virus disinfection and has no side effects on humans. Therefore, it is quite convenient for sterilization and does not disturb dental activities.
Conclusively, not all disinfection options will be affordable for a general dental clinic. Contagion management must be performed following government procedures (Medical Department, 2019; Ministry of Interior, 2020). If there is a budget for renovations, adjustment of the ventilation system should be the first priority, since such a renovation can greatly reduce the risk of infection. Air flow direction is the most important factor, followed by air change rate volume. If a dental clinic has recirculated ventilation, filtration quality and a system of disinfection should be of great concern. Functional arrangement and circulation should be the next priority. Maintaining separate zones for patients and staff requires little cost and can be easily sustained. Other disinfection systems, such as UVGI or an ozonator, are optional, as they are expensive for investment and maintenance.
RESULTS
Problem analysis in conventional dental unit design in the Senior Wellness Complex, Chiang Mai University
Experts have commented on conventional dental clinic issues. There are several problems surrounding virus contagion, including planning, ventilation systems, medical waste, materials, and management (Table 1).
Function and circulation of a conventional dental clinic.
Staff movement was not separated during preparing and service between cleaning rooms and operating rooms (Bhatrakarn, 2012) (Figure 6). The cleaning room and operating rooms should have the dirtiest air if there is a COVID-19 patient for operating. The dentists’ rooms and operating rooms were separated by a waiting area. If COVID-19 suspected patients visit the clinic, it may risk all staff and visitors, since there has been no air compartmenting. Even though there are several screening procedures, such as travel history screening, entering temperature, mask wearing, and hand sanitizing with alcohol. The infection between operating rooms and other rooms may be a consequence.
Infection risks from ventilation systems.
Conventional ventilation systems in the operating room do not have restrictive air direction control. During the COVID-19 pandemic, we cannot be sure that visitors were free from the virus. To limit virus contagion of the suspected patient, air direction is highly recommended to pass from the clean to the dirty area: from the waiting area to the operating room. The negative-positive air pressure is suggested for virus contagion reduction. Dental operating activities may release infected aerosols; therefore, the operating rooms are the dirtiest areas in the dental clinic. Negative air pressure is advised in the area with the highest contamination level since there is an aerosol source. Positive pressure is suggested in low contamination level areas like waiting areas, supply rooms, dentists’ rooms, and x-ray rooms. Conventional ventilation systems may cause cross-infection among patients and staff (Figure 7). A rate of at least 6 ACH is proposed for general dental services, and 12–24 ACH are recommended in the operating room.
Medical waste management.
All waste will be disposed of in the cleaning room and delivered by staff after office hours. During the COVID-19 pandemic, all staff members are required to wear PPE suits for operations. They need to walk in and out between operating rooms and cleaning rooms. Contamination may be caused by these incidences. The space in the cleaning and supply rooms is also inadequate for cleaning activities during COVID-19.
Materials.
Easy cleaning materials are suggested for reception and dental staff counters, such as plastic, stainless steel, brass, and copper. Fabric and wallpaper are not recommended for this situation. Although copper has been reported as the shortest virus lifespan surface, it needs a large budget to use copper surfaces in dental clinic. The conventional clinic uses granite and plastic surfaces for frequent cleaning.
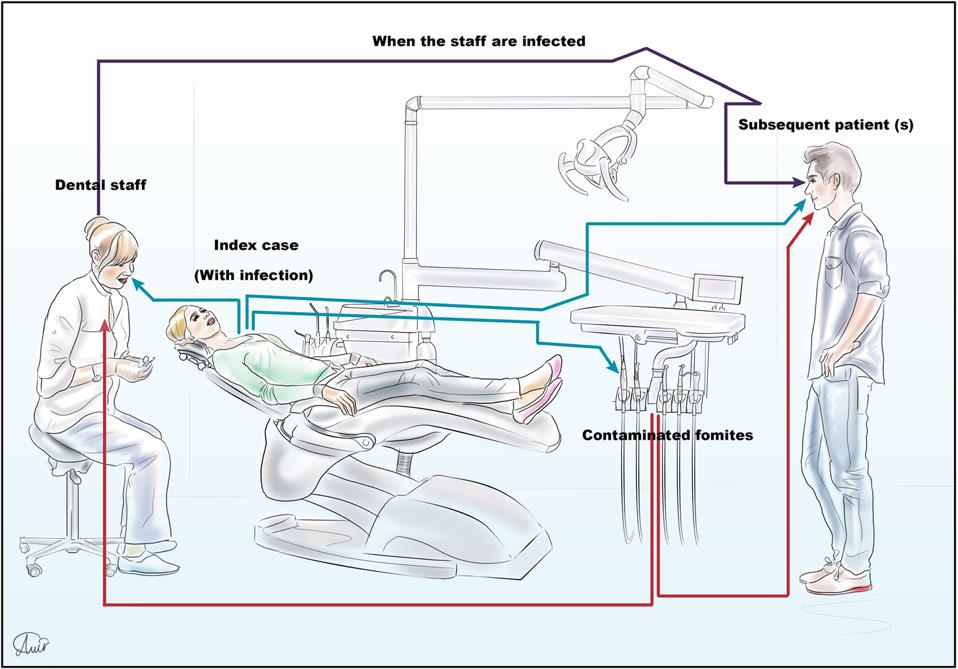
Figure 6. COVID-19 transmission dynamics in dental care settings (Fallahi et al, 2020).
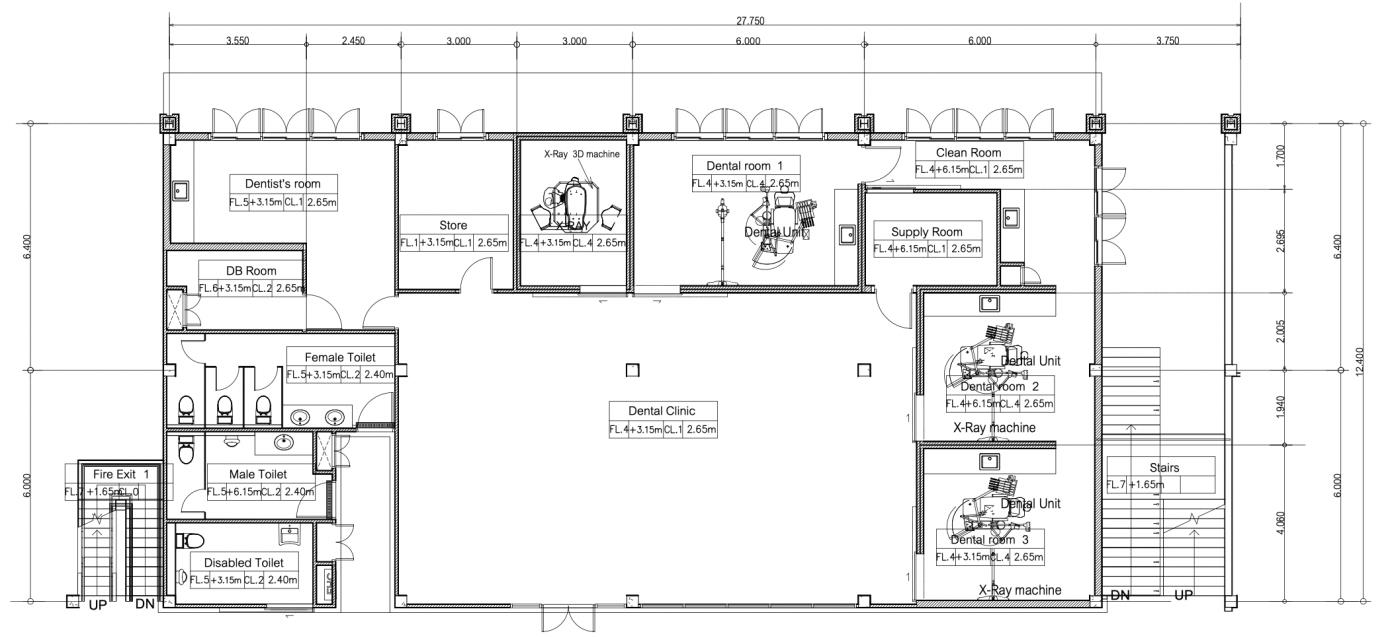
Figure 7. Conventional dental clinic layout designed in 2018.
Table 1. Expert feedback on conventional dental clinic design toward COVID-19.
|
COVID-19 Risks |
Expert 1 (Dentists) |
Expert 2 (Engineers) |
Expert 3 (Physicians) |
|
Functional and circulation for dental services |
- Operating rooms should be isolated from staff circulation to reduce contamination. - A changing area is required for PPE dressing, and it should connect to the operating rooms. - A larger circulation area is required for PPE suits, carts, and wheelchairs in both waiting and staff areas. |
- The staff circulation is combined between two operating rooms which may cause contagion. - Staff areas should be enlarged for cleaning activities. |
- Circulation of staff and visitors should be separated for contagion reduction. - The waiting area is adequate for bubble social distancing between seats.
|
|
Ventilation system |
- Negative air pressure is required in all operating rooms, supply room, and cleaning room. - The supply air grill should be above the dentist’s position and the return air inlet should be on the foot of the chair. - All windows should be fixed to ensure fully controlled ventilation. - Drop-seals are required for all doors. - 12 ACH is required in operating rooms. |
- Ventilation in waiting areas and operating rooms is contaminated. Air-ventilation must be separated in zones with drop-sealed doors. - 8ACH or more is advised combined with HEPA and UVC filters. - Head-to-toe ventilation of the patient chair is recommended for air movement direction. - A portable dental vacuum cleaner is suggested in the operating room. |
- A high speed sterilization system must be added in the air-condition system such as filter, HEPA, UVC, UVGI. - The entrance gates should be opened automatically to minimize touch. - Air curtains should be applied in all doors. |
|
Medical waste |
- Waste should be disposed after clinic hours only and transported in the separated circulation. - Wastewater from the dental unit must be virus-disinfected before being released to the public (close system recommended). |
- Wastewater from dental units is organically treated in the dental wastewater treatment before releasing to the public. - A concentration of treatment waste should be required. |
- Biohazardous waste is suggested to be sealed, transferred and disposed in the hospital incinerator. |
|
Materials |
- All surfaces must have a gloss or smooth finish for frequent cleaning. - Copper, brass, and bronze have antiviral and antimicrobial properties. |
- Gloss and smooth surfaces like metal or plastic are highly recommended since they are easily and often cleaned. |
- Surfaces should be easy cleaning and non-infectious such as gloss finish, metal, and plastic. |
|
Contagion management |
- Tele-screen for remote dental care consultation is required. - Screening areas with alcohol sanitizers and thermometers should be provided for all visitors before entering the waiting area. |
- A limited number of visitors is suggested. - All visitors’ travel history should be reported at the reception to evaluate the risk. |
- Urgency level of symptom should be considered to prioritize the service: emergency, urgent, and elective cases. |
Re-design of the dental clinic for the pandemic
The dental clinic was redesigned in response to the literature on the COVID-19 pandemic and the experts’ reviews.
Function and circulation
This research reviewed the literature and relevant case studies to develop a functional diagram for dental clinic design under COVID-19 conditions (Figure 8). Functions are grouped into three zones—public, clinical, and staff zones—with complete separation of the circulation of patients and staff (Figure 9). The general zone includes the waiting area and dentists’ rooms, which welcome any new visitors. The disinfection zone is set at the entrance gate with alcohol and a UV light. The air curtain system is installed at the entrance to separate interior and outdoor ventilation. All seats in the waiting area are placed two meters apart from each other. The operation zone consists of three operating and one X-ray room. These four rooms are connected to service circulation through the supply and cleaning rooms. All doors in the clinic are drop-sealed doors to limit air leaks between zones, since this area is the most contaminated area of all the rooms. The service zone includes a cleaning room, supply room and staff circulation. The staff circulation requires a separated entrance to divide clean and dirty functions. The infectious waste can be disposed of from each operating room to the cleaning room without contamination between operating rooms. Operating, cleaning, and supply rooms are enlarged for disinfection activities and connected to staff circulation. While the waiting area is reduced by minimizing the number of visitors.
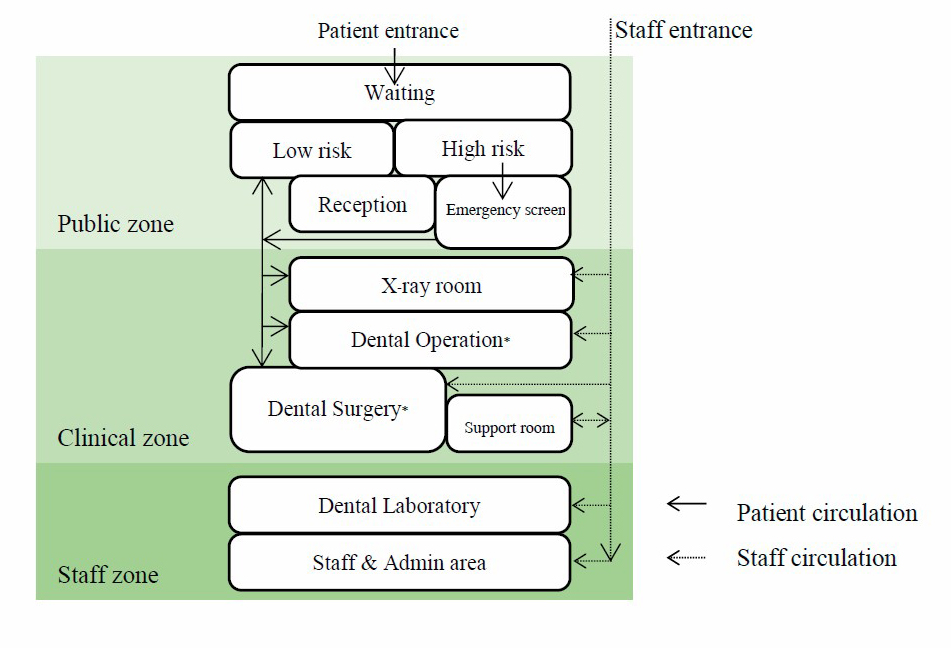
Figure 8. Functional diagram for dental settings during COVID-19 pandemic.
Note: * denotes a room with negative air pressure.
Ventilation system
Negative air pressure was designed in all three operating rooms, while positive air pressure was set in the other zones. Regarding air flow direction, positive air pressure is provided in general and in the service zones. The upwind air flows from the waiting room to the downwind air in the operating rooms. High horsepower (HP) fans are required to comply with a 600 CFM air change in operating room one and 800 CFM air change in operating rooms two and three. Supply air grills are installed in the ceiling above the dentist’s chair, with 400 CFM in operating room one and 300 CFM in operating room two and three. Fresh air grills are designed for a 600 CFM air change in operating room one and 450 CFM in operating room two and three. Pollution and particulate matter (PM) 2.5 strainers consist of a Merve 8 prefilter, a Merve 14 medium filter, and a HEPA filter. An exhaust air grill is installed at 0.3–0.8 meters above the floor on the wall toward the foot of the patient chair (Figure 10), with a 500 CFM air change in operating room one and 400 CFM air change in operating rooms two and three. The 800 CFM exhaust air blower adds disinfection for COVID-19 contagion reduction, including a Merve 8 prefilter, Merve 14 medium filter, HEPA filter, and a UV lamp. Due to the high-speed air change rate required in dental clinics during COVID-19, 12 ACH was designed in the ventilation system. The UVGI system will also be installed at a height of 1.80 meters in all operating rooms.
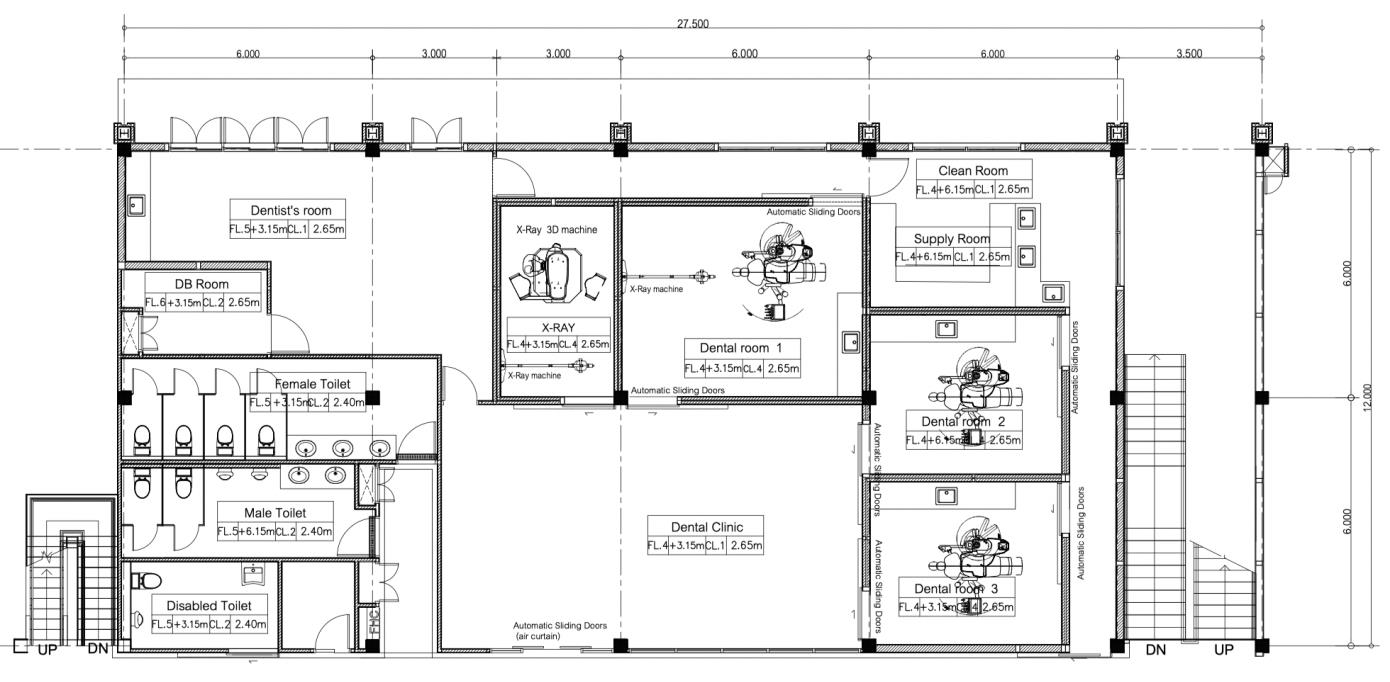
Figure 9. Redesigned dental clinic layout for COVID-19 pandemic designed in 2021.
The operation rooms are the dental service room most at risk of contamination. They are designed with a negative air flow to limit the spread of infection to the other rooms. The air direction flows from the entrance to the reception area, then to the waiting area, and ends in the operation rooms. The staff zone also has positive air flow but with its own exhaust air grill. The ventilation inside the staff zone will be circulated only within the zone, meaning that the patient and staff zones cannot contaminate each other.

Figure 10. The exhaust air grill installed in the dental unit at the Faculty of Dentistry, Chiang Mai University.
Medical waste management
There are three types of dental waste during COVID-19. The infectious medical solid waste will be disposed of in the red bin and transferred to the hospital incinerator by the end of the day. The medical solid waste includes masks, PPE, single-use equipment barriers, and tissue or suspected infectious objects. The medical waste, like sharp items, should be disposed in the thick waste bag and treated the same as medical solid waste. The normal solid daily waste will be disposed of in either general or recycle bins. This waste type may be disinfected before closing the waste bags due to the possibility of virus contamination. The last dental waste is wastewater. Dental wastewater is theoretically treated by amalgam separator, plaster separator, and a disinfecting sanitary system following The Clinical Practice Guidelines for Dental Infectious Prevention (Medical Technical Office, 2004).
Other disinfection options
Sterilization procedures are strictly conducted during COVID-19. Special sterilized equipment should be provided such as pre-post vacuum autoclaves, surgical handpiece sterilizers, and suction sterilization. The ozonators may be used daily after office hours for certified 100% disinfection.
Experts’ feedback on the re-design
All the experts agreed that the re-design has the potential to be highly effective against the spread of COVID-19. Most issues of concern in the review were considered in the re-design. Functional arrangement and the circulation of dental services assure the separation of patients and staff, limiting contamination. The ventilation system is adequate in terms of air change rate and direction flow. The disinfection system used in the re-design would be well operated. However, the use of UVGI and a dental vacuum cleaner may not be appropriate for every dental setting, as the greater the efficiency of the virus disinfection equipment, the higher the cost. Thus, not all organizations will have the budget for such equipment. The experts advised that management protocols should be combined with appropriate disinfection of facilities and equipment for contagion control. Waste management should strictly follow medical waste disposal protocol (Ministry of Interior, 2020). Although the use of copper has not been applied in the re-designed clinic, its use may be appropriate in situations of limited budget.
DISCUSSION
Applying the guidelines for dental unit adaptation during COVID-19 has not only been difficult in practice since it requires specific knowledge, time, extra space for installation and additional budget. But it has also reluctant recommendations in the same topic. No authority has made a recommendation on the architectural arrangement of dental settings under COVID-19 conditions. This research contributes to the literature by providing a functional diagram for dental settings during COVID-19. Circulation should be exclusively separate between patients and staff to ensure reduction in infection, and ventilation should be fully released to the outside. If air is recirculated, a HEPA infiltration system and UV ray with positive air flow should be installed in the ventilation system. However, since such renovations are costly, many researchers recommend that natural ventilation be applied to reduce contamination (Chin et al, 2020; Krithikadatta et al., 2020). Thus, architectural adjustment plays an important role in ventilation adaptation intended to achieve full ventilation control.
There are several suggestions about the value of the air change rate required in the dental operating room, from 6–12 ACH by the Thai authority to 12–24 ACH by the US authority in the CDC guidelines. It depends on the definition of the dental operating room. Thai agencies interpret the operating room as a treatment room requiring 6–12 ACH, while the CDC specifies it as a surgical room which needs 12-24 ACH. This not only affects the specifications of the ventilation system, but it also results in different times required for virus removal. In the 6–12 ACH case, 300-600 CFM with a 1–2 HP motor are required for the blower fan. Whereas 12-24 ACH needs more than 800 CFM with several 2 HP motors. However, the higher the power of the blower, the shorter the time for removal to 99% efficiency. Twelve ACH takes 23 minutes for removal time, while 20 ACH only takes 14 mintues (CDC, 2020b). Dental clinic designed in this paper follows the Thai authority’s recommendations since they are more suitable in the Thai context than the US CDC’s. Moreover, the Thai suggestion allows less renovation budget to control COVID-19. But it needs to combine with management protocols (AI-Halabi et al, 2020). The re-designed clinic in this research costs approximately three million Baht (91,206$US) to build; this price includes architectural rearrangement and a ventilation system with 12 ACH HEPA infiltration, UV ray sterilization, and positive air flow. It does not include the cost of electricity and maintenance during operation. The US guidelines suggest 24 ACH, which is a high standard and cost over 5.5 million Baht (167,266$US) to renovate only three dental units. With high standard of the enhanced infection control protocol, three dental clinics in New York has been no report of COVID-19 transmission case from 2,810 patients during a 6-month period (Froum and Froum, 2020). It has been unclear on feasibility since there is no expenditure reported in the study.
Although the ventilation quality in Thailand is lower than in the US, other infection protocols will support a safe dental service. However, for safety in areas with high rates of COVID-19 infection, all dental clinics should be closed, and emergency cases should be dealt with at the hospital (CCSA, 2021). Research suggests that the Thai option is a more sustainable protocol for a developing country than the US option, since it represents a compromise between investment and management. All applications and devices obtained for the COVID-19 situation can also be applied to the post-COVID situation.
This research presents the perspectives of the supply section, which includes the dentist, the architect, the engineer, and the executive staffs. Future studies should compare the perspectives of dental staff members and their patients.
ACKNOWLEDGEMENTS
The authors thank the Office of Strategy Management, Chiang Mai University for providing information of the Senior Wellness Complex Center, Chiang Mai University.
AUTHOR CONTRIBUTIONS
Piyadech Arkarapotiwong designed and conducted all of the methods and clinic design and wrote the manuscript. Sumavalee Chindapol assisted in conducting the experiments, performed the support information and data visualization and wrote the manuscript. All authors have read and approved of the final manuscript.
CONFLICT OF INTEREST
The authors declare that they hold no competing interests.
Bedell, K., Buchaklian, A.H., and Perlman, S. 2016. Efficiency of an automated multiple emitter whole-room Ultraviolet-C disinfection system against coronavirus MHV and MERS-CoV. Infection Control Hospital Epidemiology. 37: 598-599.
Bhatrakarn, T. 2012. Dental Clinic Design Guidelines. Journal of the Faculty of Architecture, Chulalongkorn University. 61: 43-58.
Brian, J., Harrington, B.J., and Valigosky, M. 2007. Monitoring Ultraviolet Lamps in Biological Safety Cabinets with cultures of standard bacterial strains on TSA blood agar. Labolatory Medicine. 38: 165–168.
CCSA. 2020. Order of the Centre for the Administration of the Situation due to the Outbreak of the Communicable Disease Coronavirus (COVID-19) No. 2/2563 Re : Guidelines based on Regulations Issued under Section 9 of the Emergency Decree on Public Administration in Emergency Situations B.E. 2548 (2005). Center for COVID-19 Situation Administration (CCSA), Ministry of Interior, updated on 31 July 2021.
CDC. 2003. Infection control: Guidelines for environmental infection control in health-care facilities. Available from https://www.cdc.gov/infectioncontrol/guidelines/ environmental/index.html [Accessed on 20 May 2021]
CDC. 2020a. Guidance for dental settings: interim infection prevention and control guidance for dental settings during the coronavirus disease 2019 (COVID-19) Pandemic, Centers for Disease Control and Prevention (CDC), US, updated December 4, 2020. Available from: http://www.cdc.gov4_12_20 [Accessed 25 April 2021]
CDC. 2020b. Infection control: severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), Interim Infection Prevention and Control Recommendations for Patients with Suspected Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings, updated March 19, 2020. Available from https://www.esrdnetwork.org/sites/default/files/Infection%20and%20Prevention%20-%20CDC.pdf [Accessed 25 April 2021]
Chin, A.W.H., Chu, J.T.S., Perera, M.R.A., Hui, K.P.Y., Yen, H.-L., Chan, M.C.W., Peiris, M. and Poon, L.L.M. 2020. Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe. 1: E10.
Cumbo, E., Gallina, G., Messina, P., and Scardina, G.A. 2020. Alternative methods of sterilization in dental practices against COVID-19, International Journal of Environmental Research on Public Health. 17: 5736.
Dehghani, M., Sorooshian, A., Nazmara, S., Baghani, A.N., and Delikhoon, M. 2018. Concentration and type of bioaerosols before and after conventional disinfection and sterilization procedures inside hospital operating rooms. Ecotoxicology Environmental Safety. 164: 277-282.
Design and Construction Division. 2020a. Document No. Kor 44, Dental unit ventilation system renovation guideline for patients with COVID-19 [in Thai]. Department of Health Service Support, Ministry of Public Health, Thailand. Released in April 2020.
Design and Construction Division. 2020b. Document No. Kor 45, Dental unit design guideline for patients who pass pre-screen of COVID-19 [in Thai], Department of Health Service Support, Ministry of Public Health, Thailand. Released in April 2020.
Doremalen, N. van, Bushmaker, T., Morris, D., Holbrook, M., Gamble, A., Williamson, B., Tamin, A., Harcourt, J., Thornburg, N., Gerber, S., Lloyd-Smith, J., Wit, E. de, and Munster, V. 2020. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1, The New England Journal of Medicine. Letter to editor.
Edmunds, S. and Brown, G. 2012. Doing qualitative research in dentistry and dental education. European Journal of Dental Education 16: 110-7.
Fallahi, H.R., Keyhan, S.O., Zandian, D., Kim. S.-G. and Cheshmi, B. 2020. Being a front-line dentist during the Covid-19 pandemic: a literature review. Maxillofacial Plastic and Reconstructive Surgery 42: 6.
Froum, S.H. and Froum, A. J. 2020. Although three dental clinics in New York has been no report of COVID-19 cases during a 6-month period with high degree of protective equipment and management. Int J Periodontics Restorative Dent. 40: 853-859.
Gammaitoni, L., and Nucci, M.C. 1997. Using a mathematical model to evaluate the efficacy of TB control measures. Emergency Infection Diseases. 3: 335-42.
General Dental Council. 2020. High level principles for good practice in remote consultations and prescribing. Available from https://www.gdc-uk.org/docs/default-source/guidance-documents/high-level-principles-remote-consultations-and-prescribing.pdf. [Accessed on 15 September 2021].
Giudice, R.L. 2020. The severe acute respiratory syndrome Coronavirus-2 (SARS CoV-2) in Dentistry. Management of Biological Risk in Dental Practice. International Journal of Environmental Research and Public Health. 17: 1–12.
Grabarczyk, Z. 2001. Effectiveness of indoor air cleaning with corona ionizers. J. Electrost. 51: 278–283.
Grelat, M., Pommier, B., Portet, S., Amelot, A., Barrey, C., Leroy, H.A. and Madkouri, R. Patients with Coronavirus 2019 (COVID-19) and Surgery: Guidelines and Checklist Proposal. World Neurosurg. 139(July): e769-e773.
Hagbom, M., Nordgren, J., Nybom, R., Hedlund, K.O., Wigzell, H. and Svensson, L. 2015. Ionizing air affects influenza virus infectivity and prevents airbourne-transmission. Sci. Rep. 5: 11431.
Hudson, J.B., Sharma, M., and Petric, M. 2007. Inactivation of norovirus by ozone gas in conditions relevant to healthcare. Journal of Hospital Infection. 66: 40–45.
Hudyono, R., Bramantoro, T., Benjamin, B., Dwiandhono, I., Soesilawati, P., Hudyono, A.P., Irmalia, W.R. and Nor, N.A.M. 2020. During and post COVID-19 pandemic: prevention of cross infection at dental practices on country with tropical climate. Dental Journal (Majalah Kedokteran Gigi). June. 53: 81-87.
Isha, S.N. 2020. Dental clinic architecture prevents COVID-19-like infectious diseases. Health Environment Research & Design Journal. 1: 1–2.
IUVA. 2020. UV disinfection for COVID-19. Available from http://www.iuva.org/IUVA-Fact-Sheet-on-UV-Disinfection-for-COVID-19. [Accessed on 25 April 2021]
Jamal, M., Shas, M., Almarzooqi, S.H., Aber, H., Khawaja, S., Abed, R.E., Alkhatib, Z. and Samaranayake, L.P. 2020. Overview of transnational recommendations for COVID-19 transmission control in dental care settings. Oral Diseases. 00: 1–10.
Kewcharoenwong, C., Khamduang, W., Kwunchoo, S., Chantawiang, K., Pinta, P., Promarat, S., Punchaburi, B. and Pornprasert, S. 2021. Prolonged Detection of SARS-CoV-2 RNA in An Asymptomatic Individual in Thailand: A Case Study. CMUJ. Nat. Sci. 20: e2021061.
Krishnan, S., and Pandain, S. 2016. Dental office design and waste care management in infection control. International Journal of Pedodontic Rehabilitation. 1: 37.
Krithikadatta, J., Nawal, R.R., Amalavathy, K., McLean, W. and Gopikrishna, V. 2020. Endodontic and dental practice during COVID‑19 pandemic: Position statement from the Indian Endodontic Society, Indian Dental Association, and International Federation of Endodontic Associations. Endodontology. 32(2April-June): 55-66.
Lippmann, M. 1989. Health effects of ozone: a critical review. JAPCA. 39: 672-695.
Liu, M.H., Chen, C.T., Chuang, L.C., Lin, W.M., and Wan, G.H. 2019. Removal efficiency of central vacuum system and protective masks to suspended particles from dental treatment. PLoS One. 14: 1-9.
Malkin, J. 2002. Medical and Dental Space Planning: A Comprehensive Guide to Design, Equipment, and Clinical Procedures. 3rd ed. New York: John Wiley & Sons.
Medical Department. 2019. Practice guideline for dental treatment in COVID-19 pandemic, Ministry of Public Health, Thailand. Bangkok: Ministry of Public Health.
Medical Technical Office. 2004. Clinical practice guideline: control and supervision for dental infectious prevention. Medical Department, Ministry of Public Health, Thailand. Bangkok: Agricultural cooperative.
Miglani, S., Ansari, I., Ahuna, B., and Gupta, A. 2002. Use of Newer Protective and Disinfection Strategies: A simple tool guide for the dentists during the COVID-19 pandemic. International Journal of Current Research and Review. 12: 151–154.
Ministry of Interior. 2020. Waste disposal measures during COVID-19 pandemic. Document IR 0820.2/W1759 [in Thai]. Released March 24, 2020.
Parihar, A., Saxena, A., Rawat, A. and Jain, A. 2020. COVID-19: Influenced alternation in dental OPD management. International Journal of Applied Dental Sciences. 6: 349-355.
Peng, X., Xu, X., Li, Y., Cheng, L., Zhou, X., and Ren, B. 2020. Transmission routes of 2019-nCoV and controls in dental practice. International Journal of Oral Sciences. 12: 9.
Ren, S.Y., Wang, W.B., Hao, Y.G., Zhang, H.R., Wang, Z.C., Chen, Y.L. and Gao, R.D. 2020. Stability and infectivity of coronaviruses in inanimate environments. World Journal of Clinical Cases. 8: 1391.
Rupf, S., Berger, H., Buchter, A., Harth, V., Ong, M.F., and Hannig, M. 2015. Exposure of patient and dental staff to fine and ultrafine particles from scanning spray. Clinical Oral Investigation. 19: 823-30.
Teanpaisan, R., Taeporamaysamai, M., Rattanachone, P., Poldoung, N. and Srisintorn, S. 2001. The usefulness of the modified extra-oral vacuum aspirator (EOVA) from the household vacuum cleaner in reducing bacteria in dental aerosols. International Dental Journal. 51: 413-416.
Tobiska, W.K., and Nusinov, A.A.J. 2005. Status of ISO draft international standard for determining solar irradiances (DIS 21348). Advanced Space Research. 1: 1-10.
Tseng, C.C. and Li, C.S. 2005. Inactivation of Virus-Containing Aerosols by Ultraviolet Germicidal Irradiation. Aerosol Sciences Technology. 39: 1136-1142.
US Department of Veterans Affairs. 2014a. Dental service design guideline. Office of construction and facilities management. Washington, DC.
US Department of Veterans Affairs. 2014b. Chapter 222: Dental service, PG-18-9: Space planning criteria. Veterans Health Administration, Washington, DC. Revised 3 October 2016.
WHO. 2020. Novel Coronavirus (2019-nCoV) Situation Report – 1. WHO Bull (Jan): 1-7.
Ye, Y., Ellenberg, R.M., Graham, K.E., and Wigginton, K.R. 2016. Survivability, partitioning, and recovery of enveloped viruses in untreated municipal wastewater. Environment Science s Technology. 50: 5077-5085.
OPEN access freely available online
Chiang Mai University Journal of Natural Sciences [ISSN 16851994]
Chiang Mai University, Thailand
https://cmuj.cmu.ac.th
Piyadech Arkarapotiwong and Sumavalee Chindapol*
Faculty of Architecture, Chiang Mai University, Chiang Mai 50200, Thailand
Corresponding author: Sumavalee Chindapol, E-mail: sumavalee.ch@cmu.ac.th
Total Article Views
Editor: Korakot Nganvongpanit,
Chiang Mai University, Thailand
Article history:
Received: July 21, 2021;
Revised: September 17, 2021;
Accepted: September 21, 2021

