
Development of Collaborative Diabetes Management in Communities
Thanakamon Leesri*, Taweeluk Vannarit, Wichit Srisupan,Wilawan Senaratana and Kittipan RerkasemPublished Date : 2019-08-24
DOI : 10.12982/CMUJNS.2015.0090
Journal Issues : Number 3, September - December 2015
ABSTRACT
Diabetes is on constant rise worldwide as regards both its prevalence rate and related complications: persons affected with diabetes suffer from physiological, psychosocial, and economic consequences. This study aimed to increase community collaboration among diabetics to deal with the problem of diabetes and to develop and measure the effective diabetes management via mutual-collaborative action research. The core working group represented 60 participants from local community leaders, persons with diabetes, family caregivers, village health volunteers, healthcare providers, and other interested community residents. The five-step development procedure was composed of community preparation; community needs assessment; collaborative planning; implementation; and continuous monitoring and evaluation. The qualitative methods of data collection consisted of focus group discussions, in-depth interviews, and participatory observation. The content analysis utilized all the data assembly. The Collaborative Diabetes Management [CDM] method composed of six components, including 1) local capacity building, 2) municipality government policy, 3) diabetic management curriculum and community advocacy, 4) maximized used of community social capital, 5) community care and support, and 6) lessons learned sharing. The processes and the outcome measurement were to increase all the community capabilities and the impacts of all collaborative diabetes management components. Moreover, the number of participants whose HbA1C could be controlled after participating in the CDM program was significantly different from the number of participants whose HbA1C could be controlled before participating in the CDM program (χ² = 10.971, p<0.05). The percentage of persons who can control the blood sugar level different in 25% (3 persons) increased to 92% (11 persons) after participated in CDM program. Consequently, the CDM encouraged all the local community organizations and the community members to utilize the collaborative diabetic management by community participation as a significant method with individuals and group participants by effectively engaging stakeholders based on their community context, thereby triggering a movement in the direction of community practice, nursing education, local health policy, and future research. It still requires continued community collaborative management by including community members, local organizations, and healthcare providers.
Keywords: Collaborative, Diabetes management, Community
INTRODUCTION
Diabetes is a significant non-communicable disease, and it affects the health of people worldwide (World Health Organization [WHO], 2010). Globally, the number of adults with diabetes in 2010 was 285 million, with a prevalence percentage of 6.4%. By the year 2030, this number is estimated to be 439 million
with a prevalence of 7.7% (Shaw, Sicree, & Zimmet, 2010). Diabetes and its complications produce physiological, psychosocial, and socioeconomic impacts (American Diabetes Association [ADA], 2013). Also, in Thailand, a developing country, diabetes has been a major cause of morbidity and mortality in the past decade. The high prevalence rate of diabetes in Thailand places it among the top ten in Asia (Chan et al., 2009). A prevalence of 6.7% was reported in adults aged over 15 years, of whom 53.3% were undiagnosed (Aekplakorn et al., 2011). The various interventions that enhanced the diabetic person’s ability to achieve diabetic control have been well-documented. These interventions focused on the collaboration between persons with diabetes, between their families, and between the communities (AADE, 2009; Dean, 2012; Mendenhall & Doherty, 2006; Peek, Cargill, & Huang, 2007). However, the number of persons with diabetes who are able to keep the blood sugar in control is still low; in addition, the number of persons with diabetes who experience complications has increased (Nitiyanant et al., 2007 and Shaw, Sicree, & Zimmet, 2010). Therefore, there are some limitations to the previous interventions in promoting the ability of persons with diabetes and their families as well as communities to perform continuous and sustainable actions.
In order to achieve the implementation of effective development strategies through active engagement with, and participation from, all stakeholders at individual, family, community, societal, and national levels. This ultimately led to a health system of sufficiency and a happy and peaceful society (The Office of the National Economic and Social Development Board, 2012). Thus, the management for diabetes should be developed from the participation of each group’s competency. As far as sustainable management of diabetes is concerned, the development of continuous interventions and decision-making based on strategy-sharing will give rise to collaborative management which is effective for diabetes management in a community setting (Quinlan & Robertson, 2010, and Takahashi et al., 2001). Accordingly, the effective strategies required to develop effective interventions, by enhancing skills and building competencies for community capacity by promoting community participation applied as a form to ascertain diabetes management in a community setting, based on the research on the most appropriate method of action.
The primary objective aimed to develop effective methods to increase community collaboration to deal with the problem of diabetes and to develop effective diabetic management by using mutual-collaborative action research. And the secondary was to evaluate risk factor control outcomes including blood sugar, blood pressure, and lipid profiles. The knowledge derived from this study may enable persons with diabetes, their family caregivers, and the community and healthcare providers to clearly define their practice in order to promote appropriate education, attitude, skills, and practice. Diabetic management was conducted as an interactive planning activity, including implementation, and both the processes and the outcomes were evaluated. The related research questions were as follows: what are the components of collaborative diabetes management in a community? and whether the collaborative diabetes management can improve blood sugar, blood pressure, and lipid profiles?
Focused on collaboration, it is a mutually beneficial and well-defined relationship between two or more organizations to achieve common goals. The relationship includes a commitment to mutual relationships and goals; a jointly developed structure and shared responsibility; mutual authority and accountability for success; and sharing of resources and rewards (Parkinson, 2006). Therefore, it was the mutual-collaborative action research that guided this diabetes management method which is integrated with the community participation concept for triggering the processes of collaborative diabetes management in a community setting.
Low-sugar volunteers (LSVs) were defined as representative persons from community members who volunteered to participate in all the processes of a collaborative diabetes management (CDM) development program. They were composed of 15 village health volunteers, 12 persons with diabetes, 12 family caregivers, 1 municipal member, 2 leaders of community groups, and 2 healthcare providers, in addition to 1 community member.
MATERIALS AND METHODS
The mutual-collaborative action research was employed for developing a method for collaborative management of problems related to diabetes for 12 months during the period from October 2012 to September 2013.
This study was reviewed and approved by the Research Ethics Review Committee, Faculty of Nursing, Chiang Mai University.
Participants consisted of persons who live in Sannameng Municipality, Sun-Sai district, Chiang Mai province, Thailand. There were three groups of participants: community stakeholders, core working group, and community residents. First, the community stakeholders, who were called the “advisory board committee,” consisted of local government administrators, healthcare providers, religious leaders, village health volunteers, family caregivers of diabetics, diabetic support groups, and persons with diabetes. Second, the core working group, called “low-sugar volunteers,” was composed of 15 village health volunteers, 12 persons with diabetes, 12 family caregivers, 1 municipal member, 2 leaders of community groups, and 2 healthcare providers, in addition to 1 community member, and they were willing to participate in all the processes of the study. Finally, the other community residents, and they were the other people in the community to be affected by the diabetes management activities.
The researchers prepared the knowledge and the skills in the qualitative method in the nursing research regarding participation action research and mutual-collaborative action research as well as, simultaneously, took on the role of research facilitators, coordinators, and leaders. An interview guide for the focus group using semi-structured interviews was developed by the researcher, and verbatim transcribing from the dialogues sessions in the community assessment, model development, and process evaluation. Also, an observation guide was used when the researcher participated in community events and during project activities.
Triangulation technique was used for gathering the information from different sources: multiple data sources through focus group discussions, semi-structured interviews, group brainstorming, field notes, and participant observation, member checking which allows participants to check and verify the accuracy of the information recorded. This study was concerned about the quality of the information and assures an accurate reflection of how the participants feel and think about the topic by using a moderator who is trained to listen carefully to participants, observe how they answer, and seek clarification on areas of ambiguity. Especially, at the conclusion of each focus group, the researcher asked the participants to verify the summary comments.
For achieving effectiveness in the management of diabetes in the community, the procedures of the data collection were integrated between community participation and community organizing with capacity-building processes. Before beginning the development process, the researcher proceeded to build trust with all the community members by immersing herself into every local community activity and traditional ceremony as well as by participating in all local formal and informal community meetings. Recognizing the importance of working within an integrated strategic development technique, the management process was made to consist of five continuous phases: phase 1) the preparation for building trust with the community; phase 2) Community Needs Assessment for establishing the current situation; phase 3) collaborative diabetes management planning; phase 4) implementation in order to achieve the goals; and phase 5) continuous monitoring and evaluation for feasibility, appropriateness, and effectiveness management. The research processes are illustrated in Figure 1.
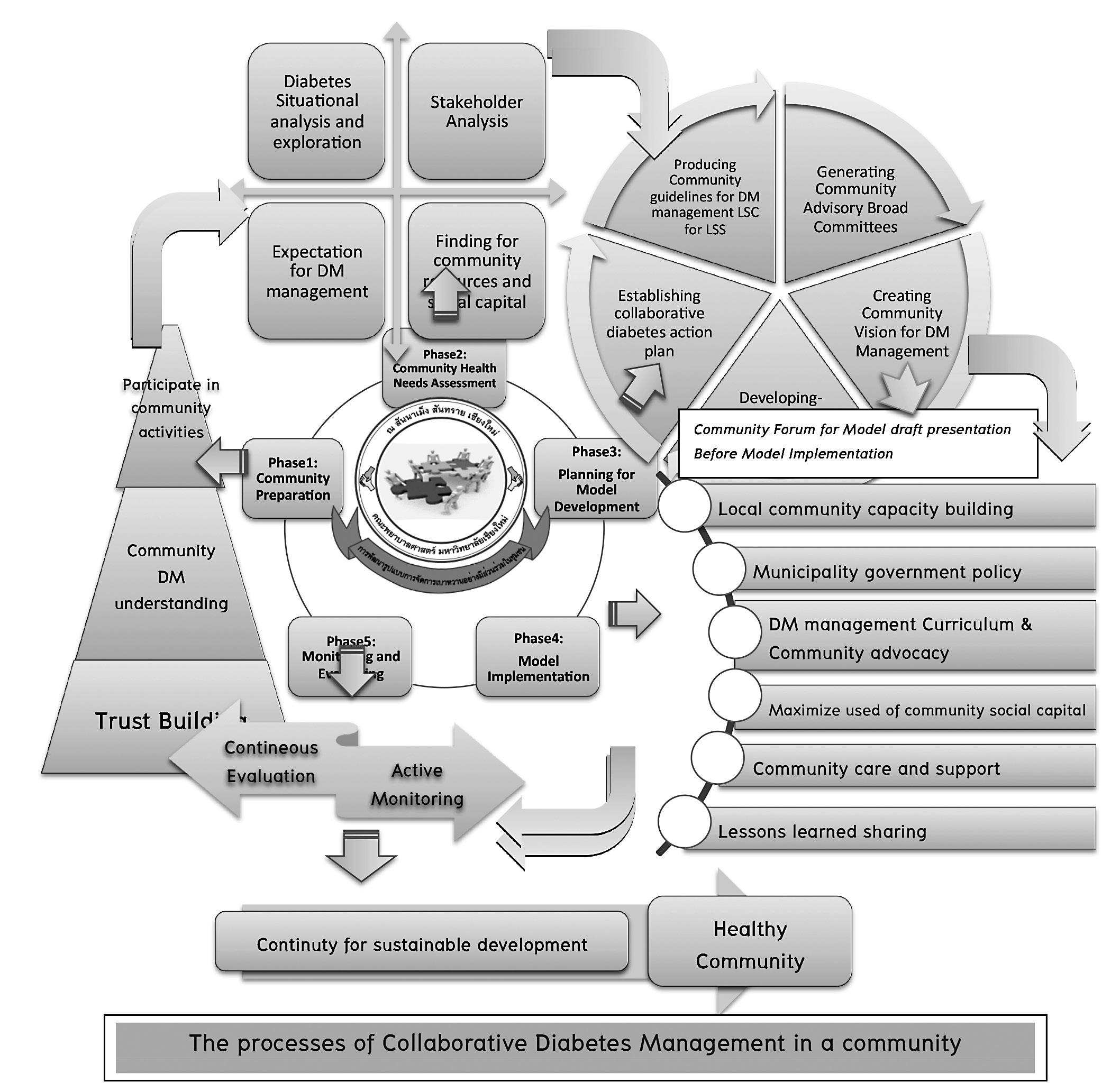
Figure 1. The processes of collaborative diabetes management in the community.
Content analysis was employed to analyze and classify words or statements from the target group’s voice while the group members gave their opinions during focus group discussions and semi-structured interviews. Chi-Square test was used to compare the number of subjects whose HbA1C, systolic blood pressure, diastolic blood pressure, and LDL could be controlled before and after participation in the CDM processes.
RESULTS
The six important components of the CDM development method are as the following: 1) local community capacity building; 2) municipal government policy; 3) community care and support; 4) maximized use of community social capital; 5) DM curriculum and community advocacy; and 6) lessons learned sharing. Each component was elaborated as follows and shown in Figure 2:
Component I: Local community capacity building
Bottom-up organizing is composed of four steps: 1) raising the awareness of community diabetes management; 2) formulating and empowering effective core working groups Low-Sugar Volunteers [LSVs]; 3) generating community commitment for diabetes management; and 4) imparting training in the essential skills.
Component II: Municipal government policy
The local organization, Sannameng Municipality, collaborated to conduct a community health policy, namely a five-year plan for community health, community vision and missions for diabetes management, and community guidelines for diabetes management in the community for establishing and developing the Innovative Health Promoting School. At the same time, local organizations provided valuable resources including budget allocations, public meeting places, health personnel, and other community resources.
Component III: Community care and support
The various effective techniques included the use of more actual existing community resources, performance by all community members, and support from local advisory board committees. In this study, the researcher and the LSVs together organized community groups supporting all the community activities which consisted of the following: the senior and junior low-sugar volunteer (LSV) systems, family support core group, integrated home visit team, community group performance, and moral support from the community for low-sugar persons.
Component IV: Maximized use of community social capital
According to Northern Thai tradition, most community residents are Northern Thai people. They usually speak the local dialect, and share other northern cultures and norms, besides sharing the Lanna-CD (the entire media ensemble produced in local dialect was entitled “Low-sugar: JOY-SAW”), Dharma speaking for health, and the mobile clinic for diabetes screening.
Component V: Diabetes management curriculum and community advocacy
Initially, the researcher together with the LSVs established the innovation of the low-sugar curriculum for the low-sugar school, aimed at community diabetes management guidance. This curriculum consisted of five modules, namely 1) the overview of the diabetes disease, 2) nutrition, 3) physical activities, 4) religious local culture and wisdom, and 5) sufficiency economy and organic farming. Mainly, the manual of the CDM program intended to guide for responsibility and assist their opinions and necessities. Correspondingly, the manual of collaborative management was created, proposing self-management for persons with diabetes and their family caregivers.
The researcher together with the LSVs drew up the diabetes-community map which indicated the location of each diabetic person’s house in the community area, and compiled a diabetes-community registration which provided the patients’ relevant information. Also, a mobile low-sugar school was established in every community setting. The researcher, together with the LSVs provided this activity as an aid for persons who cannot receive particular forms of management at the municipal public health center. Finally, as part of the monitoring activities system, the researcher together with the LSVs provided low-sugar bags for transporting the diabetes-community map, diabetes-community registration details, Lanna-CD, and manuals for community diabetes management. All the LSVs use these bags every time they give education on diabetes to other persons with diabetes in the community.
Component VI: Lessons learned sharing
The researcher together with the local organization and the core working groups (LSVs) collaboratively summarized the lessons learned from every activity. The various themes developed included the following: oral presentation, low-sugar community welfare days, honor ceremony for low-sugar volunteers and opening of an innovative health promoting school, the “Masterpiece Multimedia Presentation” by http://www.youtube.com/watch?v=6897tUiIM4Q, the memorandum of understanding (MOU) signing for Sannameng Declaration for diabetes management, local organization networking by www.sannameng.net, www.localchiangmai.co.th, and http://www.chiangmainews.co.th/page/?p=218918, and social media sharing such as the use of local newspaper.
After cooperative evaluation for sustainable development, the researcher and the LSVs presented the successful project outcomes and impacts to the local government organization and sent a referral for the development of sustainable local community activities for diabetes management. All the activities since the beginning of the project development to the final activities that all the community members established together were presented by the researcher and the LSVs. Before sending the referral information, the researcher and the LSVs created a yearly diabetes management activity calendar to monitor all the performances related to diabetes in the community. This calendar provided the convenient time allocations for community health management events and presented a summary of all the community activities for the whole year.
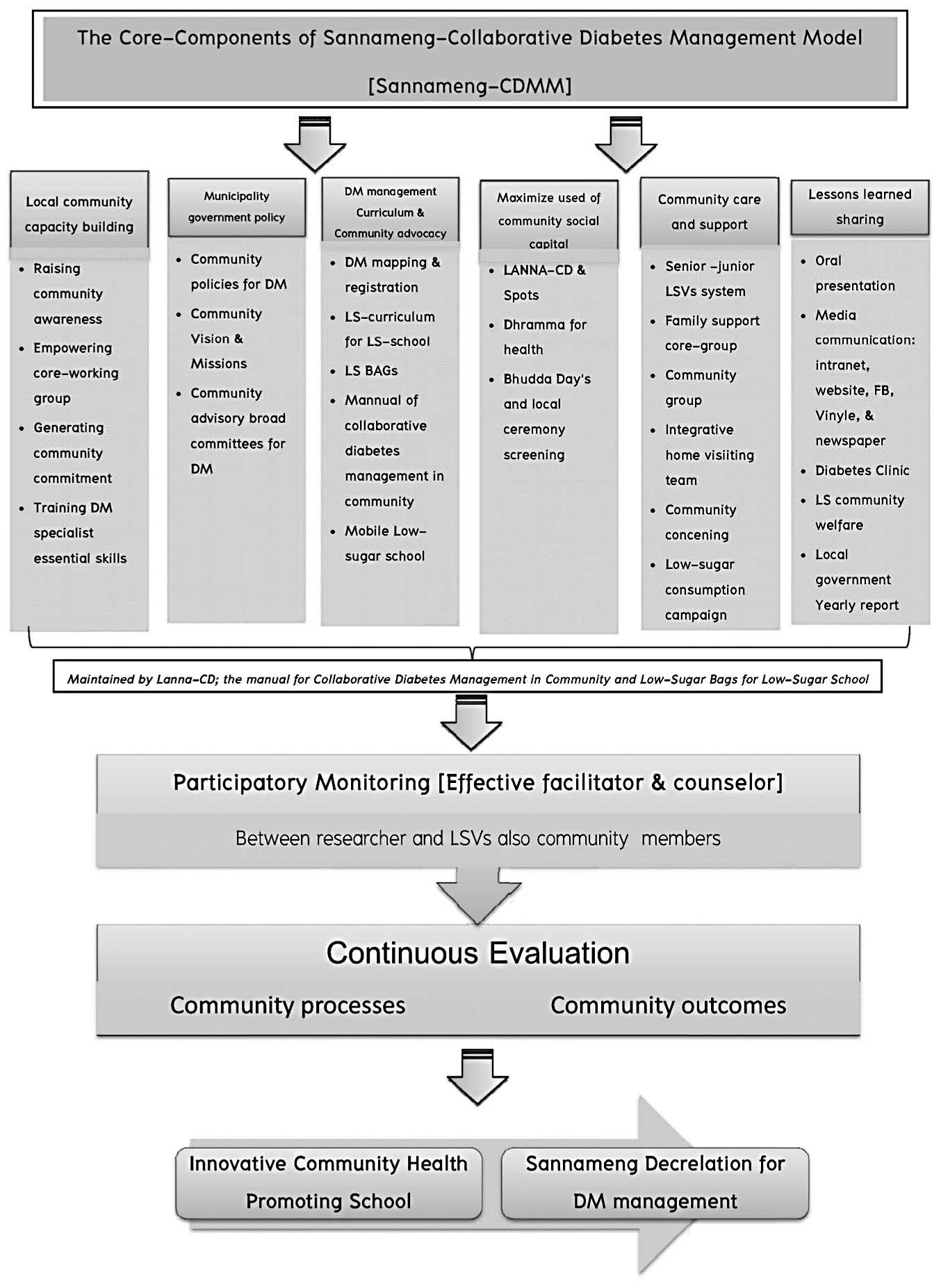
Figure 2. The six components of collaborative diabetes management in community.
For the effectiveness of the CDM development process evaluation, the results are presented as the difference between before and after participation in the CDM development program in 12 months from 12 persons with diabetes representative of the LSV group. The results of the HbA1C, blood pressure, and LDL level from 12 persons with the diabetes who represented all person of participants, perfect set of sample size, can be measured based on inclusion criteria and participated in all 5 processes CDM development. Moreover, participants cannot be increased more because others did not be participated in this study in 12 month development. The outcomes of this study were benchmark with the Standard of Medical Care in Diabetes (American Diabetes Association, 2013) included the HbA1C level to be less than 7%, the systolic blood pressure to be less than 130 mmHg, the diastolic blood pressure to be less than 80 mmHg, and the LDL level to be less than 100 mg/dL. Among the 12 persons with diabetes, 7 were women (58.33%), and the average age was 60 years (SD = 8.58) (range = 47–82). the percentage of persons who can control the blood sugar level different in 25% (3 persons) increased to 92% (11 persons) after participated in CDM program. The comparative results are presented in Table 1, as follows.
Table 1. Comparison of numbers of participants whose HbA1C, systolic blood pressure, diastolic blood pressure, and LDL could be controlled before and after participation in CDM program (n=12)
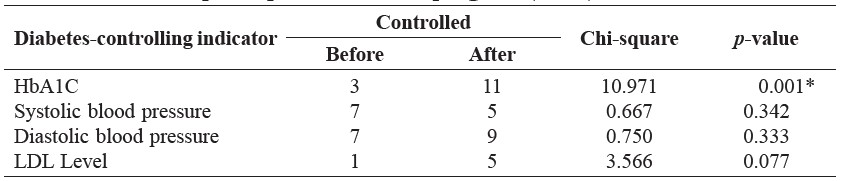
Note: *P < .05 (Fisher’s exact test = 10.971).
Compare the differences in the HbA1C, systolic blood pressure, diastolic blood pressure, and LDL values of the participants before and after participation in the CDM program by using the Chi-square values.
The analysis results demonstrate that the number of participants whose HbA1C could be controlled after participation in the CDM program was significantly different from the number of participants whose HbA1C could be controlled before participation in the CDM program (χ² = 10.971, p<0.05). However, participants whose systolic blood pressure, diastolic blood pressure, and LDL level could be controlled were observed to be not significantly different.
DISCUSSION
This CDM program was developed based on mutual-collaboration action research aimed at developing a sustainable diabetic management method appropriate in the context of the community. All the community activity development processes were created through collaboration between the researcher and the community members. The significant features of an effective diabetes management technique are the need of the community participants to be individually empowered to participate in their own diabetes management and allocation of specific times as well as the budget to support the process activities. Importantly, most of the major community stakeholders were identified and encouraged to participate in all the steps of the program because of their deep understanding of their community context and the community diabetes style as well. Moreover, the integration of diabetes management strategies with local community lifestyle in addition to the creative presentation of the alternative activities based on their community contexts produced the desired result in the form of continuous participations. They were empowered by raising community awareness related to diabetes, encouraging the community participants to share and learn, building specific capacities as regards keeping diabetes in control, establishing corporate-networking & facilitating and providing consultant activities related to diabetes management in the community as required. The effectiveness of CDM was presented as the increased the controlled blood sugar. However, it cannot be improved in blood pressure (both Systolic and Diastolic) and LDL Level. Consistent with the suggestions from ADA 2013, it should be used medication therapy incorporated with behavioral modification to manage blood pressure and lipid profile among persons with diabetes.
As for the outcomes of the CDM process development in the community, the community stakeholders had gained more knowledge, information, perceptions, attitudes, beliefs, skills, experiences, practices, confidence, and resources. Also, the CDM program encouraged local organizations and community residents’ collaborations to conduct activities for diabetic managing. This community wasopen for all community members who would be influenced by diabetes management, including persons with diabetes, their family caregivers, local healthcare providers, and other people who were in need of undertaking diabetes management activities through community collaboration. The collaboration between local organizations and community citizens provided the means for all community stakeholders to participate fully in the research process. This collaboration was an important foundation for successful diabetes management intervention, which included practical activities for effective diabetes management and establishing of a healthy community. Additionally, sustainability of the activities is the ultimate goal of any community health project. Meister and De Zapien (2005) pointed out that social action focuses on policy development that can subsidize collaborative efforts and enhance continued sustainability. These activities provide a platform for all community participants to raise their concerns and cooperate in local community movements, as well as to present effective diabetes management strategies. Importantly, in our study, they provided the integration with community traditions and their lifestyle which was in congruence with the study by Heritage & Dooris (2009) that contributed to sustainable development. Also, community action strategies have significant impacts on the physical and social determinants of health across the local organization and community involved. Of much importance is the conclusion by Swerissen & Crisp (2004) the level of sustainable effects from each intervention including individual level via information, education, and training. These produced individual changes and had little impact on behavioral outcomes. Organizational level interventions through organizational policies effect on changes in rules, roles, sanctions, and incentives. These produced changes in individual behaviors that offer greater access to social, educational, and health resources that promote better health and had a great impact on individual actions as well as changes in the physical environment. Next, community level actions focused on social action and social planning to create new settings (groups, clubs, organizations, networks, and partnerships) producing changes in organization and redistribution of resources to affect health also increase the impact on individual actions and settings, which may have pervasive effects on individuals and evidence of sustainability. Finally, an institutional change with emphasis on social advocacy to change legislative institutional settings that have effects at community, organizational, and individual levels has an extremely high impact on a wide range of settings, and, thereby, on the physical environment, and, eventually, individual action is achieved through institutional change.
Additionally, short-term success contributes to long-term effectiveness of local activities. Long-term sustainability of this CDM program should be continued to develop in the future through reimplementation of all the processes of development, thereby contributing to more effective collaboration management. Similarly,
the CDM components were in accordance with those in the study of Ibrahim et al. (2002) and Doherty & Mendenhall (2006) which related to the degree of the community change involvement, and they included the following: 1) Community meetings, meetings of the heads of communities, and community board settings generated community awareness. 2) Interactive community meetings, community presentations, etc. produced local information dissemination which established community understanding. 3) Community workshops, role models, community teaching sessions, action leaders’ groups as well as distribution finding created community support. 4) Multidisciplinary team action, empowering, encouraging, continuous feedback, promoting participation, and capacity building developed community involvement. 5) Changing in the community lifestyle or members’ daily life enhanced community commitment.
In order to evaluate the effectiveness of the CDM techniques, the four indicators that control diabetes, namely HbA1C, systolic blood pressure, diastolic blood pressure, and LDL, were measured before and after participation in the CDM program. The results demonstrated that the number of participants whose HbA1C could be controlled after participation in the CDM program was significantly higher than the number of participants whose HbA1C could be controlled before participation. This proves and establishes the fact that the CDM program was effective in enhancing the self-management of the participants. This is the reason why they were able to manage their diabetes-controlling activities which consisted of exercises, dietary control, and stress management. In other words, it can be inferred that behavioral modification mainly resulted in HbA1C.
However, there was no significant difference in the number of participants whose systolic blood pressure, diastolic blood pressure, and LDL could be controlled. This may be because the reason that behavioral modification is not the only means of effecting changes on these indicators. They may be influenced by other factors that were not included in this study.
CONCLUSION
The objective of the study was the development of a Collaborative Diabetes Management (CDM) program aimed to encourage all local community organizations and community members based on mutual-collaborative action research. The community capacity building approach using significant methods effectively engaged individuals, group participants, and stakeholders to collaboratively explore, plan, implement, monitor, and evaluate their own diabetes situations for effective management in the context of their community. Furthermore, the research findings suggest directions for community practice, nursing education, local health policies, and future research. The findings could be applied in nursing practices, especially in repetition of nursing in communities including the development of CDM programs in other communities, and in providing diabetic management activities to meet community policies. In the same manner, the possibilities for the promotion of collaborative community approaches for other health situations or community problems should be analyzed and added to the contribution.
ACKNOWLEDGMENT
The Office of the Higher Education Commission (OHEC), Thailand, is acknowledged for its support in the form of research grant. Professor Kittipan Rerkasem was supported by the National Research University Project under Thailand’s Office of the Higher Education Commission (OHEC).
REFERENCES
Aekplakorn W., P. Putwatan, S. Chariyalertsak, S. Taneepanichskul, P. Kessomboon, R. Sangthong, R. Inthawong, and The Thai National Health Examination Survey Study Group. 2011. Prevalence and Management of Diabetes and Metabolic Risk Factors in Thai Adults: The Thai National Health Examination Survey IV, 2009. Diabetes Care; 34 (9):1980-1985. doi: 10.2337/dc11-0099
American Association Diabetes Educators. 2009. Diabetes Community Health Workers. The Diabetes Educator, 29(5), 818-824.
American Diabetes Association. 2013. Standard of Medical Care in Diabetes-2013. Diabetes Care, 36(1), s11-s61. doi: 10.2337/dc13-S011
Chan J.C.N., V. Malik, W. Jia, T. Kadowaki, C.S. Yajnik, K.H. Yoon, and F.B. Hu. 2009. Diabetes in Asia: Epidemiology, Risk Factors, and Pathophysiology. The Journal of the American Medical Association; 301 (20), 2129-2140.doi: 10.1001/jama.2009.726
Dean J.D. 2012. Management of diabetes in the community. Diabetes in Practice, 38(12): 686-898.
Doherty W.J., and T.J. Mendenhall. 2006. Citizen Health Care: A Model for Engaging Patients, Families, and Communities as Co-producers of Health. Families, Systems, and Health, 24(3), 251-263. doi: 10.1037/1091-7527.24.3.251
Heritage Z., and M. Dooris. 2009. Community participation and empowerment in Healthy Cities. Health Promotion International.; 24 Suppl 1:i45-i55. doi: 10.1093/heapro/dap054.
Ibrahim I.A., J. Sidorov, R. Gabbay, and L. Yu. 2002. Measuring Outcomes of Type 2 Diabetes Disease Management Program in an HMO Setting. Southern Medical Journal, 95(1), 78-87.
Meister J.S., and J.G. De Zapien. 2005. Bringing Health Policy Issues Front and Center in the Community: Expanding the Role of Community Health Coalitions. Preventing Chronic Disease; 2(1), 1-7.
Mendenhall T.J., and W.J. Doherty. 2007. Partners in Diabetes: Action research in a primary care setting. Action Research; 5(4), 378-406. doi: 10.1177/1476750307083722
Nitiyanant W., T. Chetthakul, P. Sang-A-Kad, C. Therakiatkumjorn, K. Kunsuikmengrai, and J.P. Yeo. 2007. A survey study on diabetes management and complication status in primary care setting in Thailand. Journal of the Medical Association of Thailand, 90(1), 65-71.
Parkinson C. 2006. Building Successful Collaborations: A guide to collaboration among non-profit agencies and between non-profit agencies and businesses. Cambridge & North Dumfries Community Foundation.
Peek M.E., A. Cargill, and E.S. Huang. 2007. Diabetes Health Disparities: A systematic Review of Health Care Interventions. Medical Care Research and Review; 64(5), 101s-156s. doi: 10.1177/1077558707305409
Quinlan E., and S. Robertson. 2010. Modeling Dimensions of ‘the Social’ in Knowledge Teams: An Operationalization of Habermas’ Theory of Communicative Action. Sociological Research Online was retrieved from http://www.socresonline.org.uk/15/3/11.html. doi: 10.5153/sro.2189
Shaw J.E., R.A. Sicree, and P.Z. Zimmet. 2010. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Research and Clinical Practice; 87(na), 4-14. doi:10.1016/j.diabres.2009.10.007. doi: 10.1016/j.diabres.2009.10.007
Swerissen H., and B.R. Crisp. 2004.The sustainability of health promotion interventions for different levels of social organization. Health Promotion International; 19 (1); 123-130. doi: 10.1093/heapro/dah113
Takahashi L. M., and G. Smutney. 2001. Collaboration among small communitybased organizations: strategies and challenges in turbulent environments. Journal of Planning Education and Research; 21(2): 141-153.
The Office of the National Economic and Social Development Board Office of the Prime Minister Bangkok, Thailand. 2012. The Eleventh National Economic and Social Development Plan (2012-2016). Office of the Prime Minister, Thailand Government.
World Health Organization. 2010. World Health Statistics: Progress on the health-related Millennium Development Goals (MDGs).
Thanakamon Leesri1*, Taweeluk Vannarit2, Wichit Srisupan2, Wilawan Senaratana2 and Kittipan Rerkasem3,4
1 Faculty of Nursing, Srinakarintawirot University, Bangkok 10110, Thailand
2 Faculty of Nursing, Chiang Mai University, Chiang Mai 50200, Thailand
3 Department of Surgery, Faculty of Medicine, Chiang Mai University, Chiang Mai 50200, Thailand
4 Research Institute for Health Sciences, Chiang Mai University, Chiang Mai 50200, Thailand
*Corresponding author. E-mail: pencilnaja@gmail.com
Total Article Views

