
Prolonged Detection of SARS-CoV-2 RNA in An Asymptomatic Individual in Thailand: A Case Study
Chidchamai Kewcharoenwong, Woottichai Khamduang, Sirintra Kwunchoo, Kesinee Chantawiang, Piyapong Pinta, Sarik Promarat, Bunleng Punchaburi, And Sakorn Pornprasert*Published Date : 2021-04-01
DOI : https://doi.org/10.12982/CMUJNS.2021.061
Journal Issues : Number 3, July-September 2021
Abstract Clinical characteristics of patients hospitalized with coronavirus disease 2019 (COVID-19) have been reported in Thailand, but there is still no asymptomatic case with prolonged persistence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA has been described. Here, we report, for the first time, the detection of SARS-CoV-2 RNA from nasopharyngeal and throat swab specimens for at least 110 days in a 30-year-old Thai female with no clinical symptoms. The COVID-19 IgG antibody was also observed in her blood sample. However, her husband was negative for both SARS-CoV-2 RNA and IgM/IgG antibody, implying no transmission of SARS-CoV-2 to her husband throughout the 110 days. As far as we know, this is the very first asymptomatic case to show the longest prolonged persistence of SARS-CoV-2 RNA from nasopharyngeal and throat swab specimens in Thailand. In most cases of COVID-19 infection, molecular monitoring for SARS-CoV-2 may be discontinued, and asymptomatic cases may be underestimated. Thus, the information in this report could be combined with additional data sources to raise public health awareness with regard to clinical management.
Keywords: Asymptomatic individual, COVID-19, Prolonged detection, SARS-CoV-2
Funding: The authors are grateful for the research funding provided by the faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand.
Citation: Kewcharoenwong, C., Khamduang, W., Kwunchoo, S., Chantawiang, K.,Pinta, P., Promarat, S., Punchaburi, B., and Pornprasert, S. 2021. Prolonged detection of SARS-CoV-2 RNA in an asymptomatic individual in Thailand: A case study. CMUJ. Nat. Sci. 20(3): e2021061.
INTRODUCTION
The continued spread of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a novel highly contagious virus, has promptly spread as a global pandemic. The World Health Organization (WHO) reported in January 2021 that over 12 million people had been infected with SARS-CoV- 2 in Southeast Asia and nearly 200,000 deaths (WHO 2021). Thailand was initially the second country affected worldwide with this pandemic; however, increases in the rate of new cases has slowed down. SARS-CoV-2 testing is provided to individuals in Thailand free-of-charge if they meet the criteria of patients under investigation (PUIs) for COVID-19 applied by the Department of Disease Control, Thailand (DDC 2020).
Recent studies have found that the duration of virus shedding differs between individuals, ranging from 0-20 days after the onset of symptoms (van Kampen, van de Vijver et al. 2021). Among mild COVID-19 cases in China, SARS-CoV-2 RNA could be detected in throat swab samples at a median of 15.6 days after symptom onset (95% CI 11.8-20.7) (Sun, Xiao et al. 2020), while it was 14 days (range 9-26 days) in Thailand (Pongpirul, Mott et al. 2020). In addition, prolonged RNA detection was found in some individuals who had recovered (Park, Yun et al. 2020). However, the management of these prolonged cases is difficult in some settings, and the WHO has updated the criteria for asymptomatic cases who still test positive for COVID-19 are able to be discharged from isolation at day 10 after a positive test for SARS-CoV-2 (WHO 2020). Since they are discharged from the hospital, these criteria may put them at high risk for discontinuation of case monitoring, which might be a source of viral spread in the community. In this report, we demonstrated, for the first time, prolonged detection of SARS-CoV-2 RNA in a Thai female without clinical symptoms who had the possibility of transmitting the virus to her husband.
MATERIALS AND METHODS
The nasopharyngeal and throat swab specimens of a 30-year-old Thai female from Lamphun Hospital, Lamphun, Thailand, were tested for the presence of SARS-CoV-2 RNA as a required protocol prior to the performance of dental procedures by two real- time reverse-transcription-polymerase-chain-reaction (RT-PCR) assays (Da An Gene 2019-nCoV-2 RT-PCR, Guangdong, P. R. China and DMSc COVID-19 Real-Time RT-PCR Kit, Bangkok, Thailand) at the Associated Medical Sciences-Clinical Service Center (AMS-CSC), Chiang Mai University, Chiang Mai, Thailand. Total IgM/IgG COVID-19 antibody was determined by the WANTAI SARs-CoV-2 Ab Rapid Test, Beijing, China (100% sensitivity and 98.8% specificity). Based on this method, anti-SAR-CoV-2 IgM and IgG antibodies were detected in the same reaction line. Another rapid test kit (Acro Biotech COVID-19 Rapid POC CE-IVD Test, CA, USA) was used for confirmation. Based on this method, IgM and IgG antibodies were detected on separated lines with 85% sensitivity and 96% specificity for IgM, while there was 100% sensitivity and 98% specificity for IgG. According to the manufacturer's protocols, both rapid tests were considered positive in cases when the test zone IgM and/or IgG showed colored lines or weakly positive if the lines were faint. The results from these tests may be interpreted as the patient having been exposed to SAR-CoV-2, even weakly positive results were shown. Moreover, a complete blood count (CBC) was performed using an automated cell counter (SIEMEN ADVIA 2120i, Siemens Healthcare Diagnostics, Tarrytown, NY, USA).
RESULTS
On July 17, 2020, the 30-year-old Thai female was positive for SARS-CoV-2 RNA by RT-PCR. Unexpectedly, her past medical history indicated that she had been found positive for SARS-CoV-2 RNA since March 30, 2020 (Table 1). From the medical record, due to close contact with her colleague who was a confirmed COVID-19 case, she and her husband, a 31-year-old Thai male, had been tested at Lamphun Hospital for SARS-CoV-2 infection. Only she was positive for SARS-CoV-2 RNA by RT-PCR and was admitted to Lamphun Hospital since then without any clinical symptoms (i.e., fever, dry cough, or fatigue), except allergic rhinitis as her underlying disease. During hospitalization, she was prescribed one tablet of loratadine 10 mg and two tablets of fexofenadine HCl 60 mg according to her allergic symptoms. On April 13, 2020, she was continually found positive for SARS-CoV-2 RNA. Later, on April 27, 2020, she was still found positive for SARS-CoV-2 RNA and also positive for anti-SARS-CoV-2 IgM/IgG antibody without any clinical symptoms of COVID-19. Then, she was discharged from the hospital and was lost to follow-up.
Table 1. Time until clearance and the tests
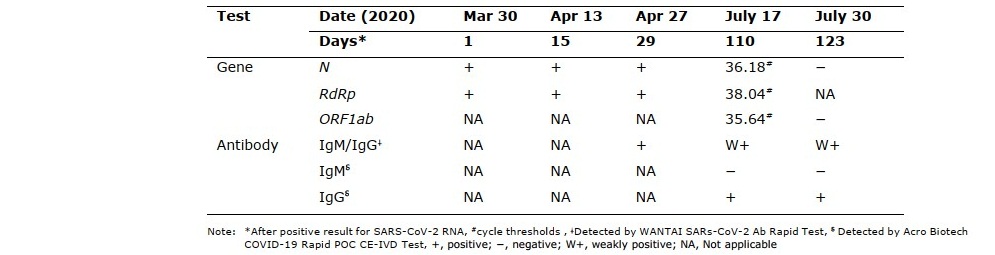
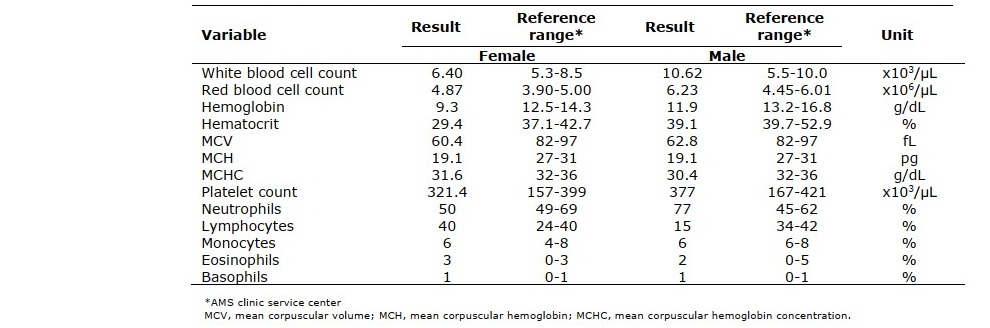
On July 17, 2020 (day 110), surprisingly, she remained positive for SARS-CoV-2 RNA and anti-SARS-CoV-2 IgG antibody without any clinical symptoms. However, the cycle thresholds (Ct) of the N, RdRp, and ORF1ab genes were 36.18, 38.04, and 35.64, respectively, which are close to a Ct of 40, the cut-off point for negative values (Table 1). Therefore, she and her husband were invited to be examined on July 30, 2020 (day 123). She was negative for SARS-CoV-2 RNA, while her anti-SARS-CoV-2 IgG antibody remained positive. Her husband was still negative for both SARS-CoV-2 RNA and antibodies. These results implied that no transmission to her husband occurred, even though she had prolonged persistence of SARS-CoV-2 RNA. From CBC data (Table 2), she had normal values of white blood cells and differential cell types, which means no sign of infection, while her husband had slightly increased values of white blood cells and neutrophils, possibly indicating inflammation or bacterial infection. Moreover, they had a microcytic anemia due to their low levels of mean corpuscular volume (MCV) and mean corpuscular hemoglobin (MCH) (Table 2), which are commonly found in iron deficiency anemia and thalassemia carriers (Lemmens-Zygulska, Eigel et al. 1996).
Table 2. Complete blood count results of the case and her husband on July 30, 2020.
DISCUSSION
As far as we know, this is the first asymptomatic case to show the longest prolonged persistence of SARS-CoV-2 RNA from nasopharyngeal and throat swab specimens in Thailand. Whereas, positive RT-PCR results in nasopharyngeal and throat swab samples were reported for 55 days at maximum from patients who recovered from mild COVID-19 (Sun, Xiao et al. 2020) and 67 days at maximum for symptomatic patients after resolution (Park, Yun et al. 2020). The possible mechanism for this persistency is a balanced coexistence between a low viral load and immune responses of the patients (Carmo, Pereira-Vaz et al. 2020, Cevik, Bamford et al. 2020), leading to less inflammation that could be interpreted as mild forms of infection or asymptomatic cases (Carmo, Pereira-Vaz et al. 2020). Our observation showed no viral transmission between spouses, since the Ct was higher than 24, which indicates low viral replication (< 1 x 106 copies/mL by RT-PCR) and a low risk for viral transmission (Cento, Colagrossi et al. 2020). Therefore, interventions for people with close contacts to this case may not be necessary. However, the practical guidelines from the Center for COVID-19 Situation Administration (CCSA), Thailand, should be strictly followed (i.e., social distancing, mask wearing, handwashing, temperature scanning and self- monitoring) (CCSA 2021). The case in this study had weakly positive total antibodies against SAR-CoV-2 and no clinical symptoms, which correlate to another previous study showing patients with slow viral clearance had a low level of anti-SAR-CoV-2 antibodies and mild symptoms (Carmo, Pereira-Vaz et al. 2020).
To distinguish between remote and new infections, viral gene sequencing should be performed and compared in the initial sample on March 30, 2020, and the last positive sample on July 17, 2020. However, due to the unavailability of the initial specimens, we could not perform viral gene sequencing. In addition, a high Ct value, indicating a low viral load, makes it difficult to perform gene sequencing. Based on serological data, only IgG was detected in this case, suggesting that she had been exposed to the virus for quite some time. On the contrary, the previous study showed that IgM was positive and IgG was negative in the first infection, whereas both IgM and IgG antibodies were detected in the new infection, even though they were asymptomatic in both episodes (Falahi and Kenarkoohi 2020). According to her Ct value and antibody results, this case is likely to be a remote infection.
CONCLUSION
To our knowledge, we reported the first asymptomatic COVID-19 case in Thailand who had the longest prolonged persistence of SARS-CoV-2 RNA, with a low level of viral replication. No evidence of viral transmission was observed among her close contacts. The information in this report could be combined with additional data sources to raise public health awareness with regard to clinical management.
ACKNOWLEDGMENTS
We thank Ms. Jiaranai Khantipong from Office of Disease Prevention & Control 1 Chiang Mai for supported information.
AUTHOR CONTRIBUTIONS
Chidchamai Kewcharoenwong wrote the manuscript. Woottichai Khamduang and Sakorn Pornprasert reviewed the manuscript. Sirintra Kwunchoo, Kesinee Chantawiang, Piyapong Pinta, Sarik Promarat and Bunleng Punchaburi provided patient’s clinical information. All authors have read and approved of the final manuscript.
CONFLICT OF INTEREST
The authors declare that they hold no competing interests.
REFERENCES
Carmo, A., Pereira-Vaz, J., Mota, V., et al. 2020. Clearance and persistence of SARS- CoV-2 RNA in patients with COVID-19. J Med Virol. 92: 2227-2231.
CCSA. 2021. Covid-19 Situation Administration Center (In Thai) from http://www.moicovid.com/.
Cento, V., Colagrossi, L., Nava, A., Lamberti, A., Senatore, S., Travi, G., Rossotti, R., Vecchi, M., Casati, O., Matarazzo, E., et al. 2020. Persistent positivity and fluctuations of SARS-CoV-2 RNA in clinically-recovered COVID-19 patients. J Infect. 81: e90-e92.
Cevik, M., Bamford, C.G.G., and Ho, A. 2020. COVID-19 pandemic-a focused review for clinicians. Clin Microbiol Infect 2020; 26: 842-847.
DDC, T. 2020. "Case definition for patients under investigation (PUIs) with COVID-19 (edited on March 2, 2020)." From https://ddc.moph.go.th/viralpneumonia/ eng/file/guidelines/G_PUIdefinition.pdf.
Falahi, S. and Kenarkoohi, A. 2020. COVID-19 reinfection: prolonged shedding or true reinfection? New Microbes New Infect. 38: 100812.
Lemmens-Zygulska, M., Eigel, A., Helbig, B., Sanguansermsri, T., Horst, J. and Flatz, G. 1996. Prevalence of alpha-thalassemias in northern Thailand. Hum Genet. 98: 345-347.
Park, S.Y., Yun, S.G., Shin, J.W., Lee, B.Y. , Son,H-J., Lee, S., Lee, E., Kim, T.H. 2020. Persistent severe acute respiratory syndrome coronavirus 2 detection after resolution of coronavirus disease 2019-associated symptoms/signs. Korean J Intern Med. 35: 793-796.
Pongpirul, W.A., Mott, J.A., Woodring, J.V., Uyeki, T.M., MacArthur, J.R., Vachiraphan, A., Suwanvattana, P., Uttayamakul, S., Chunsuttiwat, S., Chotpitayasunondh, T., et al. 2020. Clinical Characteristics of Patients Hospitalized with Coronavirus Disease, Thailand. Emerg Infect Dis. 26: 1580- 1585.
Sun, J., Xiao, J., Sun, R., Tang, X., Liang, C., Lin, H., Zeng, L., Hu, J., Yuan, R., Zhou, P., et al. 2020. Prolonged Persistence of SARS-CoV-2 RNA in Body Fluids. Emerg Infect Dis. 26: 1834-1838.
van Kampen, J.J.A., van de Vijver, D., Fraaij, P.L.A., Haagmans, B.L., Lamers, M.M. Okba,N., van den Akker, J.P.P.C., Endeman, H., Gommers, D.A.M.P.J., Cornelissen, J.J., et al. 2021. Duration and key determinants of infectious virus shedding in hospitalized patients with coronavirus disease-2019 (COVID-19). Nat Commun. 12: 267.
WHO. 2020. "Criteria for releasing COVID-19 patients from isolation." from https://www.who.int/news-room/commentaries/detail/criteria-for-releasing- covid-19-patients-from-isolation.
WHO. 2021. "WHO Coronavirus Disease (COVID-19) Dashboard." from https://covid19.who.int/.
OPEN access freely available online
Chiang Mai University Journal of Natural Sciences [ISSN 16851994]
Chiang Mai University, Thailand https://cmuj.cmu.ac.th
Chidchamai Kewcharoenwong1, Woottichai Khamduang1, Sirintra Kwunchoo2, Kesinee Chantawiang2, Piyapong Pinta2, Sarik Promarat2, Bunleng Punchaburi2, And Sakorn Pornprasert1,*
1 Department of Medical Technology, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand.
2 Lamphun Hospital, Lamphun, Thailand
Corresponding author: Sakorn Pornprasert, E-mail: sakornmi001@gmail.com
Total Article Views
Editor: Korakot Nganvongpanit, Chiang Mai University, Thailand
Article history:
Received: January 10, 2021;
Revised: February 8, 2021;
Accepted: February 15, 2021;
Published online: March 18, 2021

