
Surface Roughness and Microhardness of Heat-Cured, Milled, and 3D-Printed Occlusal Splints: A Comparative Study of Unpolished and Polished Surfaces
Uthai Uma*, Jirayu Chansri, Thitiphat Itthipornpaisan, and Trin ThahongPublished Date : April 29, 2025
DOI : https://doi.org/10.12982/NLSC.2025.041
Journal Issues : Number 3, July-September 2025
Abstract This study aimed to evaluate the variations in surface roughness and microhardness among different occlusal splint materials and compare these properties between their unpolished and polished surfaces. Seventy-two specimens (10×10×5 mm3) were made using three methods: heat-cured (HC) (Meliodent-Heat Cure, Kulzer), milled (ML) (Smile-Cam, Pressing Dental SRL), and 3D-printed (3D) (MED610, Stratasys). One side of each specimen was polished using 600-, 800-, and 1000-grit sandpaper, followed by pumice and tallow. The surface roughness (Ra) was determined on 36 specimens (12 per group), and the Vickers microhardness (HV) was determined on the remaining specimens. Statistical analysis was done using SPSS 29.0. The Ra values for the unpolished surfaces demonstrated significant differences (P < 0.001), with 3D < ML < HC. Similarly, the polished surfaces also displayed significant differences (P < 0.001), with ML < HC < 3D. The polishing reduced Ra for HC and ML, but increased Ra for 3D (P < 0.05). Regarding the HV values, the unpolished surfaces had significantly different values (P < 0.001), with ML > HC > 3D, and the same trend was observed for the polished surfaces (P < 0.001). However, no significant differences in HV were found between the polished and unpolished surfaces. In conclusion, significant differences in surface roughness and microhardness were observed among the three occlusal splint materials. Polishing differentially affected the surface roughness depending on the material, underscoring the importance of material selection and polishing protocols for optimal splint fabrication.
Keywords: Occlusal splint, Dental materials, Heat-cured, Milled, 3D-printed
Funding: This work was supported by the Dental Research Fund, Dental Research Project, Faculty of Dentistry, Chulalongkorn University, Bangkok, Thailand, under Grant [Number 3200502#10/2023].
Citation: Uma, U., Chansri, J., Itthipornpaisan, T., and Thahong, T. 2025. Surface roughness and microhardness of heat-cured, milled, and 3D-printed occlusal splints: A comparative study of unpolished and polished surfaces. Natural and Life Sciences Communications. 24(3): e2025041.
INTRODUCTION
Occlusal splints are available in various types, including flat plane stabilizing splints, anterior repositioning splints, anterior bite planes, posterior bite planes, distraction splints, soft rubber splints, and hydrostatic splints (Albagieh et al., 2023). Each type is designed for specific clinical applications and offers distinct advantages depending on the patient's condition and treatment goals. Occlusal splints help to evenly distribute occlusal forces and alleviate the symptoms of temporomandibular disorders (Ahmed et al., 2023; Minervini et al., 2023; Orzeszek et al., 2023; Rongo et al., 2023; Ding et al., 2024) and bruxism (Hardy and Bonsor, 2021; Kolcakoglu et al., 2022; Uma et al., 2024). Despite being in use for a long time, the occlusal splint has recently experienced renewed interest and application (Crout, 2017).
Occlusal splints can be manufactured using various methods, comprising conventional techniques (heat-curing and vacuum forming) and digital techniques (milling and 3D-printing) (Nassif et al., 2023). Although conventional techniques have long been used to fabricate occlusal splints, the use of digital workflow is now increasingly prevalent in dentistry due to its accuracy (Blasi, Henarejos-Domingo, Palacios-Banuelos, Aparicio, et al., 2023; Orgev et al., 2023) and minimal need for adjustment (Blasi, Henarejos-Domingo, Palacios-Banuelos, Vidal-Ponsoda, et al., 2023). This approach employs a combination of computer-aided design (CAD) and computer-aided manufacturing (CAM) for occlusal splint fabrication (American College of Prosthodontists and ACP Education Foundation, 2021; Layton et al., 2023). The dental materials used in digital techniques differ from those used in conventional methods (Zafar, 2020; Nassif et al., 2023), and these transformative materials should be thoroughly evaluated before being prescribed to patients.
The fabrication techniques used for these splints can markedly impact their properties and effectiveness (Perea-Lowery et al., 2021; Guimaraes et al., 2023; Wuersching et al., 2023). Conventional techniques and advanced digital technologies, such as CAD-CAM, offer different advantages and challenges in producing these appliances. Typically, occlusal splints have two types of surfaces: the unpolished surface (intaglio surface) located on the inner side wrapping the teeth and the polished surface (cameo surface) on the outer side contacting the opposing teeth (Crout, 2017). Polishing is the final step in splint finishing, performed after fabrication in the laboratory and following adjustments in clinical settings. It is a crucial factor influencing the properties of all splint materials, directly impacting clinical outcomes. Although the properties of acrylic resin fabricated using conventional and CAD-CAM techniques have been studied (Zeidan et al., 2022), the differences between unpolished and polished surfaces require further investigation. In particular, it is essential to examine how CAD-CAM splints respond to the same polishing protocol compared with conventional splints. A thorough understanding of these differences is crucial for optimizing fabrication techniques, establishing effective treatment protocols, and enhancing the performance and comfort of occlusal splints.
Hence, the aim of this study was to evaluate and compare the surface roughness and microhardness of the unpolished and polished surfaces of three occlusal splint materials: heat-cured, milled, and 3D-printed. The primary null hypothesis was that there would be no significant differences in surface roughness and microhardness among the three different occlusal splint materials. The secondary null hypothesis stated that there would be no significant differences in these properties between the unpolished and polished surfaces.
MATERIAL AND METHODS
Sample size
The surface roughness and microhardness tests were performed for occlusal splint materials fabricated by different techniques i.e., heat-curing, milling, and 3D-printing. The study determined the mean difference among three groups of independent specimens. The sample size was determined using G*Power software version 3.1.9.7, on the basis of the F test family and one-way ANOVA. According to Grymak et al. (2021), the mean microhardness of the polished occlusal splint materials was as follows: heat-cured at 0.290 ± 0.110 µm, milled at 0.070 ± 0.012 µm, and 3D-printed at 0.430 ± 0.170 µm. With 10 specimens per group, a power of 0.80, and a significance level of 0.05, the required sample size for this study was calculated to be 12 specimens per group for each test. Therefore, each test required 36 specimens, for a total of 72 specimens (Figure 1).
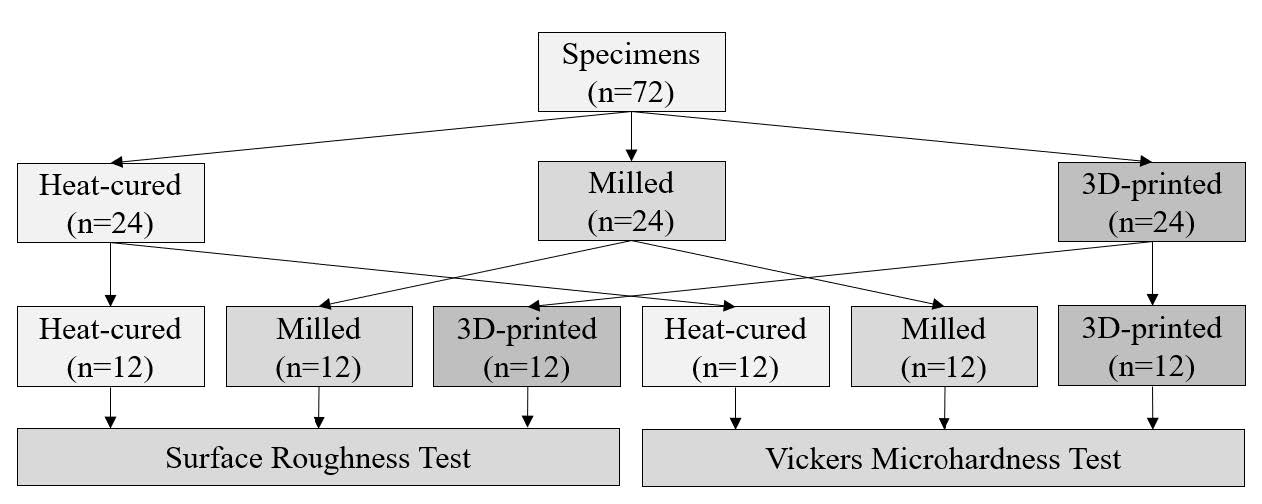
Figure 1. The study design involved 72 specimens for all tests. The first 36 specimens, comprising 12 each from heat-cured, milled, and 3D-printed occlusal splint materials, were tested for surface roughness. The remaining specimens were tested for Vickers microhardness.
Specimen preparation
The heat-cured specimens were created using 10×10×5 mm³ rectangular wax patterns placed in flasks. The wax was melted out and replaced with a mixture of clear acrylic resin powder and monomer (Meliodent-Heat Cure, Kulzer, Hanau, Germany) in a 35 g to 14 ml ratio (powder to liquid). The flasks were then placed in boiling water for 20 minutes to achieve complete polymerization, according to the manufacturer’s instructions (Figure 2A). For the milled specimens, CAD software was used to design 10×10×5 mm³ blocks. A clear PMMA block (Smile-Cam, Pressing Dental SRL, Dogana, San Marino Republic) was milled to these dimensions using a 5-axis milling machine (vnf S2, vhf camfacture AG, Germany) (Figure 2B). The 3D-printed specimens were created using CAD software to design the 10×10×5 mm³ dimensions and printed with clear resin (MED610-Biocompatible Clear, Stratasys, Minnesota, USA) on a 3D printer (Stratasys Objet260 Dental, USA). Standard manufacturer-recommended printing parameters, including a 0-degree orientation, high speed, high quality, and digital material printing mode, were used. Post-curing was performed with a UV light box (LC-3DPrint Box, NextDent, Vertex-Dental, Soesterberg, Netherlands) for 30 minutes (Figure 2C). One side of each specimen was polished using a stepwise process with 600-, 800-, and 1000-grit sandpaper, followed by wet pumice and tallow (Figure 2D). The other side was left untouched. After preparation, the specimens were stored in a dry container for 7 days before testing.
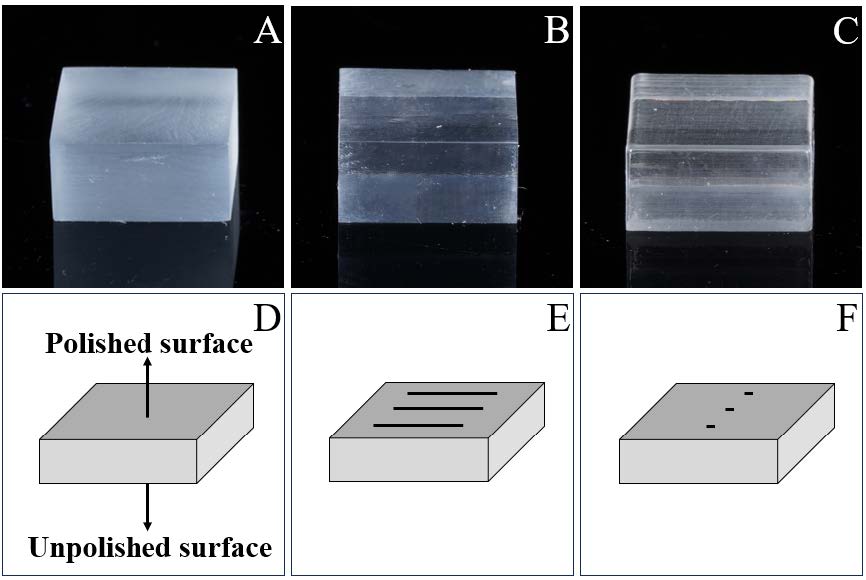
Figure 2. Specimen preparation and test protocols: A) Heat-cured specimen, B) Milled specimen, C) 3D-printed specimen, D) One side was polished (referred to as the polished surface) and the opposing side was left unpolished (referred to as the unpolished surface), E) Three 5-mm lines for a contact stylus in the surface roughness test, and F) Three points for pyramid indentation in the Vickers microhardness test.
Surface roughness and microhardness tests
Thirty-six specimens, i.e., 12 each from the heat-cured, milled, and 3D-printed groups, were measured for surface roughness using a contact surface roughness tester (Stylus for Contact, Talyscan 150, England). Each specimen was tested three times at random areas around the center, using a contact length of 5 mm per test (Figure 2E). The mean surface roughness value (Ra) was calculated for further analysis. Another set of thirty-six specimens was tested for their microhardness. Vickers microhardness was measured using a microhardness tester with a Vickers indenter (FM810, Future-Tech, Japan), which applied a load of 1.96 N for 15 seconds (Gibreel et al., 2021). The diagonals of the pyramid indentation on the specimen were measured optically by the testing machine's eyepiece operator, and the Vickers hardness number (HV) was calculated using the formula HV = 0.1891(F/d²), where F is the force in newtons and d is the mean length of the two diagonals in millimeters. Each specimen was measured three times in different areas (Figure 2F), and the mean value was used for further analysis. Additionally, one specimen from each group, totaling three specimens with six surfaces, was randomly selected and sputter-coated with a 99.99% gold layer using a sputter coater (Gold Coater, JFC-1200, Jeol, USA). This preparation allowed for the examination of the surface roughness morphology using scanning electron microscopy (SEM) (Quanta 250 FEG, FEI, USA), operating in high vacuum mode at 1000X magnification.
Data collection and analysis
To ensure consistent data collection, two examiners were assigned: one for the surface roughness test and another for the microhardness test, to measure and record all data for all specimens. Statistical analysis was performed using IBM SPSS Statistics for Windows, version 29.0 (IBM Corporation, Armonk, New York, USA). The Shapiro-Wilk test was used to assess data distribution. One-way ANOVA and the Kruskal-Wallis H test were used to compare the mean differences among the three groups, while the paired t-test and the Wilcoxon signed-rank test were used to compare the mean differences between the polished and unpolished specimens. A P-value of 0.05 was considered significant at the 95% confidence level.
RESULTS
Surface roughness analysis
Table 1 presents the mean surface roughness values for the occlusal splints. For the unpolished surfaces, there were significant differences in roughness among the three materials (P < 0.001). The 3D-printed occlusal splints had the lowest roughness, followed by the milled and heat-cured splints. The polished surfaces also showed significant differences (P < 0.001), with milled splints exhibiting the lowest roughness values. Figure 3A illustrates the roughness of the unpolished and polished surfaces, revealing that the heat-cured and milled splints had a significant reduction in roughness after polishing (P < 0.05). Conversely, the 3D-printed splints presented a significant increase in roughness after polishing (P < 0.05).
Table 1. The mean surface roughness values (µm) for the heat-cured, milled, and 3D-printed occlusal splints.
|
Surface Roughness [Ra (µm)] |
Heat-cured (n=12) |
Milled (n=12) |
3D-printed (n=12) |
P-value |
|
|
Unpolished surfaces |
Mean ± SD |
0.287 ± 0.041A |
0.090 ± 0.023B |
0.038 ± 0.002C |
<0.001* |
|
|
95% CI |
[0.261, 0.313] |
[0.076, 0.105] |
[0.036, 0.039] |
|
|
Polished surfaces |
Mean ± SD |
0.064 ± 0.016a |
0.046 ± 0.009b |
0.082 ± 0.019a |
<0.001** |
|
|
95% CI |
[0.054, 0.074] |
[0.040, 0.052] |
[0.070, 0.094] |
|
|
Note: *one-way ANOVA, **Kruskal-Wallis H test Different uppercase superscript letters denote significant differences (P < 0.05) from the post hoc Dunnett T3 test, while different lowercase letters indicate significant differences (P < 0.05) from the pairwise comparisons with Bonferroni correction. |
|||||
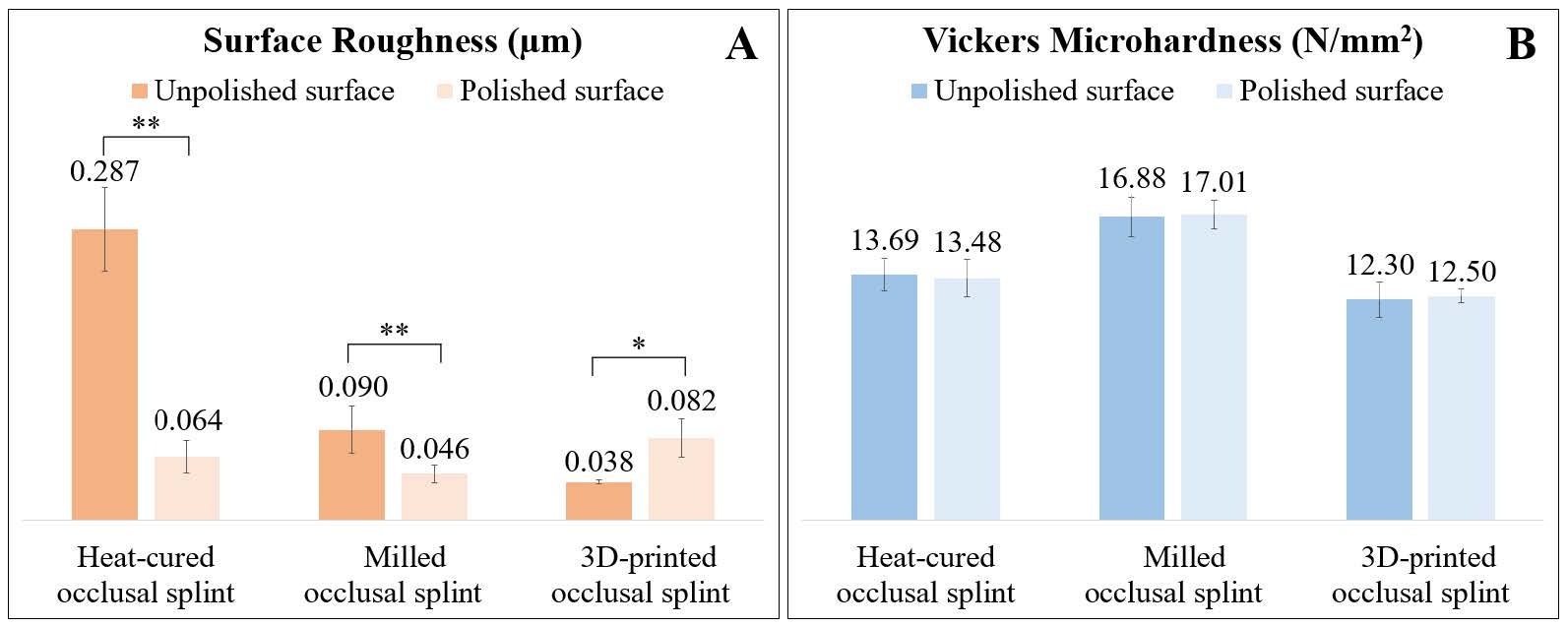
Figure 3. Comparisons of the unpolished and polished surfaces for the three occlusal splint materials: A) Surface roughness analysis with a single asterisk (*) indicates significant differences (P < 0.05) as determined by the paired t-test, while a double asterisk (**) denotes significant differences (P < 0.05) as determined by the Wilcoxon Signed Rank test. B) Vickers microhardness analysis indicated that there were no significant differences between the unpolished and polished surfaces.
The SEM images in Figure 4 demonstrate the surface morphology, illustrating the different changes in texture after polishing. The unpolished heat-cured surface (Figure 4A) exhibited rough and uneven features, while the unpolished milled surface (Figure 4B) was smoother with faint machining lines. The unpolished 3D-printed surface (Figure 4C) appeared smooth and homogeneous. Polishing improved all surfaces, with the heat-cured surface (Figure 4E) showing fewer irregularities, the milled surface (Figure 4F) achieving a fine texture, and the 3D-printed surface (Figure 4G) maintaining a smooth, consistent finish, with minimal surface imperfections.
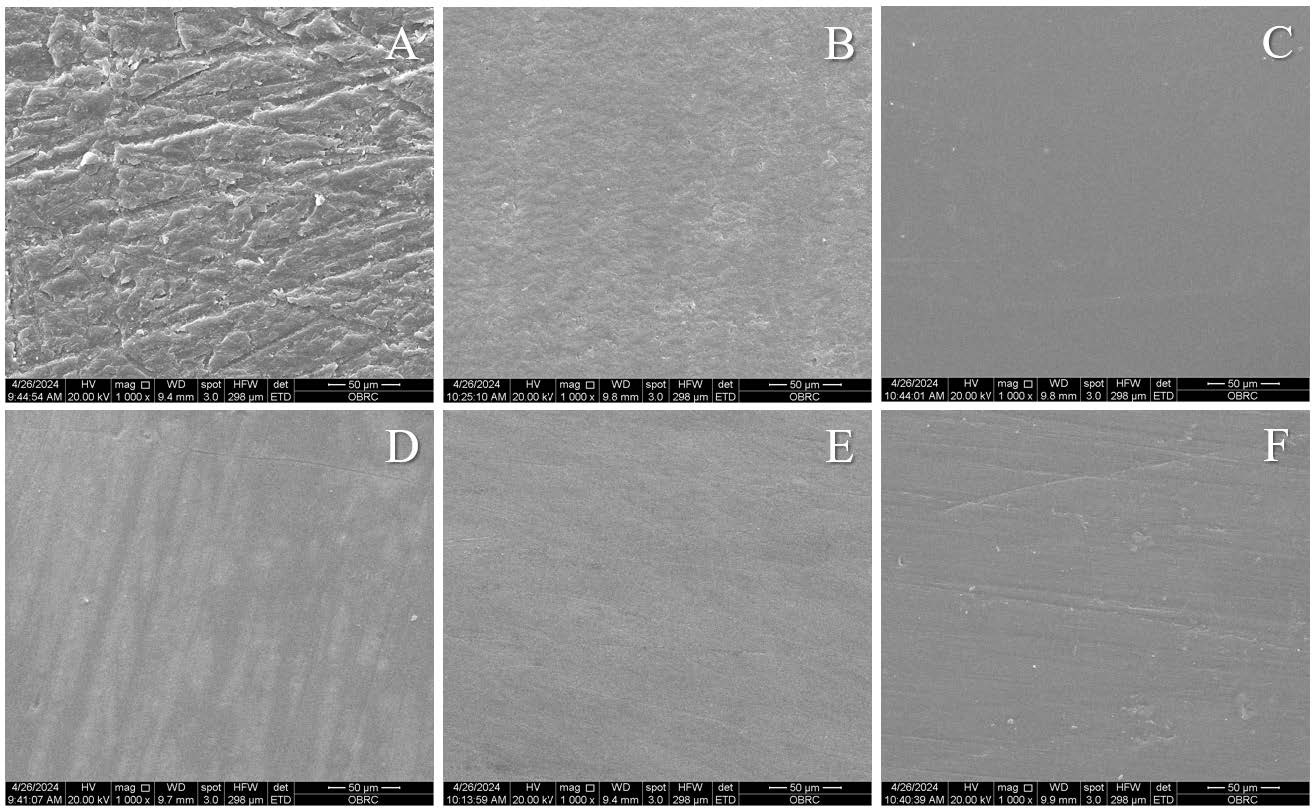
Figure 4. Representative SEM images at 1000X magnification: A-C) Unpolished surfaces of the heat-cured, milled, and 3D-printed occlusal splints, respectively, D-F) Polished surfaces of the heat-cured, milled, and 3D-printed occlusal splints, respectively.
Vickers microhardness analysis
Table 2 details the mean microhardness values for the heat-cured, milled, and 3D-printed occlusal splint materials, showing significant differences among the three materials for the unpolished and polished surfaces (P < 0.001). The milled occlusal splints exhibited the highest microhardness values, 16.88 ± 1.09 N/mm² for the unpolished surfaces and 17.01 ± 0.80 N/mm² for the polished surfaces, followed by the heat-cured splints and the 3D-printed splints. Comparing the unpolished and polished surfaces of each material, there were no significant differences in microhardness (P > 0.05) (Figure 3B). This indicates that the polishing process did not significantly alter the microhardness of the occlusal splint materials.
Table 2. The mean microhardness values (N/mm2) for the heat-cured, milled, and 3D-printed occlusal splints.
|
Vickers Microhardness [HV (N/mm2)] |
Heat-cured (n=12) |
Milled (n=12) |
3D-printed (n=12) |
P-value |
|
|
Unpolished surfaces |
Mean ± SD |
13.69 ± 0.90a |
16.88 ± 1.09b |
12.30 ± 0.98a |
<0.001** |
|
|
95% CI |
[13.12, 14.25] |
[16.19, 17.58] |
[11.68, 12.93] |
|
|
Polished surfaces |
Mean ± SD |
13.48 ± 1.03A |
17.01 ± 0.80B |
12.50 ± 0.36C |
<0.001* |
|
|
95% CI |
[12.83, 14.14] |
[16.50, 17.52] |
[12.27, 12.73] |
|
|
Note: * one-way ANOVA test, ** Kruskal-Wallis H test Different uppercase superscript letters denote statistical differences (P < 0.05) from the post hoc Tukey test, while different lowercase letters indicate statistical differences (P < 0.05) from pairwise comparisons with Bonferroni correction. |
|||||
DISCUSSION
The present study investigated the properties of three occlusal splint materials and found significant differences in their surface roughness and microhardness. Consequently, the primary null hypothesis, which stated there would be no significant differences in these properties among the three materials, was rejected. These findings align with previous studies, such as those by Berli et al. (2020), Gibreel et al. (2021), and Zeidan et al. (2022), which also reported significant variations in the mechanical properties of different occlusal splint materials. Additionally, the secondary null hypothesis, which stated that there would be no significant differences between unpolished and polished surfaces, was rejected for surface roughness but accepted for microhardness.
In terms of surface roughness, the heat-cured material exhibited the highest value of 0.287 µm on the unpolished surfaces, which was reduced to 0.064 µm after polishing. Similarly, the milled occlusal splints also had a decrease in roughness after polishing. These results suggest that the heat-cured and milled occlusal splints should be polished after fabrication to decrease roughness before being used by dental patients. Conversely, the 3D-printed materials had the lowest roughness of 0.038 µm on the unpolished surfaces. These findings suggest that 3D-printing technologies produce an occlusal splint with a smooth surface, aligning with research by Grymak et al. (2021) and Raffaini et al. (2023), who found that the 3D-printed occlusal splint surface had the lowest roughness compared with the other materials. Notably, after polishing, the 3D-printed materials showed an increase in roughness, unlike the heat-cured and milled materials, indicating that 3D-printed materials may not require polishing after fabrication (Grymak et al., 2021). However, Hickl et al. found that soft or flexible occlusal splints made by a 3D-printing machine had the highest roughness compared with heat-cured, milled, and hard 3D-printed materials (Hickl et al., 2022). Thus, the recommendation to avoid polishing may apply to hard 3D-printed splints, but not to soft splints.
The study of Grymak et al. demonstrated that surface roughness was affected by different printing angles (0°, 45°, and 90°), with three out of five 3D-printed splints showing the lowest roughness at a 0° printing angle, and two out of five splints showing the lowest roughness at 45° (Grymak et al., 2021). Similarly, this study utilized 3D-printed specimens oriented at 0°, with high speed and high-quality printing settings, which resulted in the lowest surface roughness on unpolished surfaces. Therefore, the printing angles influence the surface roughness of 3D-printed occlusal splints. Grymak et al. also observed that polishing with pumice reduced the surface roughness of unpolished surfaces with high and medium roughness levels, but increased the roughness of surfaces with initially low roughness levels (Grymak et al., 2021). These findings suggest that the initial surface roughness after fabrication was influenced by polishing. Similarly, in this study, the low surface roughness of unpolished 3D-printed splints increased after polishing. This could be attributed to the layer-by-layer printing technique at a 0° printing angle, which created a layered undulated microstructure (Nassif et al., 2023). This factor was influenced by polishing, which may be unparalleled and affect each layer differently, leading to alterations in the surface texture and exposing interlayers of the polished surfaces.
Moreover, surface roughness data can provide insights into the biofilm formation potential, which is important for selecting suitable materials for dental patients. Wuersching et al. found that greater roughness in occlusal splints led to increased microbial accumulation (Wuersching et al., 2023). In another study, Ozarslan et al. reported that surface roughness was not related to the adhesion amount of Candida albicans, as higher roughness did not result in greater adhesion (Ozarslan et al., 2024). Additionally, Schubert et al. stated that the adhesion of fungi (Candida albicans) or bacteria (Streptococcus mutans) varied in occlusal splints fabricated by different manufacturing methods (Schubert et al., 2021). Thus, these findings suggest that different occlusal materials have varying potential for microbial accumulation. However, the surface roughness threshold for bacterial colonization was reported to be 0.2 µm (Bollen et al., 1997), indicating that only unpolished surfaces of heat-cured splints have a higher potential for plaque accumulation compared to other materials.
For the microhardness analysis, the 3D-printed material showed the lowest hardness, ranging from 12.30–12.50 N/mm², indicating that it is less resistant to wear than milled and heat-cured materials. Similarly, Prpic et al. reported that 3D-printed occlusal splints had the lowest microhardness (4.88–11.29 N/mm²), compared with conventional and milled materials (Prpic et al., 2023). This is due to the composition of the materials used in printing technology, which must be printable and biocompatible, resulting in a lower microhardness compared with polymethyl methacrylate (PMMA) (de Paula Lopez et al., 2023). In contrast, the milled occlusal splints exhibited the highest hardness on the unpolished and polished surfaces, ranging from 16.88–17.01 N/mm², followed by the heat-cured materials. This suggests that milled occlusal splints, often made from controlled clear PMMA blanks before milling, are more resistant to scratches, wear, and occlusal load, indicating better long-term performance in clinical applications (Benli et al., 2023; Valenti et al., 2024). These findings align with those of Berli et al. (2020), Gibreel et al. (2022), and Zeidan et al. (2022), who found that milled materials maintained higher microhardness than other fabrication methods did.
Understanding the differences in splint properties is essential for optimizing the selection and fabrication of occlusal splints, ultimately leading to improved clinical outcomes for patients. Although this study focused on clear materials suitable for occlusal splints, similar findings have been reported in other studies, such as those on denture base materials, which also demonstrated comparable results among heat-cured, milled, and 3D-printed fabrication methods (Srinivasan et al., 2021; Zeidan et al., 2022; Fouda et al., 2023). By providing detailed insights into the material properties, this study contributes to the growing body of knowledge aimed at improving the effectiveness and durability of occlusal splints in dental practice. Dentists should consider factors related to individual patients, such as the severity of bruxism, the level of dentine exposure, and the rigidity of the opposing teeth contacting the occlusal splint. Additionally, the fabrication methods, including the appropriate polishing protocols for each material, are also critical considerations. These considerations can help dentists predict the long-term durability and wear resistance of the occlusal splint and the opposing teeth. Additionally, understanding the effects of bacterial accumulation on different materials will aid in managing and mitigating potential oral health issues when patients use their occlusal splints, as well as effective cleaning of acrylic surfaces (Siriyod et al., 2023).
The clinical significance and implication of this study lies in demonstrating that CAD-CAM occlusal splints exhibit low surface roughness after fabrication, with 3D-printed splints having the lowest roughness, eliminating the need for post-fabrication polishing. In contrast, heat-cured and milled splints still require polishing. During adjustments and polishing in clinical settings, milled splints achieve smoother surfaces more effectively than the others. Regarding microhardness, the ranking was milled > heat-cured > 3D-printed splints, with polishing having no significant impact on this property. Microhardness should be considered when selecting occlusal splints for individual patients based on their specific oral conditions.
This study had several limitations. First, the study focused on specific material types, excluding others, which means that the results may not be applicable to different materials. Second, potential variability in operator techniques during specimen preparation and testing should be taken into account. These results, based on in vitro conditions that differ from real-life settings, should be interpreted with caution. Additionally, the surface roughness test was standardized with a uniform polishing protocol, which may not reflect the variety of polishing techniques used by clinicians in practice. Therefore, the roughness obtained in clinical settings might differ from the study’s findings. Additionally, although the microhardness test was utilized to assess the durability of occlusal splints, it does not directly measure wear resistance. In clinical scenarios, occlusal splints and opposing teeth experience static and dynamic forces, which the study’s results may not fully capture. Furthermore, the laboratory conditions may not accurately replicate the complex oral environment, where factors, such as saliva, temperature fluctuations, and mechanical forces, markedly impact material properties. Future research should focus on studying occlusal splints under conditions that more closely simulate long-term use in the patient’s mouth.
CONCLUSION
Within the limitations of this study, significant differences in surface roughness and microhardness were observed among heat-cured, milled, and 3D-printed occlusal splint materials. The 3D-printed splints had the smoothest unpolished surfaces, while the milled splints had the smoothest polished surfaces and the highest microhardness. Polishing had varying effects on surface roughness, reducing it in heat-cured and milled materials but increasing it in 3D-printed splints. However, microhardness remained unaffected by polishing across all materials.
ACKNOWLEDGEMENTS
The authors sincerely thank Dr. Kevin Tompkins for his thorough review and English editing of the manuscript. We also deeply appreciate the essential support from the Dental Materials Research and Development Center and the Oral Biology Research Center at the Faculty of Dentistry, Chulalongkorn University.
AUTHOR CONTRIBUTIONS
UU conceived the ideas and conceptualization. UU, JC, TI, and TT reviewed the relevant literature. UU designed the study. UU, JC, TI, and TT conducted experiments and collected the data. UU performed the initial screening, statistical analysis, and critical interpretation of the data, and wrote the manuscript draft. JC, TI, and TT provided suggestions for the manuscript draft. UU, JC, TI, and TT revised and approved the final manuscript.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
REFERENCES
Ahmed, M.M.S., Shi, D., Al-Somairi, M.A.A., Alhashimi, N., Almashraqi, A.A., Musa, M., Li, N., Chen, X., and Alhammadi, M.S. 2023. Three dimensional evaluation of the skeletal and temporomandibular joint changes following stabilization splint therapy in patients with temporomandibular joint disorders and mandibular deviation: A retrospective study. BMC Oral Health. 23(1): 18.
Albagieh, H., Alomran, I., Binakresh, A., Alhatarisha, N., Almeteb, M., Khalaf, Y., Alqublan, A., and Alqahatany, M. 2023. Occlusal splints-types and effectiveness in temporomandibular disorder management. Saudi Dental Journal. 35(1): 70-79.
American College of Prosthodontists and ACP Education Foundation. 2021. Glossary of digital dental terms, 2nd edition. Journal of Prosthodontics. 30(Supplement 3): 172-181.
Benli, M., Al-Haj Husain, N., and Ozcan, M. 2023. Mechanical and chemical characterization of contemporary occlusal splint materials fabricated with different methods: A systematic review. Clinical Oral Investigations. 27(12): 7115-7141.
Berli, C., Thieringer, F.M., Sharma, N., Muller, J.A., Dedem, P., Fischer, J., and Rohr, N. 2020. Comparing the mechanical properties of pressed, milled, and 3D-printed resins for occlusal devices. Journal of Prosthetic Dentistry. 124(6): 780-786.
Blasi, A., Henarejos-Domingo, V., Palacios-Banuelos, R., Aparicio, C., and Roig, M. 2023. Comparison accuracy of digital and analog method using milled occlusal splints. Journal of Esthetic and Restorative Dentistry. 35(7): 1103-1112.
Blasi, A., Henarejos-Domingo, V., Palacios-Banuelos, R., Vidal-Ponsoda, C., Aparicio, C., and Roig, M. 2023. CAD-CAM and analog occlusal splints comparison based on the amount of occlusal adjustments. 3D analysis of the volumetric changes: A pilot study. Journal of Esthetic and Restorative Dentistry. 35(8): 1271-1278.
Bollen, C.M., Lambrechts, P., and Quirynen, M. 1997. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dental Materials. 13(4): 258-269.
Crout, D.K. 2017. Anatomy of an occlusal splint. General Dentistry. 65(2): 52-59.
de Paula Lopez, V., Dias Corpa Tardelli, J., Botelho, A.L., Marcondes Agnelli, J.A., and Candido Dos Reis, A. 2023. Mechanical performance of 3-dimensionally printed resins compared with conventional and milled resins for the manufacture of occlusal devices: A systematic review. Journal of Prosthetic Dentistry. 132(6): 1262-1269.
Ding, W.H., Li, Y. F., Liu, W., Li, W., Wu, N., Hu, S.Y., and Shi, J.J. 2024. Effect of occlusal stabilisation splint with or without arthroscopic disc repositioning on condylar bone remodelling in adolescent patients. International Journal of Oral and Maxillofacial Surgery. 53(2): 156-164.
Fouda, S.M., Gad, M.M., Abualsaud, R., Ellakany, P., AlRumaih, H.S., Khan, S.Q., Akhtar, S., Al-Qarni, F.D., and Al-Harbi, F.A. 2023. Flexural properties and hardness of CAD-CAM denture base materials. Journal of Prosthodontics. 32(4): 318-324.
Gibreel, M., Perea-Lowery, L., Vallittu, P.K., Garoushi, S., and Lassila, L. 2022. Two-body wear and surface hardness of occlusal splint materials. Dental Materials Journal. 41(6): 916-922.
Gibreel, M., Perea-Lowery, L., Vallittu, P.K., and Lassila, L. 2021. Characterization of occlusal splint materials: CAD-CAM versus conventional resins. Journal of the Mechanical Behavior of Biomedical Materials. 124: 104813.
Grymak, A., Aarts, J.M., Ma, S., Waddell, J.N., and Choi, J. J.E. 2021. Comparison of hardness and polishability of various occlusal splint materials. Journal of the Mechanical Behavior of Biomedical Materials. 115: 104270.
Guimaraes, D.M., Campaner, M., Santos, R.W.D., Pesqueira, A.A., and Medeiros, R.A. 2023. Evaluation of the mechanical properties of different materials for manufacturing occlusal splints. Brazilian Oral Research. 37: e034.
Hardy, R.S. and Bonsor, S.J. 2021. The efficacy of occlusal splints in the treatment of bruxism: A systematic review. Journal of Dentistry. 108: 103621.
Hickl, V., Strasser, T., Schmid, A., and Rosentritt, M. 2022. Effects of storage and toothbrush simulation on color, gloss, and roughness of CAD/CAM, hand-cast, thermoforming, and 3D-printed splint materials. Clinical Oral Investigations. 26(5): 4183-4194.
Kolcakoglu, K., Dogan, S., Tulga Oz, F., and Aydinbelge, M. 2022. A comparison of hard and soft occlusal splints for the treatment of nocturnal bruxism in children using the Bitestrip®. Journal of Clinical Pediatric Dentistry. 46(3): 219-224.
Layton, D.M., Morgano, S.M., Muller, F., Kelly, J.A., Nguyen, C.T., Scherrer, S.S., Salinas, T.J., Shah, K.C., Att, W., Freilich, M.A., and Ferro, K.J. 2023. The glossary of prosthodontic terms 2023: Tenth Edition. Journal of Prosthetic Dentistry. 130(4): e1-e126.
Minervini, G., D'Amico, C., Cicciu, M., and Fiorillo, L. 2023. Temporomandibular joint disk displacement: Etiology, diagnosis, imaging, and therapeutic approaches. Journal of Craniofacial Surgery. 34(3): 1115-1121.
Nassif, M., Haddad, C., Habli, L., and Zoghby, A. 2023. Materials and manufacturing techniques for occlusal splints: A literature review. Journal of Oral Rehabilitation. 50(11): 1348-1354.
Orgev, A., Levon, J.A., Chu, T. G., Morton, D., and Lin, W.S. 2023. The effects of manufacturing technologies on the surface accuracy of CAD-CAM occlusal splints. Journal of Prosthodontics. 32(8): 697-705.
Orzeszek, S., Waliszewska-Prosol, M., Ettlin, D., Seweryn, P., Straburzynski, M., Martelletti, P., Jenca, A., Jr., and Wieckiewicz, M. 2023. Efficiency of occlusal splint therapy on orofacial muscle pain reduction: A systematic review. BMC Oral Health. 23(1): 180.
Ozarslan, M., Avcioglu, N.H., Bilgili Can, D., and Caliskan, A. 2024. Biofilm formation of C. albicans on occlusal device materials and antibiofilm effects of chitosan and eugenol. Journal of Prosthetic Dentistry. 131(1): 144.e1-144.e9.
Perea-Lowery, L., Gibreel, M., Vallittu, P.K., and Lassila, L. 2021. Evaluation of the mechanical properties and degree of conversion of 3D printed splint material. Journal of the Mechanical Behavior of Biomedical Materials. 115: 104254.
Prpic, V., Spehar, F., Stajdohar, D., Bjelica, R., Cimic, S., and Par, M. 2023. Mechanical properties of 3D-printed occlusal splint materials. Dentistry Journal (Basel). 11(8): 199.
Raffaini, J.C., Soares, E.J., Oliveira, R.F.L., Vivanco, R.G., Amorim, A.A., Pereira, A. L.C., and Pires-de-Souza, F.C.P. 2023. Effect of artificial aging on mechanical and physical properties of CAD-CAM PMMA resins for occlusal splints. Journal of Advanced Prosthodontics. 15(5): 227-237.
Rongo, R., Michelotti, A., Pedersen, T.K., Resnick, C.M., and Stoustrup, P. 2023. Management of temporomandibular joint arthritis in children and adolescents: An introduction for orthodontists. Orthodontics & Craniofacial Research. 26(Supplement 1): 151-163.
Schubert, A., Burgers, R., Baum, F., Kurbad, O., and Wassmann, T. 2021. Influence of the manufacturing method on the adhesion of Candida albicans and Streptococcus mutans to oral splint resins. Polymers (Basel). 13(10): 1534.
Siriyod, W., Wanachantararak, P., Sastraruji, T., Chaijareenont, P., Chaiyana, W., Sookkhee, S., and Owittayakul, D. 2023. Novel denture cleanser formulated from virgin coconut oil and the anionic emulsifier against Candida albicans biofilms formed on 96-wells plate and acrylic resin surfaces. Natural and Life Sciences Communications. 22(3): e2023047.
Srinivasan, M., Kalberer, N., Kamnoedboon, P., Mekki, M., Durual, S., Ozcan, M., and Muller, F. 2021. CAD-CAM complete denture resins An evaluation of biocompatibility, mechanical properties, and surface characteristics. Journal of Dentistry. 114: 103785.
Uma, U., Fongpisuttikul, P., Padungpipatbawon, P., and Luyapan, P. 2024. Prevalence, awareness, and management of bruxism in Thai dental students: A cross-sectional study. Cranio: The Journal of Craniomandibular & Sleep Practice. 42(5): 532-538.
Valenti, C., Federici, M.I., Coniglio, M., Betti, P., Pancrazi, G.P., Tulli, O., Masciotti, F., Nanussi, A., and Pagano, S. 2024. Mechanical and biological properties of polymer materials for oral appliances produced with additive 3D printing and subtractive CAD-CAM techniques compared to conventional methods: A systematic review and meta-analysis. Clinical Oral Investigations. 28(7): 396.
Wuersching, S.N., Westphal, D., Stawarczyk, B., Edelhoff, D., and Kollmuss, M. 2023. Surface properties and initial bacterial biofilm growth on 3D-printed oral appliances: A comparative in vitro study. Clinical Oral Investigations. 27(6): 2667-2677.
Zafar, M.S. 2020. Prosthodontic applications of polymethyl methacrylate (PMMA): An update. Polymers (Basel). 12(10): 2299.
Zeidan, A.A.E., Abd Elrahim, R.A., Abd El Hakim, A.F., Harby, N.M., and Helal, M.A. 2022. Evaluation of surface properties and elastic modulus of CAD-CAM milled, 3D printed, and compression moulded denture base resins: An in vitro study. Journal of International Society of Preventive and Community Dentistry. 12(6): 630-637.
OPEN access freely available online
Natural and Life Sciences Communications
Chiang Mai University, Thailand. https://cmuj.cmu.ac.th
Uthai Uma1, *, Jirayu Chansri2, Thitiphat Itthipornpaisan2, and Trin Thahong2
1 Department of Occlusion, Faculty of Dentistry, Chulalongkorn University, Bangkok 10330, Thailand.
2 Faculty of Dentistry, Chulalongkorn University, Bangkok 10330, Thailand
Corresponding author: Uthai Uma, E-mail: Uthai.U@chula.ac.th
ORCID ID: Uthai Uma: https://orcid.org/0000-0003-1949-9465
Total Article Views
Editor: Anak Iamaroon,
Chiang Mai University, Thailand
Article history:
Received: January 27, 2025;
Revised: March 22, 2025;
Accepted: April 8, 2025;
Online First: April 29, 2025

