
Exploring Post-stroke Experiences of Thai Community-Dwelling Stroke Survivors and Family Caregivers: Implications for Enhancing Quality of Life
Waranya Chingchit, Sopida Apichai, Chirathip Thawisuk, Paweena Meenasak, Achiraya Chaikham*, and Jananya P. DhippayomPublished Date : October 20, 2025
DOI : https://doi.org/10.12982/NLSC.2026.014
Journal Issues : Number 1, January-March 2026
Abstract Stroke is one of the non-communicable diseases (NCDs) that is a serious global health concern because it is the leading cause of long-term disability and death, while the burden of stroke continues to increase. Stroke survivors should receive early rehabilitation that continues post-hospital discharge to improve their abilities and quality of life (QoL). Although Thailand has made advancements in its healthcare system at hospitals, the QoL of stroke survivors and their caregivers still needs to be improved through an understanding of their experiences and needs in the community context. This study aimed to explore the post-stroke experiences and needs of community-dwelling Thai stroke survivors and their primary family caregivers. A total of 16 participants (eight stroke survivors and their eight primary family caregivers) from both rural and urban areas of the Muang district, Lamphun province, Thailand, were recruited. Data was collected through semi-structured, in-depth face-to-face interviews and was analyzed using thematic analysis, applying both inductive and deductive approaches. Four key themes emerged: 1) changes after stroke; 2) impact after life changes from stroke; 3) perspectives on needs for well-being; and 4) barriers to achieve well-being. These findings provide valuable insights into the challenges and needs of Thai stroke survivors and their caregivers, emphasizing the importance of client-centered rehabilitation services that effectively address their specific requirements. Furthermore, the results support the establishment of community rehabilitation centers as an effective strategy to improve the QoL of community-dwelling Thai stroke survivors and their families.
Keywords: Stroke survivors, Caregivers, Community, Quality of life, Well-being
Graphical Abstract:

Funding: This study was supported by the Faculty of Associated Medical Sciences, Chiang Mai University research fund.
Citation: Chingchit, W., Apichai, S., Thawisuk, C., Meenasak, P., Chaikham, A., and Dhippayom, J.P. 2026. Exploring post-stroke experiences of Thai community-dwelling stroke survivors and family caregivers: Implications for enhancing quality of life. Natural and Life Sciences Communications. 25(1): e2026014.
INTRODUCTION
Stroke is an important health concern in Thailand, as it can lead to long-term disability and death. The incidence of acute stroke patients among individuals aged 15 and older has significantly increased from 172.33 to 328.00 per 100,000 population from 2009 to 2021 (Chantkran et al., 2021; Tiamkao et al., 2022). Stroke leads to impairments in physical and mental function, perception and cognition difficulties, activity limitations and restrictions in social participation, often resulting in stroke survivors becoming dependent on caregivers (Faria-Fortini et al., 2018; Silva et al., 2019; Tiwari et al., 2021). In addition to stroke survivors, family caregivers also experience limitations in their ability to participate in daily activities. The prolonged loss of activity can result in stroke caregivers having poor mental health and well-being (Bakas et al., 2017; Jellema et al., 2019).
Dysfunctions, particularly in physical and psychological health in stroke survivors, along with a lack of social support, negatively impact the quality of life (QoL) of both stroke survivors and their family members (Charfi, 2017; De Wit et al., 2017). However, the QoL of stroke survivors and their family caregivers is influenced by various factors, including predictors of QoL, such as socio-demographics, living conditions, the affective relationship between the stroke survivor and the caregiver, and the stroke survivor’s comorbidity. Mediators of QoL include physical functioning, complications in stroke survivors, caregiver burden, expenses of care, caregiving duration and time available for caregiving, and the mood state (anxiety and depression) of both stroke survivors and caregivers. Additionally, modulators of QoL, such as social support, continuity of stroke rehabilitation, and caregiving preparation, play a crucial role in determining overall well-being (Baumann et al., 2012; Savini et al., 2015).
Therefore, to improve the QoL of stroke survivors, family members and healthcare professionals should provide not only physical training but also a holistic approach to address their challenges. In Thailand, most stroke survivors initially receive care at the hospital, which then continues at homes under the supervision of the primary healthcare system in the community. However, a shortage of rehabilitation services has been reported in many countries, including Thailand, often resulting in limited rehabilitation training or short hospital stays (Suksathien, 2014; Chen et al., 2021), and a limited number of rehabilitation professionals, especially in rural areas (Pagaiya, 2018). Consequently, stroke survivors and their caregivers are at risk of facing challenges after hospital discharge due to a lack of caregiver skills, insufficient knowledge of post-stroke care and rehabilitation (Pitthayapong et al., 2017).
Recently, task shifting, community- and home-based rehabilitation, self-management and tele-rehabilitation have emerged as effective intervention models for stroke rehabilitation. These approaches require analysis within the context and structure of the healthcare system, as well as consideration of resource availability (Ekechukwu et al., 2020). Effective rehabilitation therapy can improve the QoL of stroke survivors, as disability level is a key factor influencing QoL (Yingkijsathavorn and Harnphadungkit, 2020). Providing disability training and financial support for caregivers of stroke survivors may enhance patient independence in activities of daily living (ADLs). This increased independence can reduce the caregiving burden, improving both the QoL and psychological health of caregivers (Chuluunbaatar et al., 2016). Among stroke survivors, diminished health-related QoL is associated with increased long-term unmet health needs (Lo et al., 2023).
A literature review highlighted that stroke survivors and their caregivers experience a lack of support due to their exclusion from services and have difficulty re-engaging, largely because of insufficient acquired knowledge and skills (Pindus et al., 2018). Perceived needs after stroke were associated with demographics, time since stroke onset, access to social care services, levels of disability and environmental factors (Chen et al., 2019). In ways consistent with the perspective of family caregivers, their needs include health information, professional healthcare support and a community support network (Tsai et al., 2015). These issues underscore the importance of rehabilitation in mitigating the impacts of stroke on survivors and their families.
Developing sustainable strategies to improve the QoL of stroke survivors and their caregivers requires an understanding of the experiences, barriers and needs within the community context. Although qualitative studies have explored the problems and needs of stroke survivors and their caregivers in communities (Petchroung and Jewpattanakul, 2014; Intamas et al., 2021), no study has been conducted in both the urban and rural areas of Lamphun province, which had the highest rate of people with disabilities in the country in 2019, 2020 and 2023 (The Lamphun Provincial Social Development and Human Security Office, 2020; 2021; 2023). The number of people with disabilities in Lamphun has increased gradually between 2016 and 2023. Moreover, the trend is likely to continue rising in the future (The Lamphun Provincial Social Development and Human Security Office, 2021; 2023).
Urban and rural areas of Lamphun differ in rehabilitation access. Urban residents benefit from public health service centers offering rehabilitation, free transport, and interdisciplinary home visits, while rural residents often rely on village health volunteers or Subdistrict Health Promoting Hospital staff. These disparities may shape QoL, as urban survivors typically access more consistent care, while rural survivors face greater barriers. Nationwide data confirm this divide, showing that rural community hospitals lack rehabilitation professionals and services, unlike better-resourced urban hospitals (Doungthipsirikul et al., 2015).
These gaps highlight the need to explore the post-stroke experiences of survivors and family caregivers in Lamphun. This study employed a qualitative approach to capture their lived experiences within the community, focusing on the problems, obstacles, and needs that shape their QoL. While not designed as a comparison, including participants from both urban and rural areas provides a broader perspective. Importantly, this article also offers potential strategies for enhancing QoL, reflecting issues commonly encountered by stroke survivors and family caregivers.
MATERIAL AND METHODS
Design
A qualitative study was conducted using semi-structured interviews to explore the experiences after stroke and needs of community-dwelling Thai stroke survivors and their primary family caregivers in Lamphun province. The focus was on their post-stroke experiences after discharge from the hospital to home until the time of the interview. This study received approval from the ethical review committee for research in humans, Faculty of Associated Medical Sciences (AMS), Chiang Mai University (CMU) (595/563). Participants provided written informed consent for their interviews to be audio-recorded and for data to be used in this study.
Participants
Stroke survivors and their family caregivers who lived in Muang district, Lamphun province, Thailand, were recruited using purposive sampling. The inclusion criteria for stroke survivors were: 1) diagnosis of stroke; 2) being 18 years of age or older; 3) having the ability to speak and understand the Thai language; and 4) normal perception and cognition (screened with Mental State Examination T10; MSET10) (Sangna et al., 2020). The inclusion criteria for family caregivers were: 1) being a primary caregiver for at least one month; 2) being at least 18 years of age; and 3) having the ability to speak and understand the Thai language. Stroke survivors were excluded if they were disabled from any disease(s) or complication(s) other than stroke.
Participants were recruited from both urban and rural areas. Urban areas were defined as those located within Mueang Lamphun Municipality, while all other areas in Mueang District outside the municipality were classified as rural. This definition follows national guidelines and the Community Development Department, Ministry of Interior, Thailand, which identify population density and income as key criteria for distinguishing urban from rural areas (Flood, 2000; National Statistical Office, 2021). Recruitment in urban areas was conducted through posters placed at the Muang Lamphun Municipal Public Health Center. Recruitment in rural areas was conducted through posters placed at Subdistrict Health Promoting Hospitals and study flyers distributed by village health volunteers. Interested participants were contacted by researchers and provided with detailed study information.
Data Collection
Stroke survivors and their family caregivers participated in separate face-to-face, in-depth interviews using a semi-structured guide. All participants chose to be interviewed in their own homes, which provided a comfortable and familiar environment. The interviews were conducted between December 2021 and March 2022. The interview questions were developed and pilot-tested with individuals who met the same inclusion criteria to ensure clarity and suitability. Both the development of interview questions and the interview process were carried out by two researchers (WC and AC) (Braun and Clarke, 2006). After obtaining signed consent forms, interviews were audio-recorded, and interviewers also took detailed field notes to capture contextual and non-verbal information. Demographic information, including age, gender, relationship of caregiver to stroke survivor, and time since stroke, was collected prior to the interviews to provide context for the sample. The majority of participants spoke Northern Thai dialect, while some used Standard/Central Thai during the interview. Each interview lasted approximately 30–45 minutes.
The semi-structured guide covered topics such as for the stroke survivors:
- Do you have problems or barriers about occupations when you got back home? If you have problems or barriers to doing occupations, please explain.
- What do you need to do? (In addition, you can do it now.)
- As you mention the need, do you know what you need to do to meet it or your well-being?
The semi-structured guides for family caregivers:
- Could you share the experience after he/she got a stroke? How do you help him/her?
- Do you have problems or barriers about occupations when he/she got back home?
- If you have problems or barriers to doing occupations, please explain.
- What do you need him/her to do? (In addition, he/she can do it now.)
- As you mention the need, do you know what you need to do to meet it or your well-being?
Data Analysis
Data from the in-depth interviews were transcribed verbatim and translated into English. Thematic analysis was used to analyze the qualitative data with cross-comparison conducted independently by researchers WC, PM and AC (Corbin and Strauss, 1990; Braun and Clarke, 2006). Both inductive and deductive approaches were applied to address the objectives of this study. The process of analysis included: 1) familiarization with the data; 2) generation of initial codes; 3) search for themes; 4) review of themes; 5) definition and naming of themes; and 6) production of the report. Data was analyzed longitudinally to capture the experiences and needs of both community-dwelling Thai stroke survivors and their primary family caregivers from hospital discharge until the time of the interview. Data saturation was considered reached when additional interviews no longer produced new codes or themes. Specifically, no new codes emerged across consecutive interviews, and thematic coverage was found to be consistent across participants, demonstrating adequate breadth and depth of the data. At this point, further data collection no longer generated novel insights, themes, or categories relevant to the research question (Hennink and Kaiser, 2022).
Trustworthiness
Strategies to ensure trustworthiness in this study using four general criteria include credibility, transferability, dependability, and confirmability. For credibility of the study, triangulation strategy was conducted. Researchers employ multiple data collection methods including interviews, observations, and previous study data to cross-verify findings. In terms of study’s transferability, thick descriptions strategy was employed by providing detailed contextual information about participants’ characteristics, research settings and data collection and analysis procedures. In addition, rigorous data collection and analysis techniques were implemented in methodological documentation process to ensure the study’s dependability by promoting consistency and reducing potential bias in the interpretation of findings. Moreover, member checking strategy to warrant confirmability of the study was carried out by requesting all participants to verify study results (Stahl and King, 2020; Ahmed, 2024).
RESULTS
The study involved eight dyads. Stroke survivors were aged between 38 and 79 years, with an equal number of males and females. The time since their stroke ranged from one to five years, with most having experienced a stroke within the past two years. The primary family caregivers were aged between 18 and 73 years. Most of them were female, and a majority were the daughters of the stroke survivors (Table 1).
Table 1. Demographic characteristics of participants.
|
No. |
Participants' hometown |
Information of stroke survivors (S) |
Information of family caregivers (F) |
|||||
|
Age |
Sex |
Time since stroke (years) |
Locomotion |
Age
|
Sex |
Relationship with stroke survivor |
||
|
1: S1-F1 |
Urban area |
79 |
Male |
1 |
Walker |
54 |
Male |
Son |
|
2: S2-F2 |
Urban area |
45 |
Male |
1 |
Walker |
44 |
Female |
Spouse |
|
3: S3-F3 |
Rural area |
75 |
Female |
2 |
Walker |
50 |
Female |
Daughter |
|
4: S4-F4 |
Rural area |
38 |
Male |
2 |
Bedridden |
18 |
Female |
Daughter |
|
5: S5-F5 |
Rural area |
65 |
Female |
1 |
Single cane |
43 |
Female |
Daughter |
|
6: S6-F6 |
Rural area |
56 |
Female |
2 |
Tripod cane |
58 |
Male |
Spouse |
|
7: S7-F7 |
Rural area |
50 |
Male |
5 |
Wheelchair |
24 |
Female |
Daughter |
|
8: S8-F8 |
Rural area |
44 |
Female |
1 |
Wheelchair |
73 |
Female |
Mother |
Four themes emerged as a result of the analysis. A schematic of the concepts arising from these themes and sub-themes is shown in Figure 1.
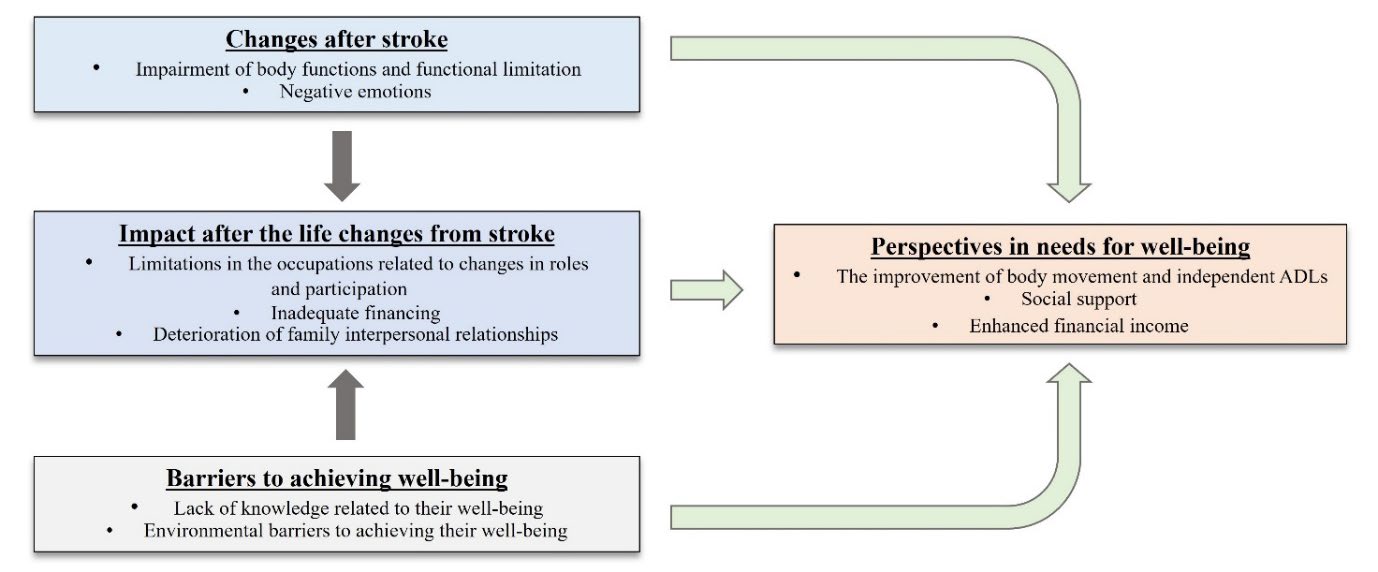
Figure 1. The experiences and needs of both community-dwelling Thai stroke survivors and their primary family caregivers.
Theme 1: Changes after stroke
The lives of stroke survivors and their family caregivers were abruptly altered by a stroke. The experiences of early post-stroke were analyzed into two sub-themes:
1) impairment of body functions and functional limitation; and 2) negative emotions.
Subtheme 1.1: Impairment of body functions and functional limitation
The impairment of body functions and functional limitation were the major problems mentioned by both stroke survivors and their primary family caregivers. Muscle weakness on one side of the stroke survivors’ body impacted their daily activities, such as sitting, standing, walking and communicating. In addition, impairment in sensation was also reported by stroke survivors, with half of the participants mentioning numbness or loss of sensation, resulting in further complications. Furthermore, some stroke survivors had complications after stroke, including seizures, urinary incontinence, bowel incontinence and pressure sores.
“I don’t know if you touch me, but I know when I feel a necessity to urinate or defecate… I had a seizure two times after my post-stroke... I cannot stand or sit because I have been lying on the bed for a long time...I had pressure sores at the bottom.” (S4)
Subtheme 1.2: Negative emotions
Impairments in body function and performance hinder stroke survivors’ ability to care for themselves and carry out routine tasks, placing a burden on their family caregivers and leading to negative emotions in stroke survivors. Fortunately, the negative emotions tended to diminish over time for both stroke survivors and their family caregivers, while the stroke survivors' functional abilities gradually improved as a result of adaptation. As one of the family caregivers expressed:
“After she had a stroke, it impacted my mental health in ways such as difficulty with transportation, lack of social participation in my village, and lack of income (F6)... We feel uncomfortable because it suddenly occurs, and we cannot adapt…now it is better, I can adapt.” (F6)
Theme 2: Impact after life changes from stroke
The majority of changes involved the bodily functions of stroke survivors that impacted both themselves and their family members. The analysis revealed three sub-themes, as follows:
Subtheme 2.1: Limitations in the occupations related to changes in roles and participation
Physical dysfunction and disability limited the occupational performance of stroke survivors, leading to changes in their former roles and participation. While the functional ability of almost all stroke survivors improved over time, these improvements did not fully restore their occupational performance. The roles of workers and housewives were identified as having been significantly negatively changed among those affected by a stroke. Some family caregivers lost their work roles, having been forced to resign from their jobs to provide care for the stroke survivors, even when the survivors had recovered and could perform more ADLs.
“After being discharged from the hospital, I was still unconscious and had to take supplemental oxygen for one month. In the early phase, my family caregivers helped me with everything, but now I can eat and groom independently and help my mother with dressing myself…I want to be better, and I want to return to work or help my mother prepare food ingredients for cooking and selling at a market.” (S8)
Subtheme 2.2: Inadequate financing
The loss of work roles among stroke survivors and/or family caregivers led to a decrease in income. Although the Thai government's policy provides financial support of THB 800 per month for people with disabilities, this amount was insufficient to cover their expenses. Consequently, they had to rely on further financial support from their son/daughter or other relatives. In this study, only one stroke survivor was able to earn a small income through online selling and speculation after their stroke.
“My father was the only worker in my family, I was a student when he had stroke… I don't know what to expect in the future, both from the disease of my father and my study that I will finish soon… Fortunately, my aunt helped me with the finances, and I had to get a part-time job.” (F7)
Subtheme 2.3: Deterioration of family interpersonal relationships
The impact of stroke widely affected not only the stroke survivors themselves but also their family relationships. The deterioration of family relationships stemmed from the stress and anxiety experienced by stroke survivors and/or the stress and fatigue of caregivers, which led to interpersonal relationship problems. Regrettably, in the worst case reported during the interviews, a primary caregiver mentioned that the stroke had led to divorce in their family.
“Since she had stroke, she was still a bedridden patient, and I had to take care of my daughter… Her husband broke up with her, divorced her, and left his sons behind, and I had to take care of her sons.” (F8)
Theme 3: Perspectives in needs for well-being
Key factors for improving the QoL among stroke survivors and caregivers were identified, including the improvement of body movement and independence in ADLs, social support and enhanced financial income.
Subtheme 3.1: The improvement of body movement and independent ADLs
The primary needs of both stroke survivors and their family caregivers were closely related to the physical functions and performance of the stroke survivors. The top two priority needs expressed by the participants were the improvement of body movement, followed by the ability to perform ADLs independently. Engaging in exercise or self-practice were essential for enhancing movement and overall functional abilities.
“I need my mother to improve body improvement, be ADL-independent, and go to the temple or participate in her social activities without returning to work... She has to exercise by herself intensively." (F5)
Subtheme 3.2: Social support
Although most stroke survivors had recovered from the stroke, the extent of their functional impairments varied. This variability highlighted the ongoing need for social and governmental support to enhance the well-being of both stroke survivors and their family caregivers. Key areas of support included expanding access to community rehabilitation centers, providing financial assistance, distributing medical supplies, and improving accessibility features, such as accessible toilets. The need for social support was influenced by both economic status and the severity of physical dysfunction. Unfortunately, disparities in access to rehabilitation services existed, as community rehabilitation centers established by the local administrative organizations and free transportation service from home to rehabilitation centers are available for people who have difficulties accessing rehabilitation centers were only available in the Mueang Lamphun town municipality area, which represented the urban area in this study. In addition, home visits are delivered by interdisciplinary healthcare teams within the Mueang Lamphun town municipality. While in rural areas or sub-district municipalities, limited access to healthcare services and ongoing rehabilitation from medical professionals was found. Home visits were delivered by village health volunteers or Subdistrict Health Promoting Hospital personnel following stroke survivors’ care plans. As a result, stroke survivors may lack the opportunity to access rehabilitation services and related healthcare information, such as healthcare advice or rights and welfare, to promote QoL. This geographic gap in service availability may have contributed to inequalities in recovery outcomes and long-term well-being for stroke survivors in rural communities.
“I want someone to help me with rehabilitation. Previously, a physical therapy student had trained me, but she moved to another province… Now, I receive rehabilitation at the hospital monthly." (S8)
“I want any institute to support medical consumables such as adult diapers, normal saline solutions, surgical cotton, and medical glove for the care of my father." (F4)
Subtheme 3.3: Enhanced financial income
The loss of income due to stroke survivors and/or primary family caregivers leaving work, combined with rising expenses for treatment, transportation, medical equipment and consumables, such as adult diapers, highlighted the need for increased financial support to improve the QoL of stroke survivors and their caregivers.
“I want to return to work and do my housework to help my daughter. Since I had a stroke, I and my husband did not get jobs…My husband had to care for me all the time…My daughter has to take time off to take me to follow-ups at the hospital." (S6)
Theme 4: Barriers to achieving well-being
The two primary barriers impacting the QoL of stroke survivors and caregivers were a lack of knowledge related to their well-being and environmental barriers that hindered their well-being.
Subtheme 4.1: Lack of knowledge related to their well-being
A lack of knowledge about rehabilitation, including exercise and appropriate ADL training methods for stroke patients, was a significant barrier to improving body movement and ADL function. Additionally, access to organizations providing information on social support was limited. Almost all participants, both stroke survivors and their primary family caregivers, raised this issue based on their personal experiences with these challenges.
"I am lacking in knowledge about stroke care because I was not the primary caregiver, and the health professionals did not explain the methods of care... The hospital's health professionals explained stroke patient care techniques to my other daughter, who served as the primary caregiver for the first two months after her discharge from the hospital… After that, my daughter taught me about stroke care before I became primary caregiver… I want any organization to help with health problems, but I don't know who it will be." (F8)
Subtheme 4.2: Environmental barriers to achieving their well-being
All stroke survivors faced greater challenges in resuming work and daily activities after hospital discharge due to physical barriers in their homes that hindered independence and social participation. These barriers included uneven ground, stairs, steps and outhouse bathrooms, which were especially problematic as most stroke participants continued to experience mobility difficulties.
“Recently, I had to use my bottom to slide step by step on the stairs from the 2nd floor to the 1st floor because my bedroom is on the second floor, and I preferred to stay on the 2nd floor for sleep…the restroom and bathroom are only on the 1st floor.” (S6)
DISCUSSION
This study provides valuable insights into the experiences and needs of Thai stroke survivors and their primary family caregivers who live in the community in Lamphun province, Thailand. The qualitative data revealed not only their perspectives on experiences and needs but also the barriers that hindered a better understanding of their stories. Notably, both stroke survivors and their primary family caregivers shared similar perspectives regarding their experiences and needs.
Changes after stroke: It is well known that stroke causes several neurological impairments of body functions due to damage to different regions of the brain, particularly the paralysis of muscles that limit movement on one side of the body, which is the most common impairment found in stroke patients. (Li, 2017; Murphy and Werring, 2020; Liu et al., 2023). Following a stroke, reduced physical abilities cause a deterioration in self-image and being a burden to their caregivers about ADL performance, indicating dissatisfaction with this situation among stroke survivors (Chau et al., 2022; Lin et al., 2022; Mohotlhoane and Nemakanga, 2023). Additionally, family caregivers not only cared for their family members after a stroke but also took on tasks previously performed by stroke survivors that are associated with anxiety, stress, depression, and burden (Hu et al., 2018; Lin et al., 2022). Consistent with previous studies, this study found that stroke survivors experienced significant changes after stroke, including physical impairments that affected their daily activities. These impairments also impacted on the emotional well-being of both stroke survivors and their family caregivers, particularly after hospital discharge.
Impact after life changes from stroke: Most stroke survivors still require assistance from caregivers to complete daily tasks, as partial recovery of bodily functions and environmental barriers limit their occupational performance and social participation. As a result, the roles of stroke survivors, such as providing care and financial support for the family, often shift to other family members. Consequently, family caregivers must take on additional responsibilities, including household income generation and caregiving duties. This shift places financial strain on families, as caregiving expenses increase while the household income decreases. Several studies have also identified financial burden as one of the most significant challenges for families of stroke survivors (Mishra et al., 2016; Lin et al., 2022; Hu et al., 2023). The change in bodily functions of stroke survivors, along with adverse impacts after changes from stroke, lead to deterioration in family relationships. The relationship problems between stroke survivors and their family members involve adaptation to a caregiver’s role, a reduction in time for leisure and social activities, and a lack of social support (Cobley et al., 2013; Chau et al., 2022).
Perspectives in needs for well-being: The needs of community-dwelling Thai stroke survivors and their primary family caregivers were highlighted, along with the negative experiences and environmental barriers they faced. Most participants expressed a strong desire to regain movement and improve bodily functions to restore independence or reduce reliance on caregivers. While all participants recognized the importance of rehabilitation, they emphasized the need for greater social support in accessing rehabilitation services and receiving education from healthcare professionals on post-discharge stroke care. Evidence indicates that continuous rehabilitation therapy after hospital discharge is essential for improving functional ability and QoL in people with disabilities (Chalermwannapong et al., 2010; Petchroung and Jewpattanakul, 2014; Intamas et al., 2021; Purton et al., 2023). To improve the QoL of both stroke survivors and their family caregivers, community rehabilitation services should integrate local resources, policies and healthcare organizations (Petchroung and Jewpattanakul, 2014; Intamas et al., 2021). Additionally, this study highlights the importance of providing essential medical supplies for bedridden patients and ensuring financial assistance for individuals with disabilities under existing Thai government policies.
Barriers to achieving well-being: Although almost all the needs of stroke survivors and their family caregivers in this study were based on reality, some needs had unrealistic expectations about the body's functional recovery. These results reflect a lack of knowledge and information about stroke. This overly-optimistic expectation might be a coping mechanism that reflects the psychological needs of stroke patients and caregivers. Thus, it is necessary to encourage realistic expectations and provide accurate information about recovery (Wiles et al., 2002). According to the previously stated data, one of the most important barriers to living with disabilities after stroke in both stroke survivors and their family caregivers was a lack of knowledge about how to meet their needs, particularly any information related to existing institutions or government sectors that deal with these matters. Both patients and family caregivers need social support to improve their QoL (Suttiwong et al., 2018; Butsing et al., 2019; Chau et al., 2022).
According to the literature, there are several types of services available for people with disabilities living in the community. One of these is community-based rehabilitation (CBR), which has the potential to significantly enhance the QoL of stroke survivors and their caregivers by providing accessible, sustainable rehabilitation services. CBR is widely recognized as an effective strategy for improving rehabilitation access in communities (World Health Organization, 2022). Previous research and practical experience suggested that the establishment of community rehabilitation centers could enhance mobility, daily functioning, cognitive abilities, mental health, social participation and the ability to return to work. Furthermore, these centers helped reduce caregiver burden and stress, leading to improved well-being for caregivers (Ru et al., 2017; Chinchai et al., 2020; Syed et al., 2022; Chinchai et al., 2024). Research conducted in Thailand has shown that the majority of stroke survivors and their family caregivers were highly satisfied with rehabilitation education provided by community-based medical professionals (Kongsri et al., 2024). In addition, the development and implementation of relevant local governmental policies and support for stroke survivors, such as free transportation service from home to hospital or rehabilitation centers, as well as access to medical supplies and assistive devices, may help stroke survivors receive continuous rehabilitation services while alleviating burdens for caregivers. Therefore, these findings highlight the importance of integrating rehabilitation centers into communities as a key component of CBR, which would be beneficial in improving the QoL of both stroke survivors and their caregivers.
RESEARCH TO PRACTICE IMPLICATIONS
The findings of this study highlight the relationship between the experiences and needs of community-dwelling Thai stroke survivors and their family caregivers. The presence of a community rehabilitation center within the municipality offers significant advantages for both groups, as it addresses a wide range of needs. The center provides regular rehabilitation therapy, ensures access to medical services close to home, and employs staff to offer guidance and coordination with relevant agencies. For example, they assist with registration for a Disabled Person ID card and provide assistive devices, ultimately promoting a better QoL. These findings underscore the critical role of social support, particularly from the local and central governments, in meeting the needs of stroke survivors and their families. Establishing community rehabilitation centers can significantly enhance their well-being. Despite Thailand's efforts to expand community health services through the Universal Health Coverage (UHC) scheme and primary care units, most primary care units lack rehabilitation services (Kitreerawutiwong et al., 2017). Furthermore, a shortage of healthcare professionals, particularly in rural areas, combined with government policies that do not prioritize rehabilitation for individuals with disabilities, has led to service deficiencies (Kitreerawutiwong et al., 2017). In addition, potential barriers were lack of basic knowledge and experience of rehabilitation centers administration such as budget execution, procurement of equipment, health personnel contracting, and transportation service providing.
Addressing these gaps should be a priority for local governments. Establishing community rehabilitation centers would provide substantial benefits for stroke survivors, family caregivers and individuals with physical disabilities, including the increasing proportion of elderly individuals in Thailand. Feasible strategies to address these barriers include combining professional and community resources to ensure continuity of care. Home visits by occupational therapists and physical therapists, conducted together with village health volunteers within the first month after hospital discharge, have been shown to improve stroke survivors’ ADL performance and quality of life when volunteers are adequately trained (Pakdee and Chinchai, 2016). Thereafter, tele-rehabilitation may be used for follow-up and adjustment of home programs every one to two months for families with sufficient access and readiness. Rural Thai community health volunteers have reported positive attitudes and high satisfaction toward a tele-stroke rehabilitation platform, highlighting its feasibility for extending follow-up care in underserved areas (Kongsawasdi et al., 2025). For families not ready for tele-rehabilitation, village health volunteers could provide in-person follow-up during the first months after discharge, with subsequent visits adjusted to every three to six months as appropriate. In addition, education and structured training for village health volunteers in basic stroke rehabilitation and caregiver support are essential for sustaining community-based stroke care (Chinchai et al., 2024).
IMPLICATION FOR FUTURE RESEARCH
Future studies should explore additional clinical characteristics of stroke survivors and examine different geographical and contextual settings. A larger, randomly selected sample would represent the larger population, allowing more accurate inferences and generalizations. Furthermore, future study should expand into quantitative research for generalization to a larger population in different settings
LIMITATIONS
This study has several limitations. First, it was conducted within a small geographical area, which may limit generalizability, though participants from both urban and rural areas provided some contextual diversity. Second, reliance on self-reported data may have introduced social desirability bias; this was mitigated by triangulating with field notes, observations, village health volunteer reports, and participants’ demonstrations (Althubaiti, 2016). Third, although interviews were conducted in Thai and translated into English, translation bias remains a possibility despite efforts such as verbatim transcription, cross-checking, and team review. Finally, interviewer influence cannot be entirely excluded, but the use of trained interviewers and peer debriefing helped minimize this risk.
CONCLUSIONS
This qualitative study demonstrates that life after a stroke is a shared family experience in Thai communities. Physical limitations and emotional distress disrupt roles and routines, transferring responsibilities to primary caregivers while causing financial strain and relationship tensions. Survivors prioritized regaining mobility and independence in daily activities, while both survivors and caregivers emphasized the importance of social support and financial stability in order to improve their QoL. These priorities were limited by knowledge gaps and environmental constraints. The CBR model, especially the community rehabilitation centers, is an effective strategy to improve QoL for both survivors and caregivers by mainly focusing on rehabilitation to restore physical functions and abilities in the ADLs of stroke survivors. Additionally, it can further ameliorate the impact of stroke and reduce barriers to achieving well-being in the future.
ACKNOWLEDGEMENTS
The authors are grateful to all participants for their contribution to this research.
AUTHOR CONTRIBUTIONS
Conceptualization: WC, JPD, SA, CT, AC; Funding acquisition: WC, JPD, SA; Investigation: WC, AC; Formal analysis: WC, PM, AC; Supervision: JPD; Writing – original draft: WC; Writing – review and editing: WC, JPD, SA, CT, PM, AC. All authors have read and approved of the final manuscript.
CONFLICT OF INTEREST
The authors declare that they hold no competing interests.
REFERENCES
Ahmed, S.K. 2024. The pillars of trustworthiness in qualitative research. Journal of Medicine, Surgery, and Public Health. 2: 100051. https://doi.org/10.1016/j.glmedi.2024.100051
Althubaiti A. 2016. Information bias in health research: Definition, pitfalls, and adjustment methods. Journal of Multidisciplinary Healthcare. 9: 211-217. https://doi.org/10.2147/JMDH.S104807
Bakas, T., McCarthy, M., and Miller, E.T. 2017. Update on the state of the evidence for stroke family caregiver and dyad interventions. Stroke. 48(5): e122-e125. https://doi.org/10.1161/STROKEAHA.117.016052
Baumann, M., Lurbe, K., Leandro, M.E., and Chau, N. 2012. Life satisfaction of two-year post-stroke survivors: Effects of socio-economic factors, motor impairment, Newcastle stroke-specific quality of life measure and world health organization quality of life: Bref of informal caregivers in Luxembourg and a rural area in Portugal. Cerebrovascular Diseases. 33(3): 219-230. https://doi.org/10.1159/000333408
Braun, V. and Clarke, V. 2006. Using thematic analysis in psychology. Qualitative Research in Psychology. 3(2): 77-101. https://doi.org/10.1191/1478088706qp063oa
Butsing, N., Tipayamongkholgul, M., Ratanakorn, D., Suwannapong, N., and Bundhamcharoen, K. 2019. Social support, functional outcome and quality of life among stroke survivors in an urban area. Journal of Pacific Rim Psychology. 13: e4. https://doi.org/10.1017/prp.2019.2
Chalermwannapong, S., Panuthai, S., Srisuphan, W., Panya, P., and Ostwald, S.K. 2010. Effects of the transitional care program on functional ability and quality of life of stroke survivors. Chiang Mai University Journal of Natural Sciences. 9: 49-66.
Chantkran, W., Chaisakul, J., Rangsin, R., Mungthin, M., and Sakboonyarat, B. 2021. Prevalence of and factors associated with stroke in hypertensive patients in Thailand from 2014 to 2018: A nationwide cross-sectional study. Scientific Reports. 11(1): 17614. https://doi.org/10.1038/s41598-021-96878-4
Charfi, N., Trabelsi, S., Turki, M., Mâalej Bouali, M., Zouari, L., Dammak, M., Ben Thabet, J., Mhiri, C., and Mâalej, M. 2017. Impact du handicap physique et des troubles émotionnels concomitants sur la qualité de vie en post-AVC [Impact of physical disability and concomitant emotional disturbances on post-stroke quality of life]. L'Encephale. 43(5): 429-434. https://doi.org/10.1016/j.encep.2016.05.014
Chau, J.P.C., Lo, S.H.S., Butt, L., and Liang, S. 2022. Post-stroke experiences and rehabilitation needs of community-dwelling Chinese stroke survivors: A qualitative study. International Journal of Environmental Research and Public Health. 19(23): 16345. https://doi.org/10.3390/ijerph192316345
Chen, L., Xiao, L. D., Chamberlain, D., and Newman, P. 2021. Enablers and barriers in hospital-to-home transitional care for stroke survivors and caregivers: A systematic review. Journal of Clinical Nursing. 30(19-20): 2786-2807. https://doi.org/10.1111/jocn.15807
Chen, T., Zhang, B., Deng, Y., Fan, J. C., Zhang, L., and Song, F. 2019. Long-term unmet needs after stroke: Systematic review of evidence from survey studies. BMJ Open. 9(5): e028137. https://doi.org/10.1136/bmjopen-2018-028137
Chinchai, P., Sirisatayawong, P., and Jindakum, N. 2020. Community integration and quality of life: Stroke survivors as recipients of rehabilitation by village health volunteers (VHVs) in Thailand. Occupational Therapy in Health Care. 34(3): 277-290. https://doi.org/10.1080/07380577.2020.1773010
Chinchai, P., Kongsawasdi, S., Sirisatayawong, P., Apichai, S., Chuatrakoon, B., and Thonglorm, N. 2024. Community rehabilitation by the trained village health volunteers on activities of daily living and quality of life in stroke survivors. Journal of Associated Medical Sciences. 57(2): 157-165. https://doi.org/10.12982/JAMS.2024.038
Chuluunbaatar, E., Chou, Y.J., and Pu, C. 2016. Quality of life of stroke survivors and their informal caregivers: A prospective study. Disability and Health Journal. 9(2): 306-312. https://doi.org/10.1016/j.dhjo.2015.10.007
Cobley, C.S., Fisher, R.J., Chouliara, N., Kerr, M., and Walker, M.F. 2013. A qualitative study exploring patients' and carers' experiences of early supported discharge services after stroke. Clinical Rehabilitation. 27(8): 750-757. https://doi.org/10.1177/0269215512474030
Corbin, J.M. and Strauss, A. 1990. Grounded theory research: Procedures, canons, and evaluative criteria. Qualitative Sociology. 13: 3-21. https://doi.org/10.1007/BF00988593
De Wit, L., Theuns, P., Dejaeger, E., Devos, S., Gantenbein, A.R., Kerckhofs, E., Schuback, B., Schupp, W., and Putman, K. 2017. Long-term impact of stroke on patients' health-related quality of life. Disability and Rehabilitation. 39(14): 1435-1440. https://doi.org/10.1080/09638288.2016.1200676
Doungthipsirikul, S., Sirisamutr, T., Kotirum, S., Pilasant, S., Tantipisitkul, K., Tantivess, S., and Teerawattananon, Y. 2015. Medical rehabilitation services for people living with disabilities in Thailand: Current situations in public hospitals. Journal of Health Systems Research. 9(4): 334-343.
Ekechukwu, E.N.D., Olowoyo, P., Nwankwo, K.O., Olaleye, O.A., Ogbodo, V.E., Hamzat, T.K., and Owolabi, M.O. 2020. Pragmatic solutions for stroke recovery and improved quality of life in low- and middle-income countries-a systematic review. Frontiers in Neurology. 11: 337. https://doi.org/10.3389/fneur.2020.00337
Faria-Fortini, I., Basílio, M.L., Scianni, A.A., Faria, C.D.C.M., and Teixeira-Salmela, L.F. 2018. Performance and capacity-based measures of locomotion, compared to impairment-based measures, best predicted participation in individuals with hemiparesis due to stroke. Disability and Rehabilitation. 40(15): 1791-1798. https://doi.org/10.1080/09638288.2017.1312570
Flood, J. 2000. Defining urban areas in Thailand. Office of National Economic and Social Development Board, Thailand.
Hennink, M. and Kaiser, B.N. 2022. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Social Science & Medicine. 292: 114523. https://doi.org/10.1016/j.socscimed.2021.114523
Hu, P., Yang, Q., Kong, L., Hu, L., and Zeng, L. 2018. Relationship between the anxiety/depression and care burden of the major caregiver of stroke patients. Medicine. 97(40): e12638. https://doi.org/10.1097/MD.0000000000012638
Hu, Y., Qiu, X., Ji, C., Wang, F., He, M., He, L., and Chen, L. 2023. Post-stroke experiences and health information needs among Chinese elderly ischemic stroke survivors in the internet environment: A qualitative study. Frontiers in Psychology. 14: 1150369. https://doi.org/10.3389/fpsyg.2023.1150369
Intamas, U., Rawiworrakul, T., Amnatsatsue, K., Nanthamongkolchai, S., and Palmer, M.H. 2021. Care of stroke survivors in community: A case study of rural Thai community. Journal of Health Research. 35(1): 77-87. https://doi.org/10.1108/JHR-07-2019-0172
Jellema, S., Wijnen, M.A.M., Steultjens, E.M.J., Nijhuis-van der Sanden, M.W.G., and van der Sande, R. 2019. Valued activities and informal caregiving in stroke: A scoping review. Disability and Rehabilitation. 41(18): 2223-2234. https://doi.org/10.1080/09638288.2018.1460625
Kitreerawutiwong, N., Jordan, S., and Hughes, D. 2017. Facility type and primary care performance in sub-district health promotion hospitals in Northern Thailand. PloS one. 12(3): e0174055. https://doi.org/10.1371/journal.pone.0174055
Kongsawasdi, S., Chuatrakoon, B., Konghakote, S., Puangkham, T., and Wantanajittikul, K. 2025. Exploring attitudes and satisfaction of rural Thai community health volunteers toward a tele-stroke rehabilitation platform. Physical and Occupational Therapy in Geriatrics. 43(3): 218-231. https://doi.org/10.1080/02703181.2025.2453932
Kongsri, I., Chuaynoo, N., Chinchai, P., Sirisatayawong, P., Apichai, S., and Chingchit, W. 2024. Educational media utilization for rehabilitation among community-dwelling stroke survivors and their caregivers: A pilot study. Journal of Associated Medical Sciences. 57(3): 204-211. https://doi.org/10.12982/JAMS.2024.062
Li, S. 2017. Spasticity, motor recovery, and neural plasticity after stroke. Frontiers in Neurology. 8: 120. https://doi.org/10.3389/fneur.2017.00120
Lin, S., Wang, C., Wang, Q., Xie, S., Tu, Q., Zhang, H., Peng, M., Zhou, J., and Redfern, J. 2022. The experience of stroke survivors and caregivers during hospital-to-home transitional care: A qualitative longitudinal study. International Journal of Nursing Studies. 130: 104213. https://doi.org/10.1016/j.ijnurstu.2022.104213
Liu, Y., Yin, J.H., Lee, J.T., Peng, G.S., and Yang, F.C. 2023. Early rehabilitation after acute stroke: The golden recovery period. Acta Neurologica Taiwanica. 32:1-8.
Lo, S.H.S., Chau, J.P.C., Lam, S.K.Y., and Saran, R. 2023. Understanding the priorities in life beyond the first year after stroke: Qualitative findings and non-participant observations of stroke survivors and service providers. Neuropsychological Rehabilitation. 33(5): 794-820. https://doi.org/10.1080/09602011.2022.2049827
Mishra, A.K., Mishra, N., and Gajjar, K. 2016. Financial burden of stroke on family and caregiver in India: A literature review. International Journal of Research in Medical Sciences. 4(9): 3675-3678. https://doi.org/10.18203/2320-6012.ijrms20162900
Mohotlhoane, R. and Nemakanga, M.N. 2023. Barriers experienced by stroke survivors when participating in meaningful occupations in a rural and semirural community. South African Journal of Occupational Therapy. 53(1): 92-100. https://doi.org/10.17159/2310-3833/2023/vol53n1a10
Murphy, S.J. and Werring, D.J. 2020. Stroke: Causes and clinical features. Medicine. 48(9): 561-566. https://doi.org/10.1016/j.mpmed.2020.06.002
National Statistical Office. 2021. Reporting to a study of guideline for the defining urban and rural areas in Thailand. Ministry of Digital Economy and Society, Thailand. https://gdcatalog.go.th/dataset/gdpublish-0210-01-0001
Pagaiya, N., Khaonuan, B., Phanthunane, P., Bamrung, A., and Jirawattanapisal, T. 2018. Human resources for health projections for primary health care services in Thailand 2026. Journal of Health Systems Research. 12(2): 189-204.
Pakdee, P. and Chinchai, P. 2016. The influence of home visit program on functional abilities and quality of life in persons with disabilities resulting from stroke. Journal of Associated Medical Sciences. 49(2): 276. https://doi.org/10.14456/jams.2016.24
Petchroung, N. and Jewpattanakul, Y. 2014. Problems and needs of stroke patients and caregivers in primary care unit. Journal of Nursing Science and Health. 37(4): 37-45.
Pindus, D.M., Mullis, R., Lim, L., Wellwood, I., Rundell, A.V., Abd Aziz, N.A., and Mant, J. 2018. Stroke survivors' and informal caregivers' experiences of primary care and community healthcare services - A systematic review and meta-ethnography. PLoS One. 13(2): e0192533. https://doi.org/10.1371/journal.pone.0192533
Pitthayapong, S., Thiangtam, W., Powwattana, A., Leelacharas, S., and Waters, C.M. 2017. A community based program for family caregivers for post stroke survivors in Thailand. Asian Nursing Research. 11(2): 150-157. https://doi.org/10.1016/j.anr.2017.05.009
Purton, J., Sim, J., and Hunter, S.M. 2023. Stroke survivors' views on their priorities for upper-limb recovery and the availability of therapy services after stroke: A longitudinal, phenomenological study. Disability and Rehabilitation. 45(19): 3059-3069. https://doi.org/10.1080/09638288.2022.2120097
Ru, X., Dai, H., Jiang, B., Li, N., Zhao, X., Hong, Z., He, L., and Wang, W. 2017. Community-based rehabilitation to improve stroke survivors' rehabilitation participation and functional recovery. American Journal of Physical Medicine and Rehabilitation. 96(7): e123-e129. https://doi.org/10.1097/PHM.0000000000000650
Sangna, R., Pinyopornpanish, K., Jiraporncharoen, W., and Angkurawaranon, C. 2020. Validation of a 14-item self-reporting questionnaire for the screening of dementia in the elderly. Journal of Mental Health of Thailand. 28: 199-210.
Savini, S., Buck, H.G., Dickson, V.V., Simeone, S., Pucciarelli, G., Fida, R., Matarese, M., Alvaro, R., and Vellone, E. 2015. Quality of life in stroke survivor-caregiver dyads: A new conceptual framework and longitudinal study protocol. Journal of Advanced Nursing. 71(3): 676-687. https://doi.org/10.1111/jan.12524
Silva, S.M., Corrêa, J.C.F., Pereira, G.S., and Corrêa, F.I. 2019. Social participation following a stroke: An assessment in accordance with the international classification of functioning, disability and health. Disability and Rehabilitation. 41(8): 879-886. https://doi.org/10.1080/09638288.2017.1413428
Stahl, N.A. and King, J.R. 2020. Expanding approaches for research: Understanding and using trustworthiness in qualitative research. Journal of Developmental Education. 44: 26-28. http://www.jstor.org/stable/45381095
Suksathien, R. 2014. Accessibility to medical rehabilitation service for acute stroke at Maharat Nakhon Ratchasima hospital: Related factors and outcomes. ASEAN Journal of Rehabilitation Medicine. 24(2): 37-43.
Suttiwong, J., Vongsirinavarat, M., and Hiengkaew, V. 2018. Predictors of community participation among individuals with first stroke: A Thailand study. Annals of Rehabilitation Medicine. 42(5): 660-669. https://doi.org/10.5535/arm.2018.42.5.660
Syed, Z., De Bastos, M., Pindela, C., Sutherland, S., Melis, S., Wort, B., and Shohsa, T. 2022. A rapid review of the roles of community rehabilitation workers in community-based mental health services in low- and middle-income countries. Disability, CBR and Inclusive Development. 33(2): 108-128. https://doi.org/10.47985/dcidj.537
The Lamphun provincial social development and human security office. 2020. Lamphun province social situation report 2020.
The Lamphun provincial social development and human security office. 2021. Lamphun province social situation report 2021.
The Lamphun provincial social development and human security office. 2023. Lamphun province social situation report 2023.
Tiamkao, S., Ienghong, K., Cheung, L.W., Celebi, I., Suzuki, T., and Apiratwarakul, K. 2022. Stroke incidence, rate of thrombolytic therapy, mortality in Thailand from 2009 to 2021. Open Access Macedonian Journal of Medical Sciences. 10(E): 110-115. https://doi.org/10.3889/oamjms.2022.8051
Tiwari, S., Joshi, A., Rai, N., and Satpathy, P. 2021. Impact of stroke on quality of life of stroke survivors and their caregivers: A qualitative study from India. Journal of Neurosciences in Rural Practice. 12(4): 680-688. https://doi.org/10.1055/s-0041-1735323
Tsai, P.C., Yip, P.K., Tai, J.J., and Lou, M.F. 2015. Needs of family caregivers of stroke patients: A longitudinal study of caregivers' perspectives. Patient Preference and Adherence. 9: 449-457. https://doi.org/10.2147/PPA.S77713
World Health Organization. 2022. Achieving well-being: A global framework for integrating well-being into public health utilizing a health promotion approach.
Wiles, R., Ashburn, A., Payne, S., and Murphy, C. 2002. Patients' expectations of recovery following stroke: A qualitative study. Disability and Rehabilitation. 24(16): 841-850. https://doi.org/10.1080/09638280210142158
Yingkijsathavorn, A. and Harnphadungkit, K. 2020. Quality of life in stroke patients at outpatient rehabilitation clinic, Siriraj hospital. ASEAN Journal of Rehabilitation Medicine. 30(3): 123-128.
OPEN access freely available online
Natural and Life Sciences Communications
Chiang Mai University, Thailand. https://cmuj.cmu.ac.th
Waranya Chingchit1, Sopida Apichai1, Chirathip Thawisuk1, Paweena Meenasak2, Achiraya Chaikham1, *, and Jananya P. Dhippayom1
1 Department of Occupational Therapy, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai 50200, Thailand.
2 Otto Bock South East Asia Co., Ltd., Bangkok 10900, Thailand.
Corresponding author: Achiraya Chaikham, E-mail: achiraya.ch@cmu.ac.th
ORCID iD:
Waranya Chingchit: https://orcid.org/0009-0000-5168-0665
Sopida Apichai: https://orcid.org/0000-0002-7235-8891
Chirathip Thawisuk: https://orcid.org/0000-0001-7650-617X
Achiraya Chaikham: https://orcid.org/0000-0001-5896-4695
Jananya P. Dhippayom: https://orcid.org/0000-0003-4739-2630
Total Article Views
Editor: Decha Tamdee,
Chiang Mai University, Thailand
Article history:
Received: May 30, 2025;
Revised: October 3, 2025;
Accepted: October 14, 2025;
Online First: October 20, 2025

