
Accuracy of Cone Beam Computed Tomography for Dental Implant Treatment Planning
Pathawee Khongkhunthian*, Kanoknual Jomjunyong and Peter A. ReichartPublished Date : 2017-01-01
DOI : 10.12982/cmujns.2017.0005
Journal Issues : Number 1 ,January - March 2017
ABSTRACT
This study evaluated the accuracy of cone beam computed tomography (CBCT) measurements using post-surgical, implant placement, CBCT images by measuring the length and width of implants on CBCT images and comparing these measurements to the actual sizes of the implants, as well as investigated critical anatomical structure injuries after using CBCT for planning. Ninety-six post-operative CBCT scans of 171 dental implants, placed between October 2012 and March 2015, were included in the study. Each implant was measured on the CBCT images for both diameter and length, using the measuring tool in the CBCT software. The measured values were compared with the actual implant diameters and lengths and calculated as a percentage of error. The mean percentage of error was 2.26%. There were no significant differences in percentage of error between implant size, implant diameters, implant positions, upper jaw, lower jaw, anterior area, or posterior area (p>0.05). Anatomical structure injuries were not found post-operatively. The accuracy of CBCT used for measurement in this study was 97.74%, and comparable to that reported for other commercial CBCT machines. The use of CBCT for implant planning can avoid anatomical structure injuries.
Keywords: 3D imaging, Implant measurement, CBCT accuracy
INTRODUCTION
Dentistry is increasingly using cone beam computed tomography (CBCT), including in implant dentistry (Tyndall et al., 2012; Gupta and Ali, 2013; Bornstein et al., 2014), endodontics (Lofthag-Hansen et al., 2007; Patel, 2009; Janner et al., 2011), oral and maxillofacial surgery (Alamri et al., 2012), periodontics (Walter et al., 2009; De Faria Vasconcelos et al., 2012), orthodontics (Van Vlijmen et al., 2012; Machado, 2015), and temporomandibular joint disorders (Alamri et al., 2012).
One benefit of using CBCT is the ability to thoroughly inspect the hard tissues of interest in three dimensions. CBCT overcomes the limitations of 2-D radiographic images in fields of view and the overlapping of complex anatomy. Moreover, CBCT provides more advantages than conventional cross-sectional tomography (CT), because of its low-dose radiation, image accuracy, rapid scan time, narrow x-ray beam field, and reduction of image artifacts (Scarfe et al., 2006).
In dental implant treatment, CBCT has been used mainly for implant surgical planning, post operatively, and for follow-up evaluation. Pre-operative CBCT helps in establishing the morphologic characteristics of the residual alveolar ridge, determining the orientation of the residual alveolar ridge and identifying local anatomic or pathologic boundaries within the residual alveolar ridge. Post-operative CBCT helps evaluate complications form implant surgery (Madhav, 2011; Kumar and Satheesh, 2013; Bornstein et al., 2014).
The accuracy of dental implant treatment is of great concern to avoid injury to critical anatomical tissues, such as the inferior alveolar nerve and vessels, mental nerve and maxillary sinus (Madhav, 2011). Normally, implant treatment planning should have a 2-mm safety zone between vital structures and implant measuring in radiographic film (Misch and Crawford, 1990; Greenstein and Tarnow, 2006; Misch and Wang, 2008). If vital structures are injured, clinical symptoms may include pain, hematoma, or numbness. CBCT accuracy is affected by the hardware, on which values such as exposure time, tube voltage, and field of view are set, and the software used to analyze the generated images. The thickness of the soft tissues in the areas of interest, the voxel size of the scan, and the intensity of radiation dose can also affect CBCT accuracy (Fourie et al., 2010; Wood et al., 2013).
Several studies have measured CBCT accuracy, both in vitro (Suomalainen et al., 2008; Razavi et al., 2010; Gerlach et al., 2013) and in vivo (Li et al., 2008; Correa et al., 2014). A comparative study in dry skulls comparing CBCT, panoramic, linear tomographic, and periapical imaging found that CBCT had the least error (Gher and Richardson, 1995). Pertl et al. (2013) showed that CBCT provided the most accurate preoperative assessment of the mandibular canal compared to panoramic imaging and medical CT. Mohamad Amin et al. (2013) measured the length of implants using CBCT post-operatively; they reported a range of measurement error of 1.86-4.61% and no significant difference between implant fixture length in CBCT and the actual implant fixture length.
The most serious complications in implant dentistry are injury of critical anatomical structures, such as the inferior alveolar nerve, from surgical implant placement, the incidence of which has been reported to be as high as 13% (Ellies, 1992; Bartling et al., 1999; Libersa et al., 2007; Tay and Zuniga, 2007; Renton and Yilmaz, 2011). The incidence of penetration of the maxillary sinus is about 7-58% (Buchmann et al., 1999; Schwartz-Arad et al., 2004; Shlomi et al., 2004). CBCT is one of the most accurate and precise techniques for localization of vital anatomical structures. Because CBCT has become the standard of care for patients receiving implant treatment (Tyndall et al., 2012), better understanding its accuracy is important.
The purposes of this study were to evaluate: 1) the accuracy of measurement of implant length and diameter on post-operative CBCT images from a CBCT machine (Dentiiscan, National Science and Technology Development Agency, Bangkok, Thailand) by using CBCT software (Dentiplan, National Science and Technology Development Agency, Bangkok, Thailand) and 2) the incidence of critical anatomical structure injury from implant surgical placement after using CBCT for planning.
MATERIALS AND METHODS
Study sample
Ninety-six post-operative CBCT scans (51 women and 45 men, mean age 52.5 years, ranging from 20 to 75 years) recorded between October 2012 and March 2015 at the Center of Excellence for Implantology, Chiang Mai University, Thailand using a Dentiiscan machine (NSTDA, Bangkok, Thailand) were used in this study. All ninety-six patients had pre- and post-operative CBCT scans for treatment planning and evaluating post-operative injury to vital structure. The CBCT device used a tube voltage setting of 90 kV, pulses of 6 mA, a scan time of 18 seconds, a maximum FOV of 160 x130 mm, and a voxel size of 0.4 mm. Data from the CBCT were exported in DICOM format.
A total of 171 implants were evaluated (one patient could have more than one implant). CBCT scans showed PW+ implants (PW+, Bangkok, Thailand) of various sizes – 3.30 mm (N=5), 3.75 mm (N=52), 4.2 mm (N=59), and 5.0 mm (N=55) – and various lengths – 8.0 mm (N=8), 10.0 mm (N=86), 12.0 mm (N=72), and 14.0 mm (N=5) (Table 1), each covered with a cover screw or healing cap.
CBCT measurement
CBCT data were analyzed using Dentiplan Version 2.9 (NSTDA, Bangkok, Thailand), software for Dentiiscan, and displayed on an LCD 21" screen (ACER NVIDIA G FORCE, GTX 570) at a resolution of 1600 x 900 pixels and a greyscale of 11 bits (2048 shades of grey) in a dark room.
All measurements were made once by a trained observer with 3-years experience in implant dentistry who was not allowed to know the real sizes of the implants in advance. A pilot study was conducted to define the intra-observer reliability of the observer. The observer repeated the measurements three times, in iterations two and four weeks after the first measurement, and an intra-class correlation coefficient was calculated from the mean of the three measurements. All data were measured in the cross-sectional CBCT images using the linear measurement tool. The magnification settings were adjusted to fit the size of the screen for optimal display. A horizontal straight line was drawn using the measurement tool in Dentiscan, from the most superior point on one edge of the implant to the corresponding point on the opposite edge of the same implant. The vertical distance was similarly measured between the mid-point of the horizontal tangent to the most radiopaque tip of the implant (Figure 1).
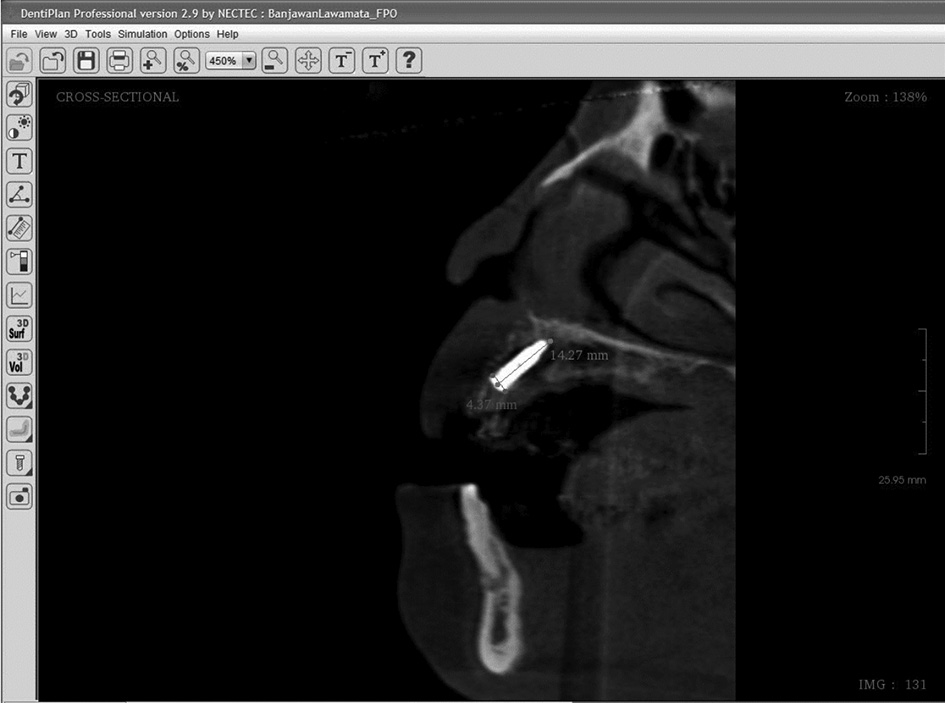
Figure 1. Implant measurement in cross-sectional CBCT using Dentiplan Version 2.9 (NSTDA, Bangkok, Thailand).
Descriptive statistics were calculated using Excel 2010 (Microsoft, Redmond, WA, USA). Statistical analysis was performed using SPSS® v. 17 (SPSS, Chicago, IL). The data were normally distributed, and the Student t-test was used to compare the measurements of the implants in CBCT and their real sizes; bivariate correlation was used to find the correlation between implant measurement errors and their real sizes, both data presented as mean and standard deviation. Differences were considered significant at p < 0.05. The average of three measurements from CBCT compared to the real size of the implants using the intra-class correlation coefficient (ICC) was used to investigate intra-examiner reproducibility.
RESULTS
The intraclass correlation coefficients (ICC) for the measurements were 0.946 for diameter and 0.984 for length, demonstrating good reproducibility within the observer.
The mean value and the standard deviation of the differences between radiological measurements and the real 171 implant sizes were 0.24 mm (SD ± 0.14) for diameter and 0.25 mm (SD ± 0.16) for length (Table 2). The ranges of percentage of measurement deviation were 0–6% for diameter and 0–6% for length. The means and standard deviation error percentages were 2.21% (SD ± 1.33) for diameter and 2.31 (SD ± 1.55) for length. The error percentages were then cal-culated back to the accuracy of the measurement; the accuracy of measurements for diameter and length were 97.79% and 97.69%, respectively. The radiological measurements were mostly overestimated compared to the real implant sizes.
The errors of measurement were not significantly different between the maxilla and mandible (p = 0.992 for diameter and 0.258 for length) (Table 3), nor between the anterior and posterior region (p = 0.561 for diameter and p = 0.803 for length) (Table 4). A correlation was not found between implant diameter and percentage of diameter measurement error (p=0.293), nor between implant length and percentage of length measurement error (p=0.12). (Figures 2 and 3)
Moreover, this study showed no vital anatomical structures, such as inferior alveolar nerve or maxillary sinus injuries, in 96 post-operative CBCT images.
Table 1. Distribution of implant site according to positions.
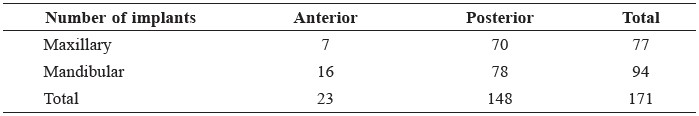
Table 2. Mean, Standard deviation (SD) of the measurement error for diameter and length of implants in CBCT cross images.
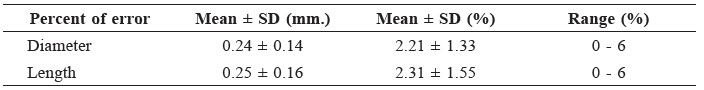
Table 3. Overview of the relative difference between positions (Maxillary/Mandibular) and percent measurement error of diameter and length. The mean and standard deviation (SD) are depicted including the 95% confidence interval (95% CI).
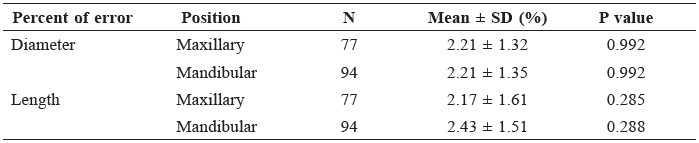
Table 4. Overview of the relative difference between positions (Anterior/Posterior) and percent measurement error of diameter and length. The mean and standard deviation (SD) are depicted including the 95% confidence interval (95% CI).
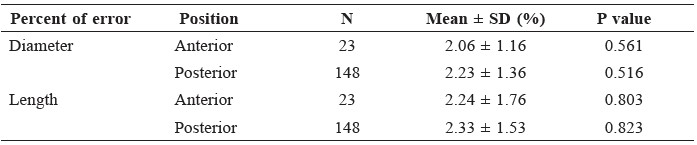
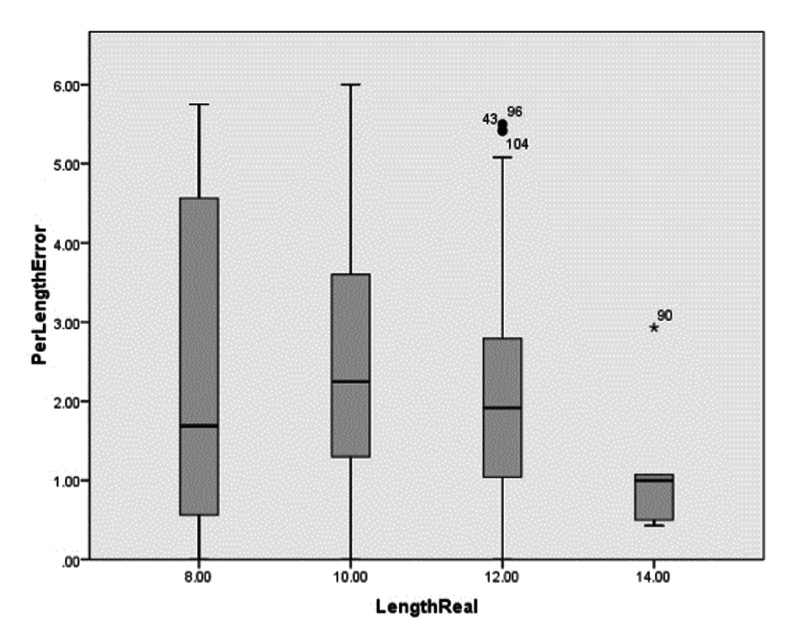
Figure 2. Box plot showing no correlation between percent diameter measurement errors and the real diameters.
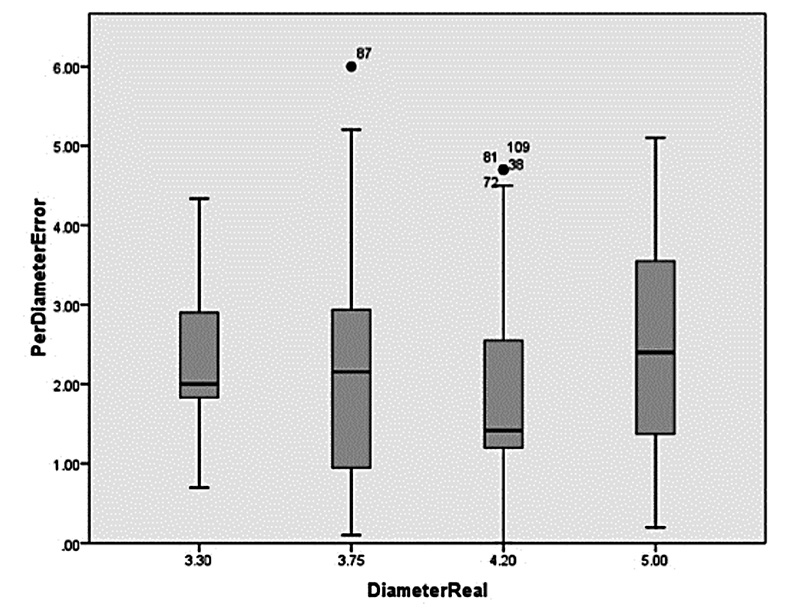
Figure 3. Box plot showing no correlation between percent length measurement errors and the real lengths.
DISCUSSION
CBCT in dental implant treatment is a necessary tool for implant positioning and placement planning (Bornstein et al., 2014). A systematic review of guidelines for using CBCT has indicated that the need for specific imaging should be based on clinical presentation and professional judgment to gain information for implant treatment planning (Tyndall et al., 2012; Bornstein et al., 2014). Some reports describe using CBCT for pre- and/or post-operative assessment for dental implant treatment (Bornstein et al., 2014). In our dental implant clinic, we use CBCT for both pre- and post-operative dental implant treatment. Post-operative CBCT following implant surgery can help ensure that the implant is placed correctly relative to critical anatomical structures, such as the inferior alveolar nerve. The use of CBCT post-operatively is of concern, because of the need to minimize patient exposure to radiation (Harris et al., 2012). The guidelines on using CBCT in implant dentistry are still being developed. The American Academy of Oral and Maxillofacial Radiology guidelines for using CBCT in dentistry state that conventional cross-sectional tomography is the method of choice for gaining the most information for most patients receiving implants (Tyndall et al., 2012). However, a systematic review of CBCT in implant dentistry stated that there is a clear need for guidelines that provide strong statements based on a rigorous methodological review of the evidence (Bornstein et al., 2014).
The accuracy of CBCT together with the software used for analysis is crucial for surgical planning in dental implantology. Many studies related to the accuracy of linear measurements have been published (Kobayashi et al., 2004; Lascala et al., 2004; Misch et al., 2006; Ludlow et al., 2007; Lund et al., 2009; Razavi et al., 2010; Harris et al., 2012). A study in cadaver mandibles by Suomalainen et al. (2008) to measure the accuracy of a CBCT showed an average measurement error of 2.3-4.7%. They also found that the measurement accuracy in mandibles with soft tissue immersed in sucrose solution was greater than that in dry mandibles. Another study, also in cadaver mandibles, which compared measurement of mandible height and width using CBCT with histological data, reported a maximum difference of 0.33 mm (SD ± 0.34). Cortical thickness measurements, especially, were significantly greater on CBCT images (p < 0.006) (Gerlach et al., 2013). Another study using CBCT measured the distance between the alveolar crest and mandibular canal, and reported a range of error of -1.5-0.8 mm (Pertl et al., 2013). All of those studies used different CBCT machines from different manufacturers. Mohamad Amin et al. (2013) compared measurement of real implant length and implant length from CBCT and found no significant difference, with similar average error for measurements as our study. Their study was smaller (11 patients / 47 implants), did not measure diameter, and used different software.
From our study, the results showed the average error for measurement of implants was 2.21% for implant diameter and 2.31% for implant length Moreover, there was no significant difference for both diameter and length measurement error compared to the real sizes (p = 0.293 for diameter and p = 0.12 for length). A correlation was not found between implant length and diameter and percentage of length and diameter measurement errors.
Several factors affect the accuracy of measurement with CBCT, such as the thickness of soft tissue, thickness of cortical bone, and voxel (thickness of bone slide). (Damstra et al., 2010; Spin-Neto et al., 2013; Wood et al., 2013). Patient movement during CBCT exposure leads to image distortion, which may affect measurement accuracy. Bone thickness may also affect measurement accuracy. Razavi et al. (2010) compared implant size measurement at varying distances from the cortical bone and found that some CBCT machines may not produce sufficient resolution of the thin cortical bone adjacent to dental implants. Moreover, metal artifacts can reduce the visibility of bone and soft tissue and result in inaccurate assessment of peri-implant regions. In our in vivo study, there were no significant differences between the average measurement errors of implant positions or implant sizes.
Injuries to critical anatomical structures during the implant surgery, such as inferior alveolar nerve injury and perforations of the maxillary sinus, are considered severe intra-operative complications. Using CBCT can avoid such serious complications. 3D planning in implant dentistry is increasingly accepted as a requirement to prevent such complications (BouSerhal et al., 2002; Bornstein et al., 2014). The measurement error of our Dentiiscan machine is less than 0.5 mm, within the recommended 2-mm safety zone between implant and crucial anatomical structures (Misch and Crawford, 1990; Greenstein and Tarnow, 2006; Misch and Wang, 2008). Our study results showed no injury to critical anatomical structures.
Our ICC was close to 1, indicating good reliability of the observer (Eldridge, 2009). However, metal artifacts may affect the accuracy of measurement in this study and might be the cause of over-measurement of the implants seen in CBCT.
CONCLUSIONS
This study showed no significant differences of measurement errors between measured values and the actual sizes in the various positions and sizes of implants. The accuracy of images produced by the Dentiiscan CBCT machine was 97.79% for diameter and 97.69% for length. There were no anatomical injury complications during implant placement in all cases with pre-operative CBCT at the Centre of Excellence for Implantology, Chiang Mai University, Thailand. We have proven that Dentiiscan is a reliable diagnostic tool in implant treatment planning.
ACKNOWLEDGEMENTS
The investigators gratefully acknowledge the Center of Excellence for Dental Implantology, Chiang Mai University and Saowapak Thongvigitmanee, National Electronics and Computer Technology Center, Bangkok, Thailand. We also thank Narumanus Korwanich and Thanapat Sastraruji, Faculty of Dentistry, Chiang Mai University for statistical consultation.
REFERENCES
Alamri, H. M., M. Sadrameli, M. A. Alshalhoob, M. Sadrameli, and M. A. Alshehri. 2012. Applications of Cbct in dental practice: A review of the literature. general dentistry. 60: 390-400; quiz 401-392.
Bartling, R., K. Freeman, and R. A. Kraut. 1999. The incidence of altered sensation of the mental nerve after nandibular implant placement. Journal of Oral and Maxillofacial Surgery. 57: 1408-1412.
Bornstein, M. M., W. C. Scarfe, V. M. Vaughn, and R. Jacobs. 2014. Cone beam computed tomography in implant dentistry: A systematic review focusing on guidelines, indications, and radiation dose risks. The international Journal of Oral and Maxillofacial Implants. 29 Suppl: 55-77.
BouSerhal, C., R. Jacobs, M. Quirynen, and D. van Steenberghe. 2002. Imaging technique selection for the preoperative planning of oral implants: A review of the literature. Clinical Implant Dentistry Related Research. 4: 156-172.
Buchmann, R., F. Khoury, C. Faust, and D. E. Lange. 1999. Peri-Implant conditions in periodontally compromised patients following maxillary sinus augmentation. A Long-Term Post-Therapy Trial. Clinical Oral Implants Research. 10: 103-110.
Correa, L. R., R. Spin-Neto, A. Stavropoulos, L. Schropp, H. E. da Silveira, and A. Wenzel. 2014. Planning of dental implant size with digital panoramic radiographs, Cbct-generated panoramic images, and Cbct cross-sectional Images. Clinical Oral Implants Research. 25: 690-695.
Damstra, J., Z. Fourie, J. J. Huddleston Slater, and Y. Ren. 2010. Accuracy of linear measurements from cone-beam computed tomography-ferived surface models of different voxel sizes. American Journal of Orthodontics and Dentofacial Orthopedics. 137: 16 e11-16; discussion 16-17.
De Faria Vasconcelos, K., K. M. Evangelista, C. D. Rodrigues, C. Estrela, T. O. de Sousa, and M. A. Silva. 2012. Detection of periodontal bone loss using cone beam Ct and intraoral radiography. Dentomaxillofacial Radiology. 41: 64-69.
Eldridge, S. M., O. C. Ukoumunne, and J. B. Carlin. 2009. The Intra-Cluster correlation coefficient in cluster randomized trials: A review of definitions. International Statistical Review. 77: 378-394.
Ellies, L. G. 1992. Altered sensation following mandibular implant surgery: A retrospective study. The Journal of Prosthetic Dentistry. 68: 664-671.
Fourie, Z., J. Damstra, P. O. Gerrits, and Y. Ren. 2010. Accuracy and reliability of facial soft tissue depth measurements using cone beam computer tomography. Forensic Science International. 199: 9-14.
Gerlach, N. L., G. J. Meijer, W. A. Borstlap, E. M. Bronkhorst, S. J. Berge, and T. J. Maal. 2013. Accuracy of bone surface size and cortical layer thickness measurements using cone beam computerized tomography. Clinical Oral Implants Research. 24: 793-797.
Gher, M. E., and A. C. Richardson. 1995. The accuracy of dental radiographic techniques used for evaluation of implant fixture placement. The International Journal of Periodontics & Restorative Dentistry. 15: 268-283.
Greenstein, G., and D. Tarnow. 2006. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: A literature review. Journal of Periodontology. 77: 1933-1943.
Gupta, J., and S. P. Ali. 2013. Cone beam computed tomography in oral implants. National Journal Maxillofacial Surgery. 4: 2-6.
Harris, D., K. Horner, K. Grondahl, R. Jacobs, E. Helmrot, G. I. Benic, M. M. Bornstein, A. Dawood, and M. Quirynen. 2012. E.A.O. Guidelines for the use of diagnostic imaging in implant dentistry 2011. Clinical Oral Implants Research. 23: 1243-1253.
Janner, S. F., F. B. Jeger, A. Lussi, and M. M. Bornstein. 2011. Precision of endodontic working length measurements: A Pilot investigation comparing cone-beam computed tomography scanning with standard measurement Techniques. Journal of Endodontics. 37: 1046-1051.
Kobayashi, K., S. Shimoda, Y. Nakagawa, and A. Yamamoto. 2004. Accuracy in measurement of distance using limited cone-beam computerized tomography. The International Journal of Oral & Maxillofacial Implants. 19: 228-231.
Kumar, V., and K. Satheesh. 2013. Applications of cone beam computed tomography (Cbct) in implant treatment planning. JSM Dentistry. 1: 1008.
Lascala, C. A., J. Panella, and M. M. Marques. 2004. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (Cbct-Newtom). Dentomaxillofacial Radiology. 33: 291-294.
Li, H., X. R. Zhu, L. Zhang, L. Dong, S. Tung, A. Ahamad, K. S. Chao, W. H. Morrison, D. I. Rosenthal, D. L. Schwartz, R. Mohan, and A. S. Garden. 2008. Comparison of 2d radiographic images and 3d cone beam computed tomography for positioning head-and-neck radiotherapy patients. International Journal of Radiation Oncology, Biology, Physics. 71: 916-925.
Libersa, P., M. Savignat, and A. Tonnel. 2007. Neurosensory disturbances of the inferior alveolar nerve: A retrospective study of complaints in a 10-Year period. Journal of Oral and Maxillofacial Surgery. 65: 1486-1489.
Lofthag-Hansen, S., S. Huumonen, K. Grondahl, and H. G. Grondahl. 2007. Limited cone-beam Ct and intraoral radiography for the diagnosis of periapical pathology. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 103: 114-119.
Ludlow, J. B., W. S. Laster, M. See, L. J. Bailey, and H. G. Hershey. 2007. Accuracy of measurements of mandibular anatomy in cone beam computed tomography images. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 103: 534-542.
Lund, H., K. Grondahl, and H. G. Grondahl. 2009. Accuracy and precision of linear measurements in cone beam computed tomography accuitomo tomograms obtained with different reconstruction techniques. Dentomaxillofacial Radiology. 38: 379-386.
Machado, G. L. 2015. Cbct Imaging - a boon to orthodontics. The Saudi Dental Journal. 27: 12-21.
Madhav, V. N. V. 2011. Cone beam computed tomography in implantology. Indian Journal of Dental Sciences. 3: 10-15.
Misch, C. E., and E. A. Crawford. 1990. Predictable mandibular nerve location-- A clinical zone of safety. The International Journal of Oral Implantology. 7: 37-40.
Misch, K., and H. L. Wang. 2008. Implant surgery complications: etiology and treatment. Implant Dentistry. 17: 159-168.
Misch, K. A., E. S.Yi, and D. P.Sarment. 2006. Accuracy of cone beam computed tomography for periodontal defect measurements. Journal of Periodontology. 77: 1261-1266.
Mohamad Amin, L. I., S. A., Rahman, M. K. Alam, and F. Daud. 2013. Validity of cone beam computed tomography (Cbct) on estimation of implant fixture length. International Medical Journal. 20: 355-358.
Patel, S. 2009. New dimensions in endodontic imaging: Part 2. cone beam computed Tomography. International Endodontic Journal. 42: 463-475.
Pertl, L., B. Gashi-Cenkoglu, J. Reichmann, N. Jakse, and C. Pertl. 2013. Preoperative assessment of the mandibular canal in implant surgery: Comparison of rotational panoramic radiography (Opg), Computed tomography (Ct) and cone beam computed tomography (Cbct) for preoperative assessment in implant surgery. European Journal of Oral Implantology. 6: 73-80.
Razavi, T., R. M. Palmer, J. Davies, R. Wilson, and P. J. Palmer. 2010. Accuracy of measuring the cortical bone thickness adjacent to dental implants using cone beam computed tomography. Clinical Oral Implants Research. 21: 718-725.
Renton, T., and Z. Yilmaz. 2011. Profiling of patients presenting with posttraumatic neuropathy of the trigeminal nerve. Journal of Orofacial Pain. 25: 333-344.
Scarfe, W. C., A. G. Farman, and P. Sukovic. 2006. Clinical applications of conebeam computed tomography in dental practice. Journal Canadian Dental Association. 72: 75-80.
Schwartz-Arad, D., R. Herzberg, and E. Dolev. 2004. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. Journal of Periodontology. 75: 511-516.
Shlomi, B., I. Horowitz, A. Kahn, A. Dobriyan, and G. Chaushu. 2004. The effect of sinus membrane perforation and repair with lambone on the outcome of maxillary sinus floor augmentation: A radiographic assessment. The International Journal of Oral & Maxillofacial Implants. 19: 559-562.
Spin-Neto, R., E. Gotfredsen, and A. Wenzel. 2013. Impact of voxel size variation on Cbct-based diagnostic outcome in dentistry: A systematic review. Journal of Digital Imaging. 26: 813-820.
Suomalainen, A., T. Vehmas, M. Kortesniemi, S. Robinson, and J. Peltola. 2008. Accuracy of linear measurements using dental cone beam and conventional multislice computed tomography. Dentomaxillofacial Radiology. 37: 10-17.
Tay, A. B., and J. R. Zuniga. 2007. Clinical characteristics of trigeminal nerve injury referrals to a university centre. International Journal of Oral and Maxillofacial Surgery. 36: 922-927.
Tyndall, D. A., J. B. Price, S. Tetradis, S. D. Ganz, C. Hildebolt, and W. C. Scarfe. 2012. Position statement of the american academy of oral and maxillofacial radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 113: 817-826.
Van Vlijmen, O. J., M. A. Kuijpers, S. J. Berge, J. G. Schols, T. J. Maal, H. Breuning, and A. M. Kuijpers-Jagtman. 2012. Evidence supporting the use of cone-beam computed tomography in orthodontics. Journal of the American Dental Association. 143: 241-252.
Walter, C., D. Kaner, D. C. Berndt, R. Weiger, and N. U. Zitzmann. 2009. Three-dimensional imaging as a pre-operative tool in decision making for furcation surgery. Journal of Clinical Periodontology. 36: 250-257.
Wood, R., Z. Sun, J. Chaudhry, B. C. Tee, D. G. Kim, B. Leblebicioglu, and G. England. 2013. Factors affecting the accuracy of buccal alveolar bone height measurements from cone-beam computed tomography images. American Journal of Orthodontics and Dentofacial Orthopedics. 143: 353-363.
Pathawee Khongkhunthian1*, Kanoknual Jomjunyong1 and Peter A. Reichart2
1 Center of Excellence for Dental Implantology, Faculty of Dentistry, Chiang Mai
University, Chiang Mai 50200, Thailand
2 Department of Oral Medicine, Dental Radiology and Oral Surgery, University
Medicine Berlin, CC3, Charité 10117, Berlin, Germany
*Corresponding author. Email: pathaweek@gmail.com
Total Article Views

