
Influence of Calcium Silicate-Based vs. Resin-Based Sealers on Pull-Out Bond Strength of Two Universal Adhesive/Resin Cement Combinations for Fiber Posts Cementation
Pimpinee Eamsa-ard, Prattana Yodmanotham *, Jidapa Saelee, Pimsiri Awsakulsutthi, Poolvalee Poolsawat, and Yotyothin KetiphanPublished Date : January 15, 2025
DOI : https://doi.org/10.12982/NLSC.2025.019
Journal Issues : Number 2, April-June 2025
Abstract This in vitro study investigated the influence of root canal sealer type (calcium silicate-based vs. resin-based) on the pull-out bond strength of two universal adhesive/resin cement combinations. Forty-eight human premolars were prepared, obturated with either Ceraseal™ (calcium-silicate based) (C) or AH Plus™ (resin-based) (A), and stored at 37°C, 100% humidity for 24 hours. Two adhesive/resin cement combinations were used for fiber post cementation: Single Bond Universal/RelyX™ Ultimate (UT) and ScotchbondTM Universal Plus/RelyX™ Universal (UN). Pull-out bond strength values (Newton) were measured after seven days using a universal testing machine. Then all fiber posts were observed for mode of failure using a stereomicroscope. AH PlusTM and ScotchbondTM Universal Plus/RelyXTM Universal (AUN) had the highest bond strength (263.50 ± 46.47 N), while CeraSealTM and Single Bond Universal Adhesive/RelyXTM Ultimate (CUT) had the lowest (202.88± 38.21 N). The results of the two-way ANOVA indicated a significant main effect for root canal sealer types (P = 0.025); a significant main effect for resin cement types (P = 0.015); and no significant interaction effect between root canal sealer types and resin cement types (P = 0.068). Post hoc Tukey HSD testing revealed significant differences between CUT and CUN (p = 0.008), CUT and AUN (P = 0.003), and CUT and AUT (P = 0.024). The most common failure mode was the mixed type. The type of root canal sealer and the combination of adhesive/resin cements influence pull-out bond strength values. Using the calcium-silicated base sealer may decrease the pull-out bond strength values in certain adhesive/resin cement combinations.
Keywords: Resin-based sealer, Calcium silicate-based sealer, Fiberglass pins, Dual-cured resin cement, Pull-out bond strength test, Universal adhesive system.
Funding:The authors are grateful for the research funding provided by the Rangsit University, Pathum Thani, Thailand.
Citation: Eamsa-ard, P., Yodmanotham, P., Saelee, J., Awsakulsutthi, P., Poolsawat, P., and Ketiphan, Y. 2025. Influence of calcium silicate-based vs. resin-based sealers on pull-out bond strength of two universal adhesive/resin cement combinations for fiber posts cementation. Natural and Life Sciences Communications. 24(2): e2025019.
INTRODUCTION
The longevity of endodontically treated teeth depends on both root canal success and the quality of tooth restoration (Dammaschke et al., 2003). The success of endodontic treatment relies on many factors, effective microbial eradication from mechanical instrumentation technique or irrigation and hermetic seal from post endodontically treated restoration (Sjögren et al., 1990; Khongkhunthian and Tanmukayakul, 2007). Fiber posts are mostly used in the restoration of endodontically treated tooth due to provide maximum retention along with stress distribution inside the root canal (Prisco et al., 2003). While various factors contribute to the clinical failure of fiber post cementation, loss of adhesion at the dentin-adhesive/resin cement interface stands out as a major role leading to post-debonding (Theodosopoulou and Chochlidakis, 2009). The bond strength of fiber post can be impacted by the choice of root canal sealer (Forough Reyhani et al., 2016; Nesello et al., 2022). Studies have shown that sealers containing eugenol, a common component, can negatively influence the retention of the fiber post within the root canal (Cecchin et al., 2011; Nica et al., 2013; Graiff et al., 2014). Fortunately, unlike eugenol-containing sealers, resin-based sealers appear to have no negative impact on the retention of fiber posts (Cecchin et al., 2011).
The calcium silicate-based sealer is used extensively because of its bioactive characteristics, which set it apart from other root canal sealers (Santos et al., 2017; Eskandari et al., 2022). Significantly, it demonstrates resilience to moisture and experiences less expansion upon setting, hence improving the effectiveness of sealing in comparison to traditional endodontic sealers (Lim et al. 2020). Some studies have indicated that calcium silicate-based sealers might lead to a weaker bond between the fiber post and dentin compared to resin-based sealers (Vilas-Boas et al., 2018; Nesello et al., 2022).
The development of adhesive system aimed to overcome the limitations of traditional self-etch adhesives. Unlike self-etch adhesives limited to dentin bonding, universal adhesives offered adhesion to a wider range of substrates, including fiber posts (Radovic et al., 2008; Perdigao et al., 2021). This broader applicability enhanced the effectiveness of self-adhesive cements.
RelyX™ Ultimate (3M, ESPE) and RelyX™ Universal (3M, ESPE) were introduced to optimize performance specifically with universal adhesives (Kim et al., 2020). Notably, RelyX™ Ultimate and Single Bond Universal Adhesive (3M, ESPE), introduced in the early 2010s, achieved superior bond strength due to the favorable bonding properties of the universal adhesive component (Kansal et al., 2018). Years later, RelyX™ Universal and Scotchbond™ Universal Plus were developed to address the instability of silane in the earlier universal adhesive system. This new formulation demonstrably improved bond strength by incorporating optimized silane mixtures (Yao et al., 2021).
While advancements have been made in both calcium silicate-based sealers and self-adhesive resin cement combined with universal adhesives, a gap exists in the research regarding the interplay between these factors (Vilas-Boas et al., 2018; Nesello et al., 2022). Therefore, this study aims to investigate the influence of root canal sealer type (calcium silicate-based vs. resin-based) on the pull-out bond strength of two specific universal adhesive/resin cement combinations: Single Bond Universal/RelyX™ Ultimate and Scotchbond™ Universal Plus/RelyX™ Universal. The null hypothesis (H₀) of this study is that neither the type of root canal sealer, the type of universal adhesive used with resin cement, nor the interaction between these factors will affect the pull-out bond strength values of fiber posts cemented into the root canal.
MATERIAL AND METHODS
This study has been approved by the Ethics Committee of Rangsit University (protocol No.RSUERB2022-075). The specimens were obtained from forty-eight extracted human permanent mandibular first premolars, each having a straight single root canal and complete root formation. These teeth were preserved in a 0.1% Thymol solution and utilized within a six-month timeframe. The exclusion criteria included teeth with dental caries, visible cracks or fractures, prior root canal treatment, open apices, calcified root canals, and teeth exhibiting internal or external root resorption.
Sample size calculation
The sample size of this study was calculated using the program G*Power 3.1 (Faul et al., 2007); The total sample was forty-eight teeth, with twelve specimens per group. By using the fixed effects, special, main effects, and interactions of the ANOVA formula, with an effect size (f) = 0.4, β/α ratio = 1, numerator df = 1, and number of groups = 4, a power of test = 0.88 was obtained. Consequently, studies in the same field were reviewed and showed a sample size of 10-12 specimens per group (Macedo et al., 2009; Alsubait, 2021).
Root canal treatment procedures
All specimens were sectioned at the coronal portion to achieve a standardized root length of 12 mm using an IsoMet slow-speed cutting machine (Buehler, Lake Bluff, Illinois, USA) equipped with a water coolant system. Root canal preparation was performed using Mtwo™ NiTi rotary files (VDW, Munich, Germany), progressing up to file size 30/05. The working length (WL) was set at 11.5 mm, which is 0.5 mm shorter than the total root length. The rotary file system was operated at the RPM and torque settings specified by the manufacturer. After each change in file size, the root canal was irrigated with 1 mL of 2.5% sodium hypochlorite using K-file no. 10 to maintain patency. Subsequently, the main cone (VDW, Munich, Germany) number 30/04 was inserted and checked for slight resistance upon gentle withdrawal (tug-back) to ensure proper fit. Radiography was then performed to confirm the position of the main cone at the working length. For the final flush, 2 mL of 2.5% sodium hypochlorite (M dentTM, Thailand) and 2 mL of 17% EDTA solution (Endo Clean, M dentTM, Thailand) were used within 1 minute, followed by 2 mL of distilled water. The specimens were then divided into two groups: calcium silicate-based (Ceraseal™, Meta Biomed Co., Cheongju, Korea) which was obturated using the single cone technique, and resin-based sealer (AH Plus™, Dentsply, Germany) which was obturated using warm vertical compaction.
After the root canals were filled, all specimens were temporarily restored using Cavit™ (3M, ESPE) with a thickness of 4 mm. They were then stored in an incubator at 100% humidity and 37°C for 24 hours to ensure the complete setting of both sealers. Next, the post space was prepared using a number 2 D.T. Light-post drill (VDW, Munich, Germany). The drilling depth was set at 7.5 mm. from the reference point, leaving 4 mm of gutta-percha as the apical seal (Figure 1.) The resin cement was mixed according to the manufacturer's instructions and then delivered into the root canal space using a Centrix syringe tip to prevent void formation during post-cementation. Figure 2 illustrates the specimen preparation and allocation process.
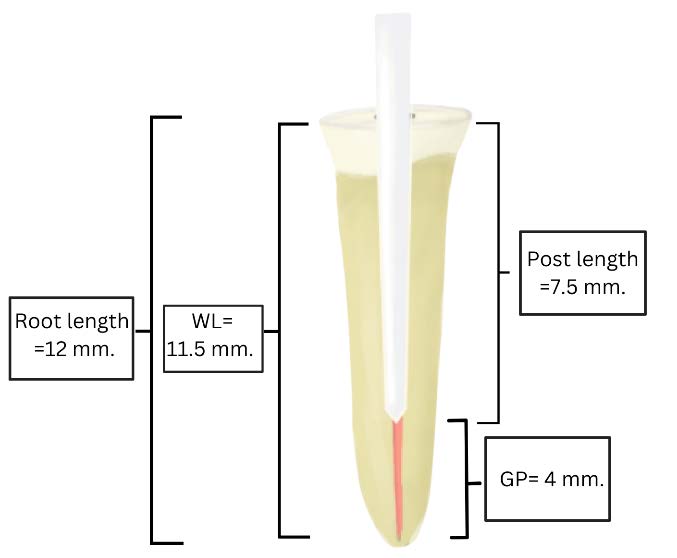
Figure 1. The specimen preparation follows the post-fixation process. Measurements include: Root length = 12 mm, WL (Working length) = 11.5 mm, GP (Gutta-percha) = 4 mm, and Post length = 7.5 mm.
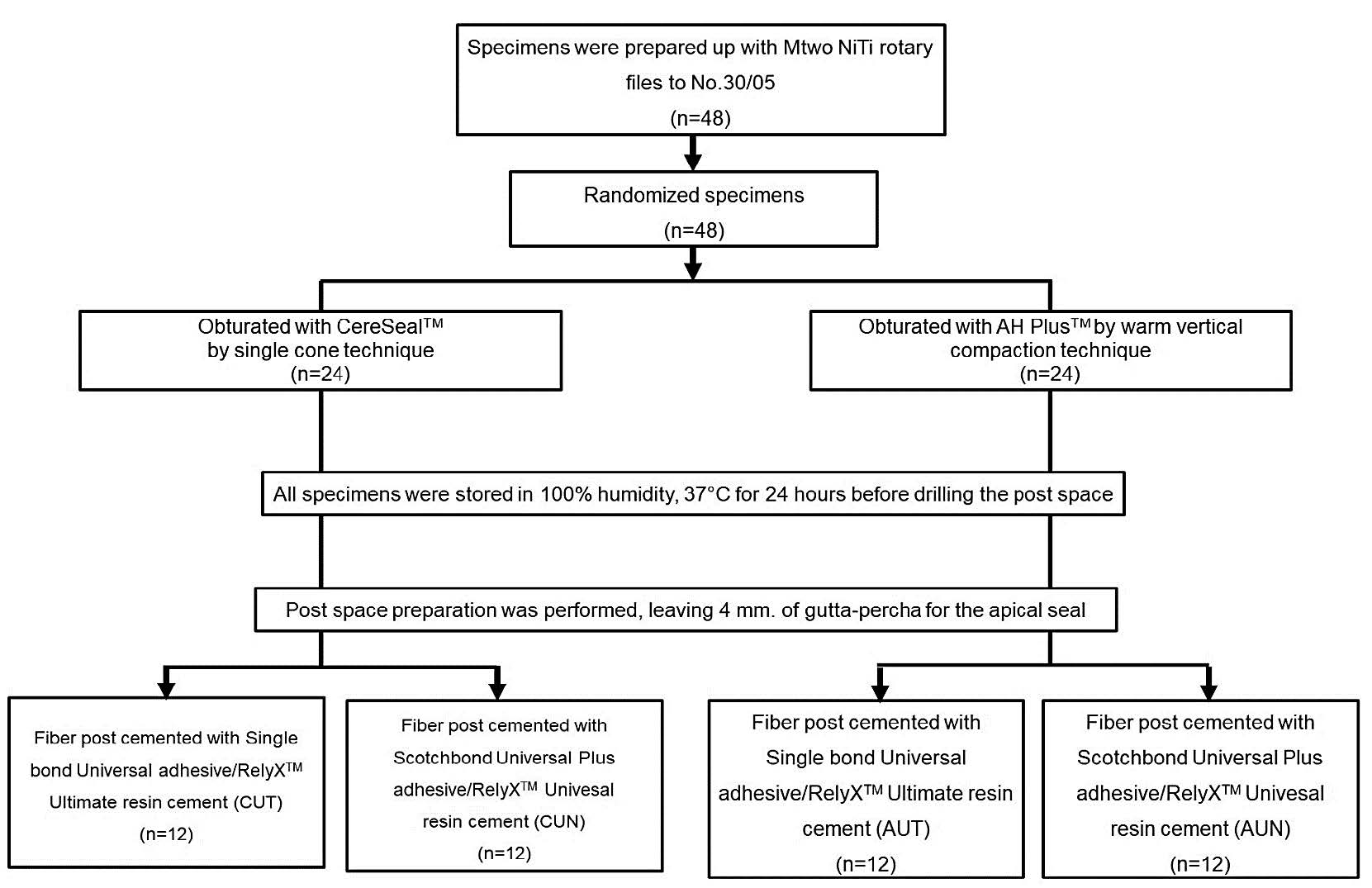
Figure 2. Specimens preparation and allocation process.
Fiber post cementation procedures
The DT-light post (RTD Illusion, France) was cemented using two different adhesive/resin cement combinations. Consequently, there were four experimental groups according to the type of root canal sealer and adhesive/resin cement combinations:
CUT: Ceraseal™ (C)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT)
CUN: Ceraseal™ (C)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN)
AUT: AH Plus™ (A)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT)
AUN: AH Plus™ (A)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN)
Table 1 details the materials, their compositions, and the corresponding application protocols. Table 2 outlines each group's post-surface treatment, post-space treatment, and fiber post cementation procedures. After the cementation process, all specimens were maintained at 37°C in 100% humidity for 7 days.
Table 1. List of materials includes brands and chemical formulations.
|
Materails |
Composition |
Batch Number |
|
CeraSeal™ (Meta Biomed Co., Cheongju, Korea) |
Premixed: calcium silicates, zirconium oxide, thickening agent |
12204011 |
|
AH Plus™ (Dentsply/Maillefer, Konstanz, Germany) |
Paste A (Epoxy): diglycidil-bisphenol-A-et her, calcium, tungsten, zirconium oxide, aerosol, Iron, oxide. Paste B (Amina): Amina 1-adamantane, N, Ndibenzyl-5-oxanonandiamine-1, 9, TCD-diamine, calcium tungsten, zirconium oxide, silicone oxide. |
2203000659 |
|
Single Bond Universal Adhesive |
MDP Phosphate Monomer, Dimethacrylate resins, HEMA VitrebondTM copolymer, filer, ethanol, water, Iitlators silane |
7879383 |
|
RelyX™ Ultimate (3M ESPE, St. Paul, USA) |
Base Paste: Methacrylate monomers, radiopaque, silanated fillers, initiator components, stabilizers, theological additives Catalyst Paste: Methacrylate monomers, radiopaque alkaline (basic) fillers, initiator components, stabilizers, pigments, theological additives, fluorescence dye, dark cure activator for Schotchbond Universal adhesive |
8879166 |
|
Scotchbond™ Universal Plus Adhesive |
BPA derivative free dimethacrylate monomers including a novel radiopaque monomer. MDP phosphate monomer, HEMA hydrophilic monomer for wetting dentin, 3M Vitrebond copolymer - 3M proprietary technology for moisture tolerance, non-settling silica filler for adjusting viscosity and handling, ethanol, water, photoinitiator system, optimized mixture of silanes for high bond to glass ceramics, dual-cure accelerator |
8991632 |
|
RelyXTM Universal (3M ESPE, St. Paul, USA) |
BPA derivative-free dimethacrylate monomers, phosphorylated dimethacrylate adhesion monomers, photoinitiator system, novel amphiphilic redox initiator system, radiopaque fillers, and theologica, additives, pigments |
8587579 |
Table 2. Post-surface treatment, post-space treatment, and fiber post-cementation were used in each group.
|
Group |
Post surface treatment |
Post space treatment |
Post cementation |
||
|
CUT |
Post surface treatment (D.T. LIGHT-POST®, RTD) 1. Surface treatment with 35% Hydrogen peroxide for 5 minutes 2. Wash and air-dry 3. Silane with Monobond N 4. Wait 1 minute and air dry with a triple syringe until there is no movement of fluid on the post surface |
Apply Single Bond Universal Adhesive with Microbrush X into the cavity with the agitating motion for 20 seconds. |
The specimens were dried using paper points and a triple syringe with a gentle airblow |
The resin cement was mixed according to the manufacturer's directions and injected into the root canal using a Centrix syringe tip to avoid voids. A fiber post was inserted by applying gentle pressure to ensure the proper positioning of the post. |
Light cure for 20 seconds with LED light curing unit |
|
AUT
|
|||||
|
CUN |
Apply Scotchbond™ Universal Plus Adhesive with Microbrush X into the cavity with the agitating motion for 20 seconds. |
||||
|
AUN |
|||||
|
Remark: CUT: Ceraseal™ (C)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT) CUN: Ceraseal™ (C)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN) AUT: AH Plus™ (A)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT) AUN: AH Plus™ (A)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN) |
|||||
Pull-out bond strength measurement
The pull-out bond strength value (in Newton) was measured using a Universal Testing Machine (Instron 5566) with a pull-up direction at a cross-head speed of 1 mm/minute. Figure 3 illustrates the pull-out bond strength test setup, using a newly designed key drill chuck (Figure 3B) combined with a novel metal plate (Figure 3A). The fiber post is inserted through the plate, with the chuck securely gripping it from above. This innovative design eliminates the need to embed specimens in resin molds and allows for securely and stably gripping small-sized fiber posts, thereby enhancing precision and reliability during testing.
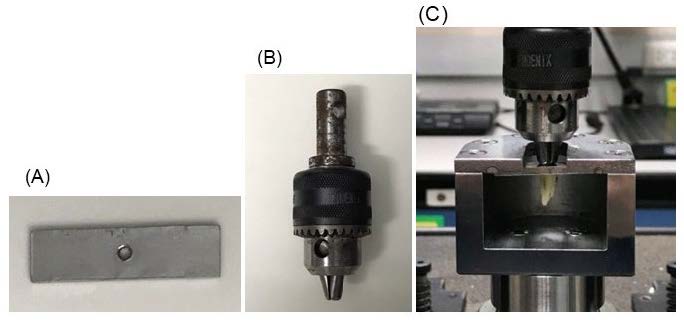
Figure 3. Illustrates the setup for the pull-out bond strength test. A) Metal plate designed to hold the post in the correct position. B) A newly designed key drill chuck fiber post holder attached to a universal testing machine. C) The specimen was fixed in the holder and plate and prepared for pull-out testing.
Mode of failure analysis
The dislodged posts were analyzed using a stereomicroscope (Olympus, Tokyo, Japan) at a magnification of 20x to evaluate the types of failures into three categories: 1) adhesive failures occurring at the post/resin cement interface with no resin cement visible around the post, 2) cohesive failures within the resin cement, and 3) mixed failures with resin cement covering 75% the post surface.
Statistical analysis
Statistical analysis was using the SPSS Statistics program version 26.0 for Windows (IBM Corp. 2019). The normality of the data for each group was assessed using the Shapiro-Wilk test. The homogeneity of variance was assessed using Levene's test. A two-way analysis of variance (ANOVA) was performed to determine the effects of the factors (root canal sealer type and adhesive/resin cement combinations) and their interaction on the pull-out bond strength values (α = 0.05). Post hoc testing using Tukey HSD was conducted for multiple comparisons when significant main or interaction effects were identified.
RESULTS
The mean pull-out bond strength values and standard deviations for root canal sealer types and resin cement types are presented in Table 3 and Figure 4. Group AH Plus™ & Scotchbond™ Universal Plus/RelyX™ Universal (AUN) revealed the highest pull-out bond strength values (263.50 ± 46.47 N), while Group CeraSeal™ & Single Bond Universal Adhesive/RelyX™ Ultimate (CUT) revealed the lowest pull-out bond strength (202.88 ± 38.21 N). The results of the two-way ANOVA indicated a significant main effect for root canal sealer types, F(1, 44) = 5.37, P = 0.025; a significant main effect for resin cement types, F(1, 44) = 6.35, P = 0.015; and no significant interaction effect between root canal sealer types and resin cement types, F(1, 44) = 3.50, P = 0.068.
Table 3. Descriptive statistics for pull-out bond strength values (N) according to Root canal sealer types and Adhesive /Resin cement combination types.
|
Sealer types |
Cement types (n=12) |
Pull-out bond strength (N) |
||
|
Mean |
S.D. |
95% CI |
||
|
C (CerasealTM) |
UT |
202.88 |
38.21 |
(178.61-227.16) |
|
UN |
257.90 |
45.56 |
(229.02-286.79) |
|
|
A (AH plusTM) |
UT |
255.38 |
43.04 |
(228.03-282.71) |
|
UN |
263.50 |
46.47 |
(233.97-293.03) |
|
|
Remark: C=Ceraseal™, UT=Single Bond Universal adhesive with RelyX™ Ultimate resin cement, A=AH Plus™, UN=Scotchbond™ Universal Plus adhesive with RelyX™ Universal resin cement |
||||
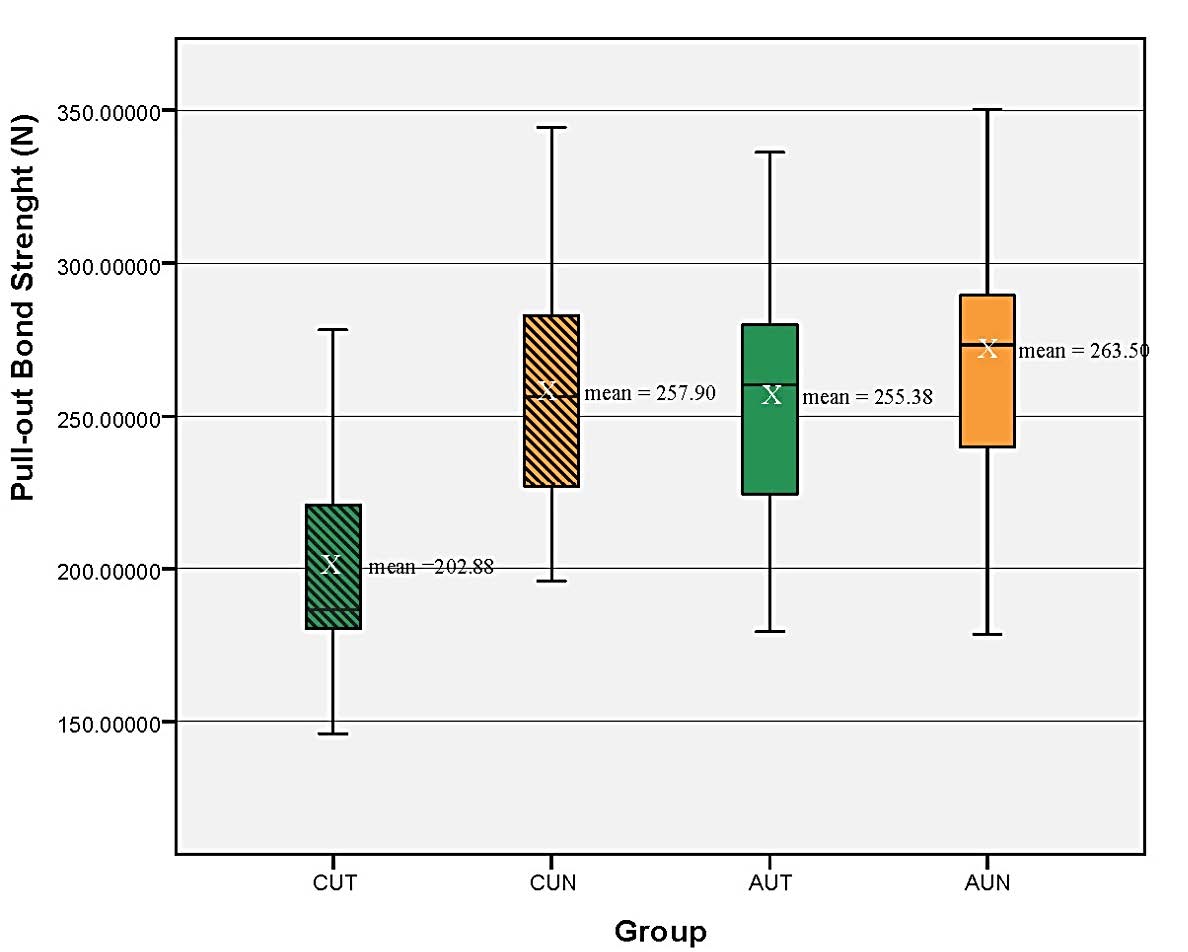
Figure 4. The box plot showed the pull-out bond strength values of the experimental groups expressed in Newton (N). The mean values were indicated by an ‘X’ inside the box plot for each group. CUT= Ceraseal™ (C)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT), CUN=Ceraseal™ (C)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN), AUT= AH Plus™ (A)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT), AUN=AH Plus™ (A)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN)
Post hoc testing using Tukey HSD indicated that pull-out bond strength values were significantly lower (-55.02) for CUT than for CUN (P = 0.008). There was a significant difference (-52.49) between the pull-out bond strength values of CUT and AUT (P = 0.024). The pull-out bond strength values were significantly lower (-60.12) for CUT than for AUN (P = 0.007). There was no significant difference (2.53) between the pull-out bond strength values of CUN and AUT (P = 0.999) and no significant difference (-5.59) between CUN and AUN (P = 0.989). There was no significant difference (8.13) between the pull-out bond strength values of AUN and AUT (P = 0.968), as shown in Table 4. The estimated marginal mean of pull-out bond strength values (N) for the experimental group is shown in Figure 5. The type of failure for each experimental group is shown in Table 5.
Table 4. Multiple comparisons between groups of types of sealers and combinations of adhesive/resin cements were analyzed by Tukey HSD.
|
Groups |
Groups |
Mean Difference |
Sig. |
95% Confidence Interval |
|
|
Lower Bound |
Upper Bound |
||||
|
CUT |
CUN |
-55.02 |
0.017* |
-102.34 |
-7.70 |
|
AUT |
-52.49 |
0.024* |
-99.81 |
-5.16 |
|
|
AUN |
-60.12 |
0.007* |
-107.94 |
-13.29 |
|
|
CUN |
CUT |
55.02 |
0.017* |
7.70 |
102.34 |
|
AUT |
2.53 |
0.999 |
-44.79 |
49.85 |
|
|
AUN |
-5.59 |
0.989 |
-52.92 |
41.72 |
|
|
AUT |
CUT |
52.49 |
0.024* |
5.16 |
99.81 |
|
CUN |
-2.53 |
0.999 |
-49.85 |
44.79 |
|
|
AUN |
-8.13 |
0.968 |
-55.45 |
39.19 |
|
|
AUN |
CUT |
60.12 |
0.007* |
13.29 |
107.94 |
|
CUN |
5.59 |
0.989 |
-41.72 |
52.92 |
|
|
AUT |
8.13 |
0.968 |
-39.19 |
55.45 |
|
|
Note: * The mean difference is significant at the 0.05 level. Remark: CUT= Ceraseal™ (C)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT), CUN=Ceraseal™ (C)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN), AUT= AH Plus™ (A)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT), AUN=AH Plus™ (A)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN) |
|||||
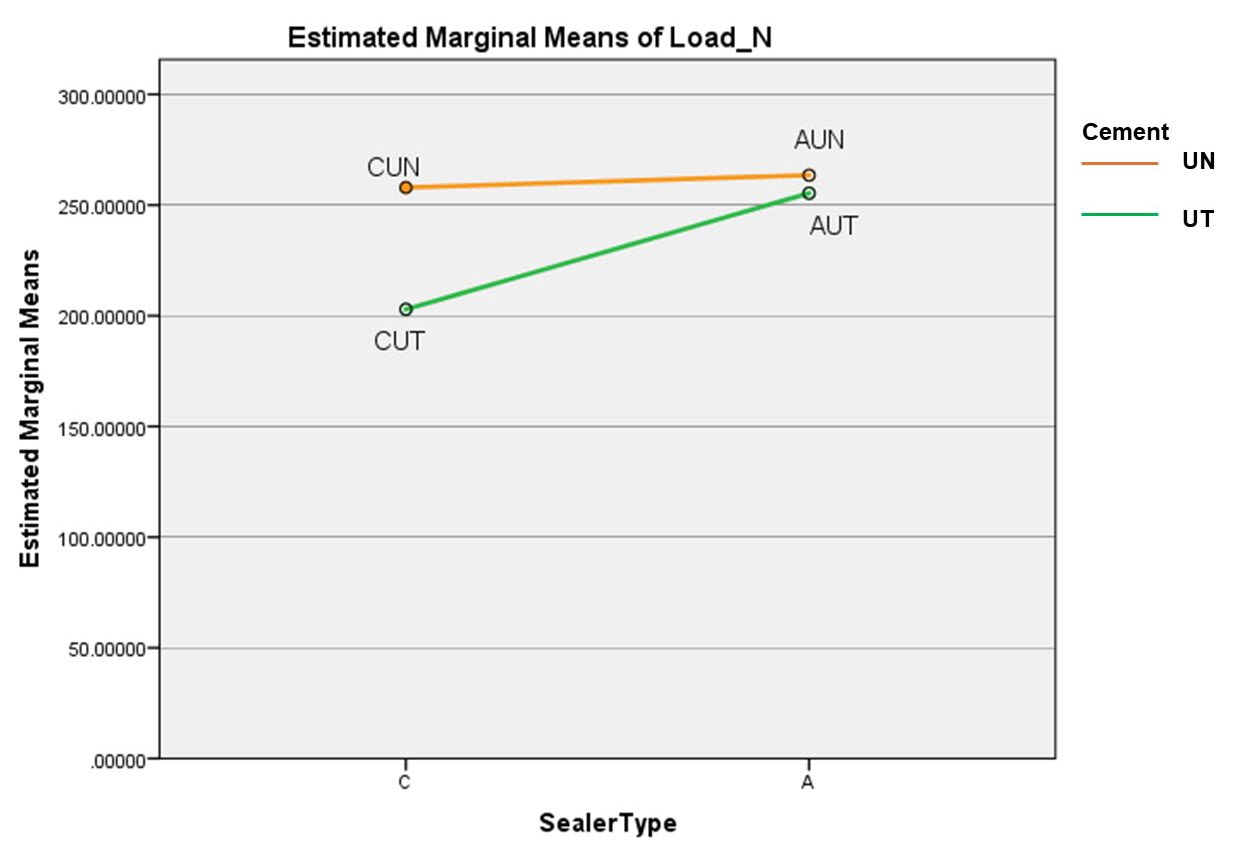
Figure 5. Estimated marginal means of the pull-out bond strength values (N) of the experimental groups; N=Newton, CUT= Ceraseal™ (C)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT), CUN=Ceraseal™ (C)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN), AUT= AH Plus™ (A)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT), AUN=AH Plus™ (A)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN)
Table 5. Type of failure.
|
Group |
Adhesive n (%) |
Cohesive n (%) |
Mixed n (%) |
Total n (%) |
|
CUT |
2 (16.67) |
1 (8.33) |
9 (75.00) |
12 (100) |
|
CUN |
4 (33.33) |
2 (16.67) |
6 (50.00) |
12 (100) |
|
AUT |
0 (0) |
0 (0) |
12 (100) |
12 (100) |
|
AUN |
4 (33.33) |
2 (16.67) |
6 (50.00) |
12 (100) |
|
Total |
10 (20.84) |
5 (10.41) |
33 (68.75) |
48 (100) |
|
Remark: CUT= Ceraseal™ (C)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT), CUN=Ceraseal™ (C)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN), AUT= AH Plus™ (A)/Single Bond Universal adhesive with RelyX™ Ultimate resin cement (UT), AUN=AH Plus™ (A)/Scotchbond Universal Plus adhesive with RelyX™ Universal resin cement (UN) |
||||
DISCUSSION
This study revealed that both the types of root canal sealers and the adhesive/resin cement combinations significantly influence the pull-out bond strength values, resulting in the rejection of the null hypothesis (H₀).
The variation in bond strength seen in various research might be due to variations in the designs and methodologies used (Singh et al. 2021; Pinto et al. 2024). In the present study, the pull-out test was chosen as the evaluation technique due to its advantages. It provides a more even distribution of stress across the bonded interface between the fiber post and root dentin, facilitating a precise measurement of the bond strength (Santos et al., 2017). Additionally, the pull-out test allows for the entire fiber post and root canal to be included in the analysis without the need for specimen sectioning. This is important because sectioning can introduce micro-fractures or damage the interface, potentially leading to early failure and compromising the accuracy of the bond strength test findings (Perdigão et al., 2007).
The bonding of fiber posts in root dentin is substantially impacted by the success of proper polymerization of resin-matrix cement (Theodosopoulou and Chochlidakis, 2009). The present study finds that the use of calcium silicate-based sealer significantly negatively impacted the pull-out bond strength values, similar to the previous study which suggests a negative effect of calcium silicate-based sealers on push-out bond strength compared to resin-based sealer when using conventional resin cement (Nesello et al., 2022). The observed reduction in bond strength is likely attributable to the inherent properties of calcium silicate-based sealers. Their small particle size (<2 μm) allows for deeper penetration into dentinal tubules (typically ranging from 2-4 μm in diameter), potentially enhancing sealing efficacy (Goldberg et al., 2011; Nagas et al., 2012; Giacomino et al., 2019), nevertheless these properties may interfere with the polymerization of resin cement to the root dentin.
Calcium silicate-based sealer are hydraulic, necessitating water for their setting reaction. This process yields calcium silicate hydrate gel (CSH, CaO·SiO·H₂O) and calcium hydroxide (Ca(OH)₂) (Sfeir et al., 2021), resulting in an initially high pH environment. The calcium ions released from calcium silicate-based sealers may interact with the components of the resin cement, potentially affecting the polymerization process. The alkaline nature of calcium silicate-based sealers can potentially interfere with the polymerization of resin-based cements (Turker et al., 2020), as these materials rely on acidic primers or adhesives to interact effectively with dentin (Turker et al., 2020). Consequently, the adverse impact of calcium silicate-based sealers on the polymerization of resin cement to root dentin is a plausible explanation for the observed decrease in bond strength.
AH PlusTM sealer is epoxy resin-amine-based material, shares compositional similarities with resin cement used for fiber post cementation. This similarity might also consider the lack of any negative effect of AH PlusTM on the bonding strength of fiber posts. These findings are consistent with the results reported in other research (Cecchin et al., 2011; Soares et al., 2020), comparable to the highest values in bond strength values of the AHplusTM group reported in this study. This finding further supports the notion that resin-based sealer's composition plays a crucial role in its adhesive properties.
Other factors influencing fiber post-adhesion, as identified in previous studies, include adhesive system (Graiff et al., 2014; Gundogdu and Aladag, 2018) and resin cement type (Liu et al., 2014). In terms of resin cement types (Liu et al., 2014), RelyXTM Ultimate adhesive resin cement exhibits high bond strength to root dentin by forming a durable micromechanical and chemical bond through its interaction with Adhesive system (3M ESPE 2011). Meanwhile, RelyXTM Universal resin cement is a more recent product that aims to simplify the cementation process by combining the benefits of various resin cement into one universal solution. It is designed to be used with or without a separate adhesive. Both types are classified as dual-cure resin cements, which are recommended for luting fiber posts. This is because dual-cure properties compensate for reduced light penetration and facilitate complete polymerization within the root canal (Liu et al., 2014; AlMadi et al., 2021). Regarding adhesive system, Single Bond UniversalTM is ethanol and water-based, containing MDP (methacryloyloxydecyl dihydrogen phosphate) for effective chemical bonding to dentin, enamel, and metals (3M Oral Care, 2016). In contrast, ScotchbondTM Universal Plus features an enhanced formulation with additional hydrophilic monomers, improving bonding performance and moisture tolerance (3M Oral Care 2020). Both adhesives are designed for use in total-etch, self-etch, and selective-etch techniques, providing versatility and simplifying clinical procedures with a one-step application process (3M Oral Care, 2016; 2020).
The present study revealed that using a combination of ScotchbondTM Universal Adhesive and RelyXTM Universal Resin Cement enhanced the pull-out bond strength value compared to using resin-based sealers or calcium-silicate-based sealers. This improved performance in this experimental group can be attributed to two potential factors.
The first potential factor is the optimized silane formulation in the ScotchbondTM Universal Plus. Following the manufacturer’s guidelines and the previous studies (Giannini et al., 2022) which stated that the amino-functional silane added in ScotchbondTM Universal Plus shows better bonding performance and higher bond strength than Single Bond Universal Adhesive (Yao et al., 2021). The advantages of this silane formulation include: 1) enhanced bonding performance and higher bond strength: this improvement is attributed to the presence of 3-(aminopropyl) triethoxysilane (APTES), which stabilizes pre-hydrolyzed silane through intramolecular hydrogen bonding, and 2) improved stability in Aqueous Acid Solutions: Unlike the Single Bond Universal Adhesive, the silane formulation in ScotchbondTM Universal Plus is less prone to degradation in aqueous acidic conditions, which can adversely affect bond strength (Yao et al., 2021).
The second potential factor is the new initiator in ScotchbondTM Universal Plus Adhesive plays a crucial role in the polymerization process. When the adhesive comes into contact with the activator in RelyXTM Universal resin cement, the initiator triggers and promotes polymerization. This is particularly beneficial for post cementation within the root canal, where light penetration from the curing unit may be limited. This improved polymerization within the canal could contribute to the enhanced bond strength observed in the AUN group (3M, 2020).
In the present study, the predominance of mixed failures, where the resin cement cover 75% of the post surface, across all groups suggests that the bond strength at the interface between the dentin and the fiber post is influenced by both the adhesive and cohesive properties of the materials used. This indicates that both the bond strength at the interfaces and the internal strength of the materials were challenged. The experiments were designed to closely simulate actual clinical procedures, and therefore, failures may occur due to multiple factors (Alnaqbi et al., 2018). The adhesive failure was found to be higher in the Calcium silicate-based sealer groups (CUT and CUN) compared to the epoxy sealer groups (AUT and AUN). This difference may be attributed to the residual Calcium silicate-based sealer remaining on the root canal surface, which has a lower bondability to the resin cement than the epoxy sealer, AH Plus.
Thus, this research aims to bridge this knowledge gap by evaluating a novel adhesive-cement combination for its suitability in fiber post cementation. The choice of root canal sealer and resin cement significantly impacts the pull-out bond strength of fiber posts, this information is crucial for clinicians in selecting the appropriate materials to optimize the retention and stability of fiber posts in endodontically treated teeth.
CONCLUSION
Within the limitations of this in vitro study, the type of root canal sealer and the combination of adhesive/resin cements significantly influence pull-out bond strength values. Using calcium-silicate-based sealers may reduce pull-out bond strength values in certain adhesive/resin cement combinations.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the Research Office, Faculty of Dentistry, Mahidol University, for their continuous support throughout the experimental process.
AUTHOR CONTRIBUTIONS
Pimpinee Eamsa-ard Roles: Conceptualization, Supervision, Methodology, Investigator, Manuscript editing and Project Administration.
Prattana Yodmanotham Roles: Corresponding author, Conceptualization, Supervision, Methodology, Investigator, Statistical Analysis, Manuscript writing, and Manuscript editing and preparation.
Jidapa Saelee, Pimsiri Awsakulsutthi, Poolvalee Poolsawat, and Yotyothin Ketiphan Roles: Investigators.
CONFLICT OF INTEREST
The authors declare that they hold no competing interests.
REFERENCES
3M. 2020. 3M™ Relyx™ universal resin cement study booklet.
3M ESPE. 2011. Relyx™ ultimate adhesive resin cement technical data sheet. In: 3M ESPE, editor. 82229 Seefeld · Germany.
3M Oral Care. 2016. 3M single bond universal adhesive technical data sheet: Single bond universal technical data. In: 3M, editor. St. Paul, MN 55144-1000 USA.
3M Oral Care. 2020. 3M scotchbond universal plus adhesive brochure: Scotchbond universal plus brochure. In: Kingdom MU, editor. Leicestershire, LE11 5RB, UK.
AlMadi, M., Khabeer, A., AlHila,l S, AlShahrani, A., and Ali, S. 2021. Pull-out bond strength of fiber post luted with two types of resin luting cements using different light curing units. Nigerian Journal of Clinical Practice. 24(12): 1841-1845.
Alnaqbi, I. O. M., Elbishari, H., and Elsubeihi, E. S. 2018. Effect of fiber post-resin matrix composition on bond strength of post-cement interface. International Journal of Dentistry. 2018(1): 4751627.
Alsubait, S.A. 2021. Effect of calcium silicate-based endodontic sealer on the retention of fiber posts cemented at different time intervals. The Saudi Dental Journal. 33(7):718-723.
Cecchin, D., Farina, A., Souza, M., Carlini‐Júnior, B., and Ferraz, C. 2011. Effect of root canal sealers on bond strength of fiberglass posts cemented with self‐adhesive resin cements. International Endodontic Journal. 44(4): 314-320.
Dammaschke, T., Steven, D., Kaup, M., and Ott, K. H. 2003. Long-term survival of root-canal-treated teeth: A retrospective study over 10 years. Journal of Endodontics. 29(10): 638-643.
Eskandari, F., Razavian, A., Hamidi, R., Yousefi, K., and Borzou, S. 2022. An updated review on properties and indications of calcium silicate-based cements in endodontic therapy. International Journal of Dentistry. 2022(1): 6858088.
Faul, F., Erdfelder, E., Lang, A.-G., and Buchner, A. 2007. G* power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 39(2): 175-191.
Forough Reyhani, M., Ghasemi, N., Rahimi, S., Milani, A. S., and Omrani, E. 2016. Effect of different endodontic sealers on the push-out bond strength of fiber posts. Iranian Endodontic Journal. 11(2): 119-123.
Giacomino, C. M., Wealleans, J. A., Kuhn, N., and Diogenes, A. 2019. Comparative biocompatibility and osteogenic potential of two bioceramic sealers. Journal of Endodontics. 45(1): 51-56.
Giannini, M., Vermelho, P. M., de Araújo Neto, V. G., and Soto-Montero, J. R. 2022. An update on universal adhesives: Indications and limitations. Current Oral Health Reports. 9(3): 57-65.
Goldberg, M., Kulkarni, A. B, Young, M., and Boskey, A. 2011. Dentin: Structure, composition and mineralization. Frontiers in Bioscience-Elite. 3(2): 711-735.
Graiff, L., Rasera, L., Calabrese, M., and Vigolo, P. 2014. Bonding effectiveness of two adhesive luting cements to glass fiber posts: Pull-out evaluation of three different post surface conditioning methods. International Journal of Dentistry. 2014: 148571.
Gundogdu, M. and Aladag, L. 2018. Effect of adhesive resin cements on bond strength of ceramic core materials to dentin. Nigerian Journal of Clinical Practice. 21(3): 367-374.
IBM Corp. . 2019. Ibm spss statistics for windows, version 26.0. IBM Corp.: Armonk, NY, USA.
Kansal, R., Rani, S., Kumar, M., Kumar, S., and Issar, G. 2018. Comparative evaluation of shear bond strength of newer resin cement (relyx ultimate and relyx u200) to lithium disilicate and zirconia ceramics as influenced by thermocycling. Contemporary Clinical Dentistry. 9(4): 601-606.
Khongkhunthian, P. and Tanmukayakul, K. 2007. Nickel-titanium rotary instrument separation during root canal preparation by dental students: A comparison between a strict crown down technique and a modified crown-down/step back technique. Chiang Mai University Journal of Natural Sciences. 6(2): 11.
Kim, B.-N., Son, S.-A., and Park, J.-K. 2020. Effect of exclusive primer and adhesive on microtensile bond strength of self-adhesive resin cement to dentin. Materials. 13(10): 2353.
Lim, M., Jung, C., Shin, D. H., Cho, Y. B., and Song, M. 2020. Calcium silicate-based root canal sealers: A literature review. Restorative Dentistry and Endodontics. 45(3): e35.
Liu, C., Liu, H., Qian, Y. T., Zhu, S., and Zhao, S. Q. 2014. The influence of four dual-cure resin cements and surface treatment selection to bond strength of fiber post. International Journal of Oral Science. 6(1): 56-60.
Macedo, G. V., Yamauchi, M., and Bedran-Russo, A.K.B. 2009. Effects of chemical cross-linkers on caries-affected dentin bonding. Journal of Dental Research. 88: 1096-1100.
Nagas, E., Uyanik, M. O., Eymirli, A., Cehreli, Z. C., Vallittu, P. K., Lassila, L. V. J, and Durmaz, V. 2012. Dentin moisture conditions affect the adhesion of root canal sealers. Journal of Endodontics. 38(2): 240-244.
Nesello, R., Silva, I. A., Bem, I. A. D., Bischoff, K., Souza, M. A., Só, M. V. R, Rosa, R. A. D. 2022. Effect of bioceramic root canal sealers on the bond strength of fiber posts cemented with resin cements. Brazilian Dental Journal. 33: 91-98.
Nica, L., Todea, C., Gabriel, F., and Baldea, B. 2013. How to bond to root canal dentin. Progress in Biomedical Optics and Imaging - Proceedings of SPIE. 8925.
Perdigao, J., Araujo, E., Ramos, R. Q., Gomes, G., and Pizzolotto, L. 2021. Adhesive dentistry – current concepts and clinical considerations. Journal of Esthetic and Restorative Dentistry. 33: 51-58.
Pinto, C., França, F., Basting, R. T., Turssi, C. P., and Amaral, F. 2024. Evaluation of bond strength of three glass fiber post-systems cemented to large root canals. Operative Dentistry. 49: 222-230.
Perdigão, J., Gomes, G., and Augusto, V. 2007. The effect of dowel space on the bond strengths of fiber posts. Journal of Prosthodontics. 16(3): 154-164.
Prisco, D., De Santis, R., Mollica, F., Ambrosio, L., Rengo, S., and Nicolais, L. 2003. Fiber post adhesion to resin luting cements in the restoration of endodontically treated teeth. Operative Dentistry. 28: 515-521.
Radovic, I., Monticelli, F., Goracci, C., Vulicevic, Z. R., and Ferrari, M. 2008. Self-adhesive resin cements: A literature review. The Journal of Adhesive Dentistry. 10(4): 251-258.
Santos, F. C, D, Banea, M. D, Carlo, H. L, and De Barros, S. 2017. Test methods for bond strength of glass fiber posts to dentin: A review. The Journal of Adhesion. 93(1-2): 159-186.
Sfeir, G., Zogheib, C., Patel, S., Giraud, T., Nagendrababu, V., and Bukiet, F. 2021. Calcium silicate-based root canal sealers: A narrative review and clinical perspectives. Materials. 14(14): 3965.
Singh, N., Garg, A., and Mittal, R. 2021. Comparative evaluation of pull-out bond strength of fiber post using different luting cements in endodontically treated teeth: An in-vitro study. Endodontology. 33: 165-169.
Sjögren, U., Hägglund, B., Sundqvist, G., and Wing, K. 1990. Factors affecting the long-term results of endodontic treatment. Journal of Endodontics. 16(10): 498-504.
Soares, I. M. V, Crozeta, B. M., Pereira, R. D, Silva, R. G., and da Cruz-Filho, A. M. 2020. Influence of endodontic sealers with different chemical compositions on bond strength of the resin cement/glass fiber post junction to root dentin. Clinical Oral Investigations. 24(10): 3417-3423.
Theodosopoulou, J. N. and Chochlidakis, K. M. 2009. A systematic review of dowel (post) and core materials and systems. Journal of Prosthodontics. 18(6): 464-472.
Turker, N., Buyukkaplan, U. Ş., Başar, E. K., and Özarslan M. M. 2020. The effects of different surface treatments on the shear bond strengths of two dual-cure resin cements to cad/cam restorative materials. The Journal of Advanced Prosthodontics. 12(4): 189.
Vilas-Boas, D. A., Grazziotin-Soares, R., Ardenghi, D. M. , Bauer, J., de Souza, P. O., de Miranda Candeiro, G. T., Maia-Filho, E. M., and Carvalho, C. N. 2018. Effect of different endodontic sealers and time of cementation on push-out bond strength of fiber posts. Clinical Oral Investigations. 22: 1403-1409.
Yao, C., Ahmed, M. H., De Grave, L., Yoshihara, K., Mercelis, B., Okazaki, Y., Van Landuyt, K. L., Huang, C., and Van Meerbeek, B. 2021. Optimizing glass-ceramic bonding incorporating new silane technology in an experimental universal adhesive formulation. Dental Materials Journal. 37(5): 894-904.
OPEN access freely available online
Natural and Life Sciences Communications
Chiang Mai University, Thailand. https://cmuj.cmu.ac.th
Pimpinee Eamsa-ard, Prattana Yodmanotham *, Jidapa Saelee, Pimsiri Awsakulsutthi, Poolvalee Poolsawat, and Yotyothin Ketiphan
College of Dental Medicine, Rangsit University, Pathum Thani 12000, Thailand.
Corresponding author: Prattana Yodmanotham, E-mail: prattana.y@rsu.ac.th
ORCID: Prattana Yodmanotham: https://orcid.org/0009-0003-7070-9584
Total Article Views
Editor:Anak Iamaroon,
Chiang Mai University, Thailand
Article history:
Received: August 4, 2024;
Revised: December 7, 2024;
Accepted: December 11, 2024;
Online First: January 15, 2025

