
Effects of a Theory-based Breastfeeding Promotion Intervention on Exclusive Breastfeeding in China
Hongwei Wan, Sujitra Tiansawad*, Susanha Yimyam and Punpilai SriarpornPublished Date : 2019-08-23
DOI : 10.12982/cmujns.2016.0005
Journal Issues : Number1 ,January - April 2016
ABSTRACT
The benefits of exclusive breastfeeding (EBF) are well known; EBF is recommended for the first six months of an infant’s life. However, EBF rates remain low and unsatisfactory in China. This study aimed to investigate the effectiveness of a breastfeeding promotion intervention based on the theory of planned behavior (TPB) to promote long-term exclusive breastfeeding rates among first-time Chinese mothers. A longitudinal, randomized, controlled trial was conducted at Shanghai First Maternity and Infant Hospital in Shanghai, China. The participants were 285 first-time Chinese mothers. The intervention group (n=157) was offered a specially designed nursing intervention program based on TPB, whereas the control group (n=128) received routine nursing care. Data of exclusive breastfeeding practices were collected at 3 days, 6 weeks, and 4 and 6 months postpartum. Data pertaining to breastfeeding mediating factors were collected three times at the first day after birth, 3 days, and 6 weeks postpartum. A Chi-square test and repeated one-way ANOVA were used for the data analysis. The results showed that the intervention group had significantly higher scores than the control group in breastfeeding knowledge, attitude, subjective norm, and perceived control (at least p< 0.01). The rates of exclusive breastfeeding at the different time points of the intervention group (40.1%, 57.3%, 56.7%, and 42.0%) were consistently and significantly higher than those of the control group (10.9%, 29.7%, 15.6%, and 10.2%) (at least p< 0.01). It could be concluded that this theory-based breastfeeding promotion intervention was effective for improving long-term exclusive breastfeeding rates in China.
Keywords: Exclusive breastfeeding, Breastfeeding promotion intervention, Theory of Planned Behavior, Randomized controlled trial
INTRODUCTION
Breastfeeding is a relatively basic means of nourishing a baby that exerts a significant effect on his or her optimal health with the establishment of a lifetime foundation (Oweis et al., 2009). The benefits of breastfeeding, particularly exclusive breastfeeding (EBF), to mothers, children, and societies have been well established (World Health Organization [WHO], 2002). EBF for the first six months has been recommended for the health of infants, because breast milk provides the best nutrients for infants’ optimal growth (WHO, 2002). The WHO and the United Nations Children’s Fund (UNICEF) have put forth an objective to increase breastfeeding rates to 75% in the early periods of an infant’s life, to 50% at 6 months, and to 25% at 1 year of age (WHO, 2002). Despite evidence of the benefits of EBF for at least 6 months, only a limited number of mothers comply with such recommendations (Zhu et al., 2013 and McIsaac et al., 2014 ). Many studies have revealed a growing number of risk factors that may impede a mother’s ability to sustain longer periods of EBF. For instance, demographic factors such as age, education, marital status, and annual income were reported to be significantly associated with breastfeeding duration (McIsaac et al., 2014). In general, married older women with higher education and income were reported to breastfeed for longer (McIsaac, et al, 2014). Other factors, including breastfeeding knowledge and access to related information sources (Tang et al., 2013), attitude (Zhang, et al., 2009 and Jessri et al., 2013), subjective norms (Lynn and Rempel 2004), and self-efficacy or control (Meedya et al., 2014), were positively related to EBF, whereas mothers’ working status or employment was negatively associated with EBF (Yimyam, 2011).
In China, the National Program of Action for Children Development has set a target rate of 80% for EBF at 4 to 6 months in different provinces since the 1990s (Shen, 2008). However, a recent report by the Consumer Association indicated that in 30 Chinese cities, only 28.6% of mothers exclusively breastfed their newborns, 40% fed their babies a mixture of breast milk and formula within the first 6 months, and almost 31.4% did not breastfeed at all (Zhao, 2010). Another survey conducted in three cities in China in 2012 revealed that the EBF rate at 6 months was only 25.2% (Zhu et al., 2014). Recently, a study conducted in Shanghai found that the EBF rate among first-time Chinese mothers at 4 months was 34.1%, and the rate sharply dropped to 3.3% at 6 months (Wan et al., 2015). The findings of these studies have suggested that few cities and provinces in China could meet the WHO goal or the national target rate for EBF. Chinese women cited working as the most common reason to stop breastfeeding. Perceived insufficient breast milk and worrying about the insufficient nutrition of breast milk were also reported as reasons for ceasing breastfeeding (Zhu et al., 2014 and Wan et al., 2015). A recent predictive study among first time Chinese mothers supported that breastfeeding knowledge, attitudes, subjective norms, and perceived control could predict their EBF practice at 4 months postpartum in a positive direction, whereas working status could negatively predict EBF practice (Wan et al., 2015). This means that employed women were more likely to discontinue EBF at 4 months, when their maternity leave ended. Three of these predictors – attitudes, subjective norms, and perceived control – are major components of the theory of planned behavior (TPB) (Ajzen, 1991) that is one of the most widely employed theories in behavior change studies. According to TPB (Ajzen, 1991), a person’s favorable or positive attitude towards a behavior and beliefs that significant others will approve the behavior (subjective norms) will drive the person’s intention to subjective norms, and perceived control – are major components of the theory of planned behavior (TPB) (Ajzen, 1991) that is one of the most widely employed theories in behavior change studies. According to TPB (Ajzen, 1991), a person’s favorable or positive attitude towards a behavior and beliefs that significant others will approve the behavior (subjective norms) will drive the person’s intention to perform the behavior. The person’s perception of control over behavioral performance together with the behavioral intention will have a direct effect on the behavior. Employment, a factor outside the person’s control, may function as a barrier to behavior performance. Thus, the evidence supports that this theory can be applied in breastfeeding research.
To promote breastfeeding, several interventions using various approaches have been studied in both developed and developing countries. The existing promotion interventions have included prenatal education, professional support, and/or counseling; interventions during postnatal hospitalization; and postnatal follow-up home support (Hannula et al., 2008 and Imdad et al., 2011). With regard to timing of interventions, a systematic review of 53 studies from developed and developing countries revealed that all prenatal, postnatal, or combined interventions had significant effects on improving EBF rate at 4-6 weeks while combined prenatal and postnatal interventions had the highest effects on the rate at 6 months (Imdad et al., 2011). In terms of components of the interventions, it was found that education alone, professional support alone, or combined approaches could significantly promote EBF at 4-6 weeks, but only combined approaches could be effective at 6 months (Imdad et al., 2011). Findings of this review suggest that to achieve great impact on long-term EBF practice, components of the interventions should include combined approaches of prenatal and postnatal interventions. Interestingly, greater increase in EBF rate was found in developing countries compared to developed countries. However, relatively few studies have been reported from developing countries. Therefore, further studies in developing countries are still needed.
In China, studies examining effectiveness of the interventions for promoting long-term exclusive breastfeeding are scarce. One community-based home visit intervention was conducted for 200 postpartum women in Shanghai, China, with community nurses providing home visits twice during the two weeks after delivery (Yang, 2009). The EBF rate at 6 months reached 24% in the home visit group, which was significantly higher than the control group, of which the EBF rate was 5%. Nonetheless, these low rates of EBF in both groups did not meet the national target goal for breastfeeding. Therefore, the objective of this study was to assess the effectiveness of a theory-based comprehensive breastfeeding promotion intervention in improving long-term EBF practice in China. The TPB was chosen for guiding the intervention development, because its usefulness has been shown in breastfeeding research (Bai et al., 2011). The expected main outcome of the study was a high rate of EBF practice at 6 months, especially in the intervention group. A specific question of “Are the EBF rates at 3 days, 6 weeks, 4 months, and 6 months postpartum of the Chinese mothers in the intervention group higher than those of the control group?” was examined. perform the behavior. The person’s perception of control over behavioral performance together with the behavioral intention will have a direct effect on the behavior. Employment, a factor outside the person’s control, may function as a barrier to behavior performance. Thus, the evidence supports that this theory can be applied in breastfeeding research.
To promote breastfeeding, several interventions using various approaches have been studied in both developed and developing countries. The existing promotion interventions have included prenatal education, professional support, and/or counseling; interventions during postnatal hospitalization; and postnatal follow-up home support (Hannula et al., 2008 and Imdad et al., 2011). With regard to timing of interventions, a systematic review of 53 studies from developed and developing countries revealed that all prenatal, postnatal, or combined interventions had significant effects on improving EBF rate at 4-6 weeks while combined prenatal and postnatal interventions had the highest effects on the rate at 6 months (Imdad et al., 2011). In terms of components of the interventions, it was found that education alone, professional support alone, or combined approaches could significantly promote EBF at 4-6 weeks, but only combined approaches could be effective at 6 months (Imdad et al., 2011). Findings of this review suggest that to achieve great impact on long-term EBF practice, components of the interventions should include combined approaches of prenatal and postnatal interventions. Interestingly, greater increase in EBF rate was found in developing countries compared to developed countries. However, relatively few studies have been reported from developing countries. Therefore, further studies in developing countries are still needed.
In China, studies examining effectiveness of the interventions for promoting long-term exclusive breastfeeding are scarce. One community-based home visit intervention was conducted for 200 postpartum women in Shanghai, China, with community nurses providing home visits twice during the two weeks after delivery (Yang, 2009). The EBF rate at 6 months reached 24% in the home visit group, which was significantly higher than the control group, of which the EBF rate was 5%. Nonetheless, these low rates of EBF in both groups did not meet the national target goal for breastfeeding. Therefore, the objective of this study was to assess the effectiveness of a theory-based comprehensive breastfeeding promotion intervention in improving long-term EBF practice in China. The TPB was chosen for guiding the intervention development, because its usefulness has been shown in breastfeeding research (Bai et al., 2011). The expected main outcome of the study was a high rate of EBF practice at 6 months, especially in the intervention group. A specific question of “Are the EBF rates at 3 days, 6 weeks, 4 months, and 6 months postpartum of the Chinese mothers in the intervention group higher than those of the control group?” was examined.
MATERIALS AND METHODS
Research design
This was a longitudinal, randomized, controlled-trial study. The intervention group was offered the specially designed breastfeeding promotion intervention, plus routine nursing care. The control group received only routine nursing care that included one prenatal breastfeeding education class, rooming-in, breastfeeding initiation within half an hour after delivery, postnatal lactation consulting support by primary nurses, and pamphlets on breastfeeding presented in the ward during their hospitalization. The prenatal education class generally aims to promote pregnant women’s intention to breastfeed by providing information regarding its benefits. A positive attitude towards breastfeeding may be enhanced, but it is not emphasized. The above-mentioned postnatal nursing care is the routine approach for the Baby-Friendly Hospital designed to promote and support breastfeeding initiation. They are beneficial for most postpartum mothers; however, information provided and teaching/learning strategies are not specifically planned to improve the individual mothers’ attitude, subjective norm, and perceived control.
Participants
The study was conducted from October 2013 to June 2014 in the Shanghai First Maternity and Infant Hospital, Tongji University, which is a teaching hospital accredited as an “AAA”, tertiary care, specialty hospital with an average of 15,000-17,000 new births per annum. The participants were first-time Chinese mothers who met the following inclusion criteria: (1) physically and mentally capable of communicating, reading, and writing in Mandarin; (2) able to be interviewed by telephone at home until 6 months postpartum; (3) not having illnesses or problems that prohibit breastfeeding for both mother and baby; (4) having attended at least one prenatal education class; and (5) having either a husband, mother, or mother-in-law who met the following four inclusion criteria as a significant other: (a) able to communicate and read in Mandarin; (b) having regular contact with the participant; and (c) able to attend the intervention activities twice.
A permuted block random sampling method was used to assign the participants into the intervention or control group. Through randomizing participants within blocks, an equal number was assigned to the treatment group (T) and control group (C). Given a block size of four, there were six different possible arrangements (1=TCTC, 2=CTCT, 3=TTCC, 4=CCTT, 5=TCCT, 6=CTTC) in a block to assign participants equally to two groups. A random number sequence was used to choose a particular block, which set the allocation order for the first four subjects. The process was then repeated. The allocation proceeded by randomly selecting one of the orderings and assigning the participants to two groups according to the specified sequence. As each participant was admitted to a private room in the hospital, there was little cross contamination between the two groups.
The sample size was estimated in two ways. Firstly, the proportion of the participants with EBF for 6 months was estimated as 50%, the WHO target rate, in the intervention group (p1 = 0.5) and 30%, an average rate from previous studies, in the control group (p2 = 0.3). Then, the sample size was estimated as n= [(1.96+0.842)2 × (0.5 × 0.5+ 0.3 × 0.7)] / 0.202 = 90 subjects per group. When considering an attrition rate of nearly 20%, the sample size was estimated as 216. Secondly, because the study examined five breastfeeding factors, including breastfeeding knowledge, attitude, subjective norms, breastfeeding control, and working status or employment between two groups, repeated measures of ANOVA were used to estimate the sample size. According to the table of sample size estimation by ANOVA, with a power of 0.8 and a medium effect size, the sample size was estimated as 280*(1+20%) = 336 participants (considering the attrition rate of 20%). The researchers enrolled participants and assigned them to their groups. At the beginning of the study, 352 participants were recruited, including 180 in the intervention group and 172 in the control group. However, during the intervention period, 67 (19%) participants dropped out of the study at different stages of the intervention, as shown in Figure 1. Incomplete participation was only one criterion for termination. No other participant was terminated from the study. Finally, 285 participants, including 157 in the intervention group and 128 in the control group, completely participated in the study. The final number was almost equal to the expectant sample size that was adequate for analysis.
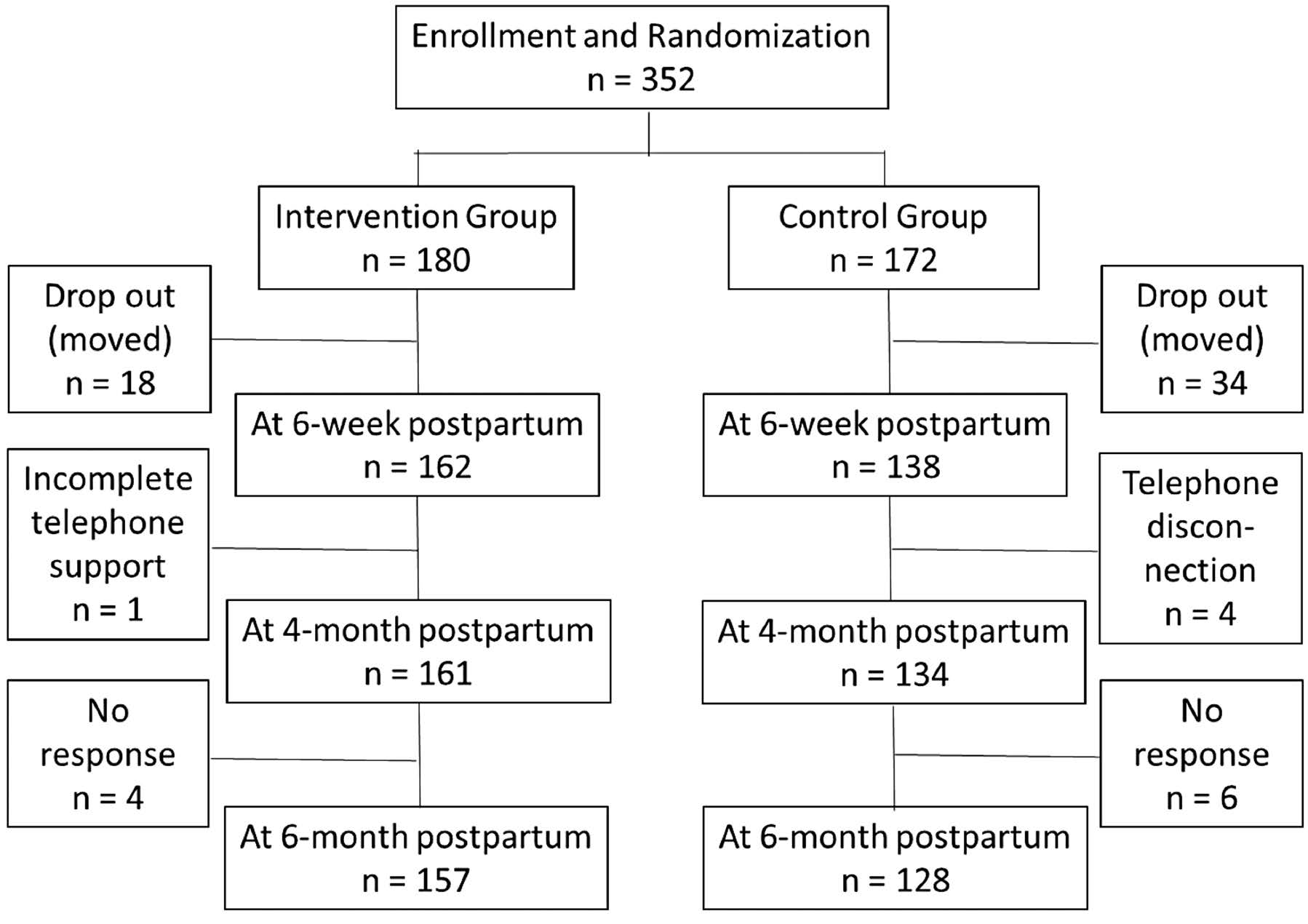
Figure 1. Flow Diagram of Participants through Each Stage of Interventions.
Theory-based comprehensive nursing intervention program
The comprehensive nursing intervention program was developed, by three members of the research team (the first three co-authors), mainly based on the TPB (Ajzen, 1991) and the findings of the previous study (Wan et al., 2015). The TPB assumes that behavioral intention is the most important determinant of behavior. Behavioral intention is influenced by three factors, including a person’s attitude toward a given behavior, subjective norms, and perceived behavioral control (Ajzen, 1991). The attitude refers to a person’s overall positive or negative feeling with respect to performing the behavior. It is determined by a person’s beliefs or expectations about the outcome of the behavior and evaluation of that outcome. The subjective norm is defined as a person’s subjective belief about the approval or disapproval of the behavior from people important to them. It is determined by two factors: beliefs about what significant others think the person should do and the person’s motivation to comply with those beliefs. The perceived behavioral control is a person’s belief in her own ability to perform the behavior. This is influenced by control beliefs and control power. Control beliefs are beliefs about resources available for performing the behavior, and control power is the perceived effect of resources on the difficulty of performance (Ajzen, 1991).
Therefore, the breastfeeding promotion interventions were designed to change women’s breastfeeding attitudes, subjective norms, and perceived breastfeeding
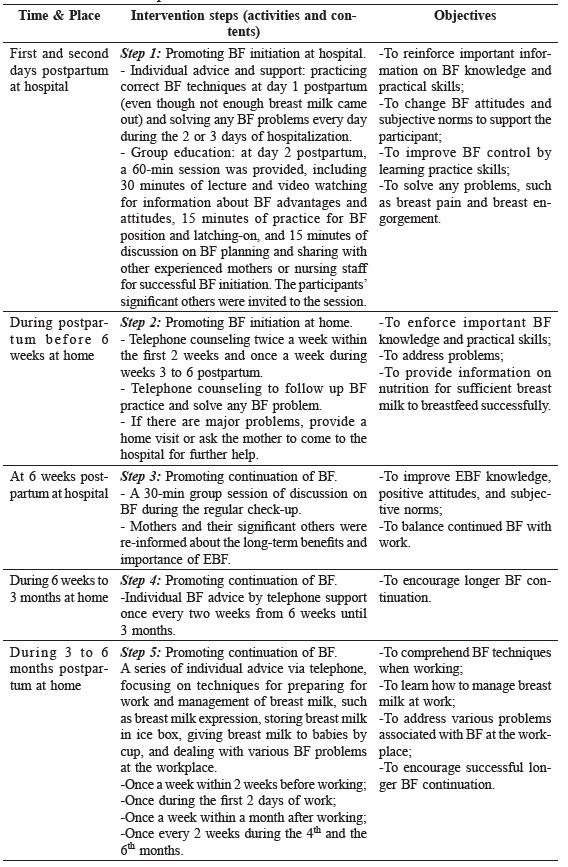
control by focusing on their underlying beliefs and values. Interventions to improve women’s breastfeeding knowledge and attitudes were planned by providing education with adequate essential information on EBF. The significant others of the women, including their husbands, mothers, or mother-in-laws, were invited to be involved in the activities to increase the women’s subjective norm. Finally, because the women’s working status was also a predictor of EBF at 6 months postpartum, the experiential learning activities attempting to enhance the women’s perceived breastfeeding control were designed to prepare employed women for EBF during their working hours. The protocol of this intervention targeted five different stages of breastfeeding, starting at the first and second days postpartum and completed at six months, as presented in Table 1. The first intervention did not begin during pregnancy, because all women of both groups had already attended prenatal education class.
Table 1. Intervention protocol.
Measurement
The research team developed the measures of demographic characteristics and breastfeeding practice. This included mother’s age, marital status, educational level, family yearly income, mother’s working status, and three questions on breastfeeding practice. The first question, “Do you currently breastfeed?” asked about the participant’s current infant feeding. If the response was “yes”, she was asked two additional questions to obtain detailed information regarding how she gave breast milk to her infant (e.g., with or without formula, water, and other foods). Then, the type of breastfeeding practice was identified. Practice of EBF was identified when an infant was fed only breast milk. No other liquids or solids, with the exception of drops or syrups consisting of vitamins, mineral supplements, or medicines, were given (WHO, 2002). If the answer was “no”, she was categorized in a group of no current EBF.
The modified Breastfeeding Attrition Prediction Tool (BAPT) and the Breastfeeding Knowledge Scale (BKS) were used to monitor changes in breastfeeding mediating factors. The original BAPT, consisting of three subscales (subjective norm, attitude, and control), was developed and revised by Janke (1994). It was modified and translated into Chinese by the first author and back translated into English by three bilingual professors, two in medicine and one in nursing. The modifications included deleting five items of the breastfeeding subjective norm subscale and changing the response scale from six to five levels. The deleted items identified family doctor, baby doctor, midwife, educator, and Lee League, which do not exist in the Chinese health care system as women’s significant others. A 5-point Likert scale was used because this scale is easy for participants to understand and make judgments. The subscales of breastfeeding attitude, the breastfeeding subjective norm, and the perceived control consisted of 29, 8, and 10 items, respectively. The Cronbach’s alpha coefficient of the total scale was 0.88, and the coefficients of the subscales were acceptable, ranging between 0.81 and 0.92. The BKS was developed and modified by Zhu et al. (2013). The modified BKS is a 5-point Likert scale with 25 items. Its content validity index (CVI) was 1.00 as reviewed by five experts in breastfeeding. The Cronbach’s alpha coefficient was 0.80.
Data collection
Before data collection, the Research Ethics Review Committee of the Faculty of Nursing, Chiang Mai University, Thailand and Shanghai First Maternity and Infant Hospital, Shanghai, China granted ethical approval. Each participant was approached on the first day after delivery and informed about the purpose of the study, procedures, confidentiality and anonymity preserved, and potential risks and benefits. Then, written informed consent was obtained. Demographic information was collected at the first day after birth and before starting the intervention. Data pertaining to breastfeeding knowledge, attitude, subjective norms, and perceived breastfeeding control were collected three times for monitoring: on the first day after birth as baseline data, 3 days postpartum before discharge from the hospital, and 6 weeks postpartum during a follow-up visit. All the questionnaires were self-completed by the participants. The data pertaining to breastfeeding practice were collected four times – at 3 days and 6 weeks postpartum using face-to-face interview at the hospital, and at 4 and 6 months postpartum using telephone interviews. The same three questions on breastfeeding practices were asked.
Data analysis
The licensed software SPSS 17.0 was employed to analyze all data. The level of significance was set at an alpha of 0.05. Data were tested and found normal distribution. The data were analyzed using descriptive statistics, t-test, Chi-square test, and repeated measure of ANOVA. T-test and Chi-square tests were used for comparison of participants’ characteristics between the intervention and control groups. Because the breastfeeding rates were compared by percentages between two groups, a Chi-square test was used. Two-way repeated measure ANOVA was used to analyze changes of breastfeeding mediating variables of the two groups at three different times (baseline, 3-days, and 6-week postpartum).
RESULTS
Characteristics of the participants
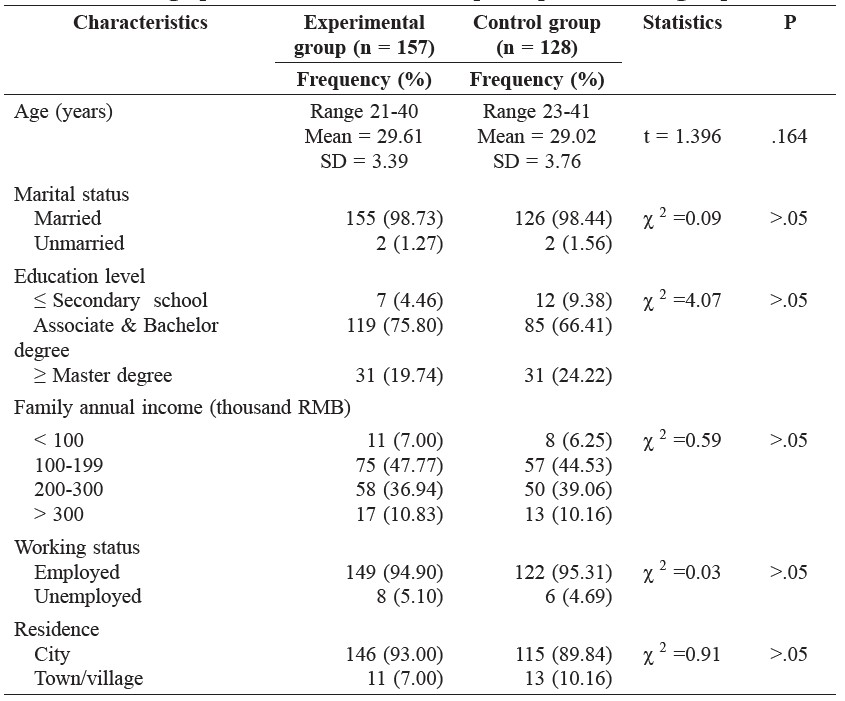
In this study, 285 first-time mothers participated, with 157 in the intervention group and 128 in the control group. The mother’s age ranged from 21 to 40 years, with average ages of 29.6 and 29.0 years in the intervention and control groups, respectively. The majority of the mothers were married, lived in the city, and held associate or bachelor’s degrees (75.8% of the intervention group and 66.4% of the control group). Nearly half (47.8% and 44.5% for the two groups) of the mothers had an annual family income of RMB 100-199 thousand (USD ~6,300-13,000), and more than one-third of the mothers in each group had an annual family income of RMB 200-300 thousand (USD ~13,000-20,000). The majority of the mothers were employed (94.9% of the intervention group and 95.3% of the control group). There were no significant differences in these demographic characteristics between the two groups, as shown in Table 2.
Table 2. Demographic characteristics of the participants in two groups.
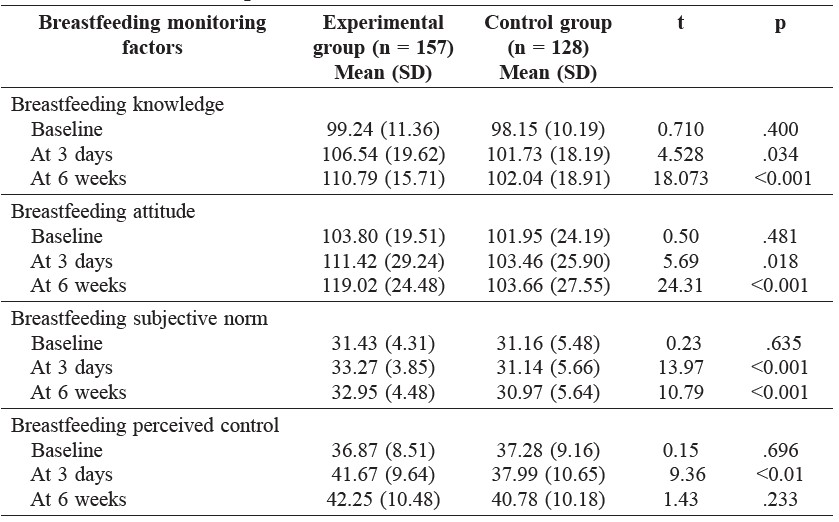
Comparison of breastfeeding mediating factors
Four breastfeeding mediating factors, including knowledge, attitude, subjective norm, and perceived control, were examined for the interaction effects of time and group. Baseline mean scores of the four factors of two groups were not different at the significance level of 0.05. The findings revealed that there were statistically significant differences in mean scores of breastfeeding knowledge, attitude, subjective norm, and perceived control between two groups at different time points (F=6.95, p <0.001; F=13.58, p <0.001; F=9.90, p <0.001; and F=7.17, p <0.01, respectively). Further analysis of the differences between mean scores of knowledge and attitude of two groups showed that the intervention group had significantly higher scores than the control group at 6 weeks (p <0.001). The subjective norm scores of the intervention group were significantly higher than those of the control group at both 3 days and 6 weeks (p <0.001) whereas the perceived control scores of the two groups were significantly different at 3 days only (p <0.01), as shown in Table 3.
Table 3. Comparison of Breastfeeding mediating factors between two groups at different time points.
Exclusive breastfeeding rates at different time points
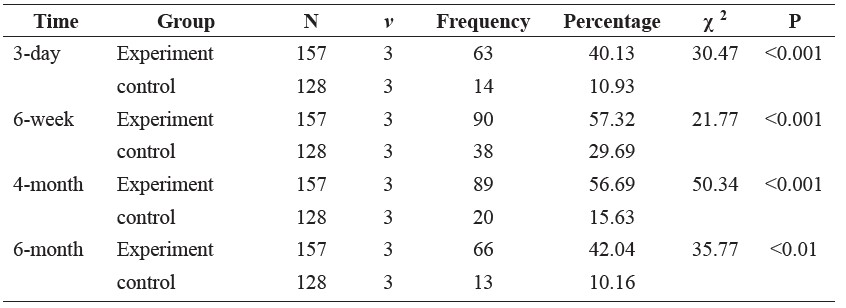
As illustrated in Figure 2, the EBF rates at 3 days, 6 weeks, 4 months, and 6 months postpartum in the intervention group (40.1%, 57.3%, 56.7%, and 42.0%, respectively) were consistently higher than those in the control group (10.9%, 29.7%, 15.6%, and 10.2%, respectively). The chi-square test showed that the EBF rates at all four time points in the intervention group were significantly higher than those in the control group (χ2= 30.47, p <0.001; 21.77, p <0.001; 50.34, p <0.001; and 35.77, p <0.01; respectively), as shown in Table 4.
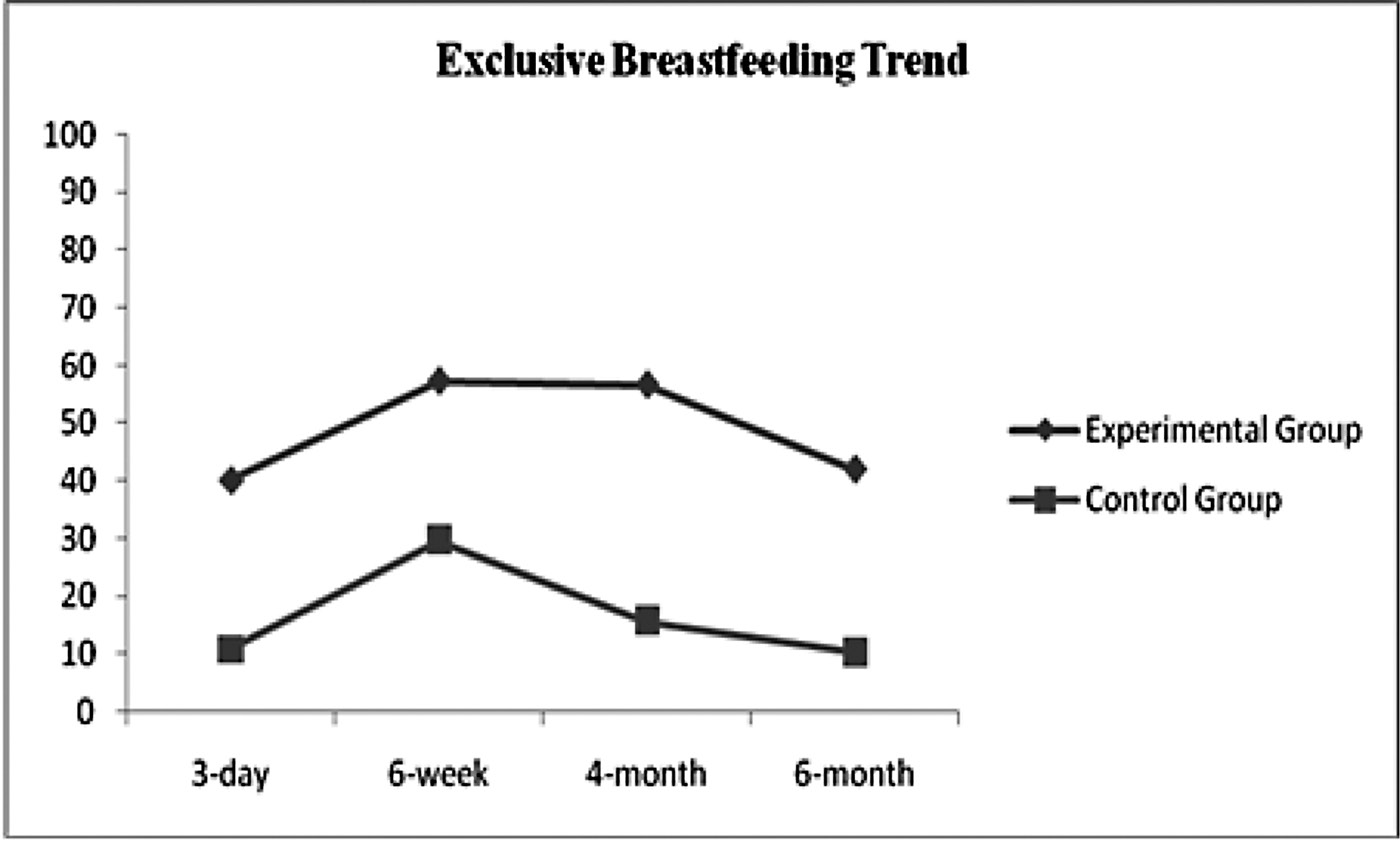
Figure 2. Exclusive breastfeeding rates of two groups at different time points.
Table 4. Comparison of exclusive breastfeeding rates at different time points.
DISCUSSION
The purpose of this longitudinal study was to evaluate the effectiveness of a specially designed, theory-based, breastfeeding promotion intervention on improving long-term EBF for first-time Chinese mothers. Overall, the findings suggest that the intervention was effective in increasing the EBF rates of the intervention group within 6 months postpartum. The EBF rates at 4 and 6 months among the intervention group were significantly higher than the control group in this study and were higher than the Chinese mothers in a recent study conducted by these researchers (Wan et al, 2015).
With regard to the breastfeeding initiation rate, it is interesting that although breastfeeding initiation was usually motivated in the study hospital, the EBF rates at 3 days postpartum of both the intervention (40.1%) and, in particular, the control groups (10.9%) were not high. The plausible explanations of these low EBF rates may be related to the mothers’ perception of insufficient breast milk, poor breastfeeding technique by either the new mothers or the infants, and no hospital policy to restrict formula or other foods. A study conducted in three cities of China revealed that the most difficult time for mothers to maintain EBF was 0-3 days (Zhu et al., 2014). Mothers’ worrying about insufficient nutrition for their babies and improper breastfeeding technique were the main problems. However, after that difficult time, the EBF rates in the current study increased in both groups. The increased rates of EBF at 6 weeks may be a result of the full adjustment to breast milk production and the improved breastfeeding skills of the mothers and the infants.
When EBF rates were compared between the two groups, the intervention group revealed significantly higher rates than the control group at all four time points. The findings demonstrated the effectiveness of the intervention program in promoting breastfeeding initiation and continuation. To promote breastfeeding initiation, in addition to the routine prenatal education class, the program included a series of interventions after delivery at the hospital and at home. Individual advice and support and group education were provided at days 1 and 2 after delivery, and the participants were provided counseling by telephone at least seven times during the first six weeks at home. These combined strategies led to an almost 93% increase in the EBF rate at 6 weeks (the rates were 57.3% in the intervention group compared to 29.7% in the control group). A review conducted by Imdad et al. (2011) revealed that the educational interventions significantly increased the EBF rate at 4-6 weeks by 43% (or 1.43 times). A previous study in Italy reported that postnatal telephone support during the first 6 weeks also led to an increased EBF rate in first time mothers (Simonetti et al., 2012).
To promote breastfeeding continuation, this study also employed various methods for the intervention. The invitation of the mothers’ significant others –including the husband or partner and own mother or mother-in-law – to participate in a postnatal group discussion that mainly focused on practical aspects to deal with breastfeeding problems was one among several approaches. Their involvement in the group discussion at 6 weeks postpartum was expected to improve the mother’s perception of social pressures for breastfeeding from referent persons or subjective norms (Ajzen, 1991). A previous non-experimental study based on TPB found that the mothers who continued breastfeeding at 6 weeks received more positive support from their partners and own mothers than the mothers who did not continue breastfeeding; likewise, subjective norms were important determinants of breastfeeding initiation and continuation (Swanson and Power, 2005). Another study evaluating the comprehensive peer support program in the United Kingdom found that significant others who were breastfeeding supporters could provide the mothers praise and reassurance and could help them overcome their obstacles to lead to an improved EBF rate (Thomson et al., 2012).
After 6 weeks until 6 months postpartum, telephone counseling and support were regularly provided. This intensified telephone support focused on preparing the mothers for breastfeeding when they returned to work. This intervention aimed to enhance the mothers’ perceived breastfeeding control or confidence in managing breast milk or their infant feeding and appeared to be effective because the EBF rate at 4 months remained high (56.7%). However, the EBF rate at 6 months slightly decreased to 42.0%. This decreased rate may be attributed to the declined effect of perceived breastfeeding control because of no or less workplace support. Since the perceived control is determined by control beliefs concerning the presence or absence of facilitators and barriers to behavioral performance and perceived power or effect of each factors to facilitate or inhibit the behavior (Ajzen, 1991), its effect can decline in situations in which prior facilitators are absent or new barriers to behavioral performance are present. Most of the mothers in this study were employed, and those who discontinued breastfeeding after 4 months cited returning to work as their main reason. This reason is similar to one of the major reasons given by most employed mothers who had completely stopped breastfeeding in previous studies (Tahir and Al-Sadat, 2013; Yimyam, 2013a; 2013b). It was also reported that mothers who were unable to nurse their infants during work shifts had 4.98 times higher odds of weaning before 4 months of age (Brasileiro et al., 2010; Yimyam, 2013a; 2013b). It was evident that employed women face various barriers in the workplace, such as not having a private room for breast milk expression and still requiring lactation information and support (Zinn, 2000). In Cohen and Mrtek’s (1994) study, 75% of the women who had access to a worksite breast pump room and lactation professional counseling continued to breastfeed their children to 6 months. In another study, 58% of the women with access to a similar physical facility and lactation professional services with an additional education class continued to breastfeed their children to 6 months (Ortiz et al., 2004). Therefore, the workplace policy and implementation of the breastfeeding promotion program for employed women must be considered.
Although the EBF rate at 6 months postpartum of the intervention group in this study did not achieve the Chinese national target rate, this rate was four times higher than the control group. In addition, the monitored scores of breastfeeding knowledge, attitude, subjective norm, and perceived control of the intervention group were higher than the control group. These findings indicate that the program was relatively effective for enhancing the breastfeeding contributing factors and consequently improving long-term EBF rate in China. They support the findings of recent systemic reviews (Haroon et al., 2013; Skouteris et al., 2014). Haroon and colleagues concluded that combined individual and group counseling appeared to be more effective than individual or group interventions alone. Another review by Skouteris et al. (2014) summarized other aspects of the effective interventions, and stated that the most successful interventions tended to include various forms of education and support and commenced in the postnatal period and continued for a relatively long period (from 3 weeks to 6 months) to provide ongoing assistance to mothers.
In conclusion, this intervention program was effective in improving EBF rates at 4 and 6 months postpartum among first-time Chinese mothers. The program involves a series of strategies during both hospitalization and the postnatal period at home. These include intensifying breastfeeding knowledge, improving positive breastfeeding attitudes, enforcing breastfeeding subjective norms, and strengthening perceived breastfeeding control. Therefore, the strategies included in this theory-based intervention program should be incorporated into the regular services of nurses in hospitals or in community healthcare for first time Chinese mothers to improve EBF. For example, breastfeeding education should be conducted by primary nurses as a part of routine care in the hospital, and follow-up telephone counseling should be performed to encourage new mothers to breastfeed exclusively and to help them address various problems associated with breastfeeding during their stay at home. Finally, a session of counseling and discussion is recommended as an intervention for preparing new mothers to return to work. Implementation of the breastfeeding promotion intervention in a healthcare setting and community, however, may not be sufficient, because problems remain in the workplace. Thus, policymakers are recommended to seriously consider issuing workplace policy for providing a private breastfeeding room and breastfeeding time at the workplace. This policy will significantly facilitate the breastfeeding practice among working mothers.
Since participants of this study were recruited from one setting in Shanghai, a large city in China, generalization of our findings to mothers in other areas should
be considered with caution. Therefore, it is recommended that further studies be conducted in other settings or other areas in China.
ACKNOWLEDGEMNTS
This study was supported by funding from the Shanghai Science and Technology Committee under Grants 134119a1000, 14495810900, and 13ZR1432800.
REFERENCES
Ajzen, I. 1991. The theory of planned behavior. Organizational Behavior and Human Decision Processes 50: 179-211.
Bai, Y., S.M. Wunderlich, and A.D. Fly. 2011. Predicting intentions to continue exclusive breastfeeding for 6 months: A comparison among racial/ethnic groups. Maternal Children Health Journal 15: 1257-1264.
Brasileiro, A.A., Rde. F. Possobon, K.C. Carrascoza, G.M. Ambrosano, and A.B. Moraes. 2010. The impact of breastfeeding promotion in women with formal employment. Cadernos de Saude Publica 26(9): 1705-1713.
Cohen, R., and M.B. Mrtek. 1994. The impact of two corporate lactation programs on the incidence and duration of breastfeeding by employed mothers. American Journal of Health Promotion 8(6): 436-441.
Hannula, L., M. Kaunonen, and M.T. Tarkka. 2008. A systematic review of professional support interventions for breastfeeding. Journal of Clinical Nursing 17: 1132-1143. DOI: 10.1111/j.1365-2702.2207.02239
Haroon, S., J.K. Das, R.A. Salam, A. Imdad, and Z.A. Bhutta. 2013. Breastfeeding promotion intervention and breastfeeding practices: A systematic review. BMC Public Health 13(suppl3): S20. DOI: 10.1 186/1471-2458-13-S3-S20.
Imdad, A., M.Y. Yakoob, and Z.A. Bhutta. 2011. Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC Public Health 11(suppl3): 1106. DOI: 10.1 186/1471-2458-11-S3-S24.
Janke, J. R. 1994. Development of the Breastfeeding Attrition Prediction Tool. Nursing Research 43(2): 100-104.
Jessri, M., A.P. Farmer, K. Maximova, N.D. Willows, and R.C. Bell. 2013. Predictors of exclusive breastfeeding: Observations from the Alberta pregnancy outcomes and nutrition (APrON) study. BMC Pediatrics 13(1): 77-92. DOI: 10.1186/1471-2431-13-77.
Lynn, A., and J. Rempel. 2004. Factors influencing the breastfeeding decisions of long-term breastfeeders. Journal of Human Lactation 20(3): 306-318.
McIsaac, K.E., W. Lou, D. Sellen, and T.K. Young. 2014. Exclusive breastfeeding among Canadian Inuit: Results from the Nunavut Inuit child health survey. Journal of Human Lactation 30(2): 229-141.
Meedya, S., K. Fahy, J. Yoxall, and J. Parratt. 2014. Increasing breastfeeding rates to six months among nulliparous women: A quasi-experimental study. Midwifery 30(3): 137-144.
Ortiz, J., K. McGilligan, and P. Kelly. 2004. Duration of breast milk expression among working mothers enrolled in an employer-sponsored lactation program. Pediatric Nursing 30(2): 111-119.
Oweis, A., A. Tayem, and E.S. Froelicher, 2009. Breastfeeding practices among Jordanian women. International Journal of Nursing Practice 15(1): 32–40.
Shen, L.P. 2008. Investigation and analysis of puerperal cognition of breastfeeding. Shanghai Nursing (Chinese) 8(3): 39-40.
Simonetti V, E. Palma, A. Giglio, A. Mohn, and G. Cicolini. 2012. A structured telephonic counseling to promote the exclusive breastfeeding of healthy babies aged zero to six months: A pilot study. International Journal of Nursing Practice 18(3): 289-294.
Skouteris, H., C. Nagle, M. Fowler, B. Kent, P. Sahota, and H. Morris. 2014. Intervention designed to promote exclusive breastfeeding in high-income countries: A systematic review. Breastfeeding Medicine 9(3): 113-127. Doi: 10.1089/bfm. 2013.0081.
Swanson, V., and K.G. Power. 2005. Initiation and continuation of breastfeeding: Theory of planned behaviour. Journal of Advanced Nursing 50: 272-282.
Tahir, N.M., and N. Al-Sadat. 2013. Does telephone lactation counseling improve breastfeeding practices? A randomized controlled trial. International Journal of Nursing Studies 50(1): 16-25.
Tang, L., C.W. Binns, C. Luo, Z. Zhong, and A.H. Lee. 2013. Determinants of breastfeeding at discharge in rural China. Asia Pacific Journal of Clinical Nutrition 22(3): 443-438.
Thomson, G., N. Crossland, and F. Dykes. 2012. Giving me hope: Women’s reflections on a breastfeeding peer support service. Maternal Children Nutrition 8(3): 340-353.
Wan, H.W., S. Tiansawad, S. Yimyam, and P. Sriarporn. 2015. Factors predicting exclusive breastfeeding among the first time Chinese mothers. Pacific Rim International Journal of Nursing Research 19(1): 32-44.
Wen, L.M., L.A. Baur, J.M. Simpson, C. Rissel, and V.M. Flood. 2011. Effectiveness of an early intervention on infant feeding practices and “Tummy Time”. Arch Pediatrics Adolescence Med 165(8): 701-707.
World Health Organization. 2002. The World Health Organization’s Infant Feeding Recommendation. Retrieved October 30, 2010, from http://www.who.int/nut.
Yang, M.H. 2009. The effect of home visit program on exclusive breastfeeding. Medicine and Nurse Journal (Chinese) 9(3): 15-16.
Yimyam, S. 2011. Breastfeeding beliefs and practices among employed women: a Thai cultural perspective. In P. Liampongtong (Ed). Infant feeding beliefs and practices: A cross-cultural perspective. Springer: New York.
Yimyam, S. 2013a. Promoting breastfeeding practices among Thai employed mothers. pp. 159-180. In T. M. Cassidy (Ed). Breastfeeding: Global practices, challenges, maternal and infant health outcomes. New York: NOVA Publishing.
Yimyam, S. 2013b. Breastfeeding experiences among employed mothers. In T. M. Cassidy (Ed). Breastfeeding: Global practices, challenges, maternal and infant health outcomes (pp. 181-200). New York: NOVA Publishing.
Zhao, J.Y. 2010. Who is responsible for the low exclusive breastfeeding rate within 6 months - Aggressive formula advertisement? South of China Daily (Chinese), Retrieved Aug. 15, 2010. from http://medicine.people.com.cn/GB/12400323.html.
Zhu, X., J. Tian, G. Chen, and K. Christensson. 2014. Predictors of breastfeeding exclusively in three cities of China. Breastfeeding Medicine 9: 103-104. doi:10.1089/bfm.2013.0053
Zhu, Y., H.W. Wan, and R. Huang. 2013. The development of breastfeeding at 6 months postpartum. Shanghai Jiaotong University Medical Science (Chinese)
18: 1176-1181.
Zinn, B. 2000. Supporting the employed breastfeeding mother. Journal of Midwifery & Women’s Health 45(3): 216-226.
Hongwei Wan1, Sujitra Tiansawad2*, Susanha Yimyam2 and Punpilai Sriarporn2
1 Shanghai Proton and Heavy Ion Hospital, Fudan University, Pudong, Shanghai 201321, the People’s Republic of China
2 Faculty of Nursing, Chiang Mai University, Chiang Mai 50200, Thailand
*Corresponding author. E-mail: stiansawad@gmail.com
Total Article Views

