
Effectiveness of Herbal Steam Bath Therapy for Quality of Life and Sleep Quality in Post-Covid-19 Patients
Rossarin Paithoon, Kusuma Sriyakul, Parunkul Tungsukruthai, Nunthiya Srikaew, Pornchai Sawangwong, Sucharat Tungsukruthai, and Pratya Phetkate*Published Date : November 22, 2024
DOI : https://doi.org/10.12982/NLSC.2025.009
Journal Issues : Number 1, January-March 2025
Abstract The objective of this study was to evaluate the effectiveness of herbal steam bath (HSB) therapy on the quality of life and sleep quality in post-COVID-19 patients. This randomized controlled trial involved 68 participants, who were divided into two groups: the intervention group received HSB combined with standard care, while the control group received only standard care. The HSB therapy was administered three times a week for four weeks. Outcome measures included the WHOQOL-BREF-THAI for quality of life, the Pittsburgh Sleep Quality Index (PSQI) for sleep quality, and the Thai Distress Thermometer for distress levels. The results indicated that HSB significantly improved the overall quality of life (P ≤ 0.05) and various components of sleep quality, such as overall sleep quality (P ≤0.05), sleep latency (P ≤ 0.05), sleep duration (P ≤ 0.05), and sleep disturbances (P ≤ 0.05). Additionally, HSB significantly reduced distress levels in the emotional domain (P ≤ 0.05). This study concludes that HSB might be beneficial in reducing distress, improving sleep quality, and consequently enhancing the quality of life among post-COVID-19 patients.
Keywords: Post-COVID-19, Herbal steam bath, Quality of life, Sleep quality
Funding: This study was funded by the Thai Traditional Medicine Knowledge Fund, the Department of Thai Traditional and Alternative Medicine (DTAM), Ministry of Public Health, Thailand (grant number: 67-04-2-10-01).
Citation: Paithoon, R., Sriyakul, K., Tungsukruthai, P., Srikaew, N., Sawangwong, P., Tungsukruthai, S., Phetkate, P. 2025. Effectiveness of herbal steam bath therapy for quality of life and sleep quality in post-covid-19 patients. Natural and Life Sciences Communications. 24(1): e2025009.
INTRODUCTION
COVID-19, caused by the SARS-CoV-2 virus emerges as a highly contagious disease. It rapidly transforms into a worldwide health emergency, placing significant burden on public health infrastructures across numerous countries (DeSalvo et al., 2021; Filip et al., 2022; Thaikruea et al., 2022). Despite notable reductions in acute COVID-19 mortality and severity, there are still unresolved problems concerning the long-term sequelae of post-COVID-19 infection, particularly regarding distress-related symptoms. (Peter et al., 2022).
Post-acute sequelae of SARS-CoV-2 infection, also known as post-COVID-19, refer to a range of symptoms that can last for weeks, months, or even years after the initial recovery from acute COVID-19. (Parotto et al., 2023). This condition impacts approximately 30% of individuals who have recovered from the virus with various symptoms including fatigue, dyspnea, memory loss, depression, and significant sleep disturbances (Fernandez-de-Las-Peñas et al., 2024; Huerne et al., 2023; Yong, 2021). Among these, psychological distress has been increasingly recognized as a prevalent issue in post-COVID-19 individuals, encompassing symptoms such as irritability, emotional instability, and depressive mood. Such distress contributes to a decline in mental health and overall well-being, highlighting the need for targeted interventions (Javed et al., 2020; Pei et al., 2024).
Sleep disturbances are particularly prominent in this context, with numerous studies linking post-COVID-19 to insomnia and other sleep disorders (Moreno et al., 2022; Shaik et al., 2023). The pathophysiology of these disturbances has been attributed to the virus's potential to induce blood-brain-barrier (BBB) disruption and neuroinflammation. (Semyachkina-Glushkovskaya et al., 2021). These mechanisms may not only explain sleep disturbances but also shed light on the broader spectrum of distress-related symptoms observed in post-COVID-19 patients. These persistent symptoms notably affect the quality of life, with up to half of the patients experiencing prolonged health issues months after overcoming the infection (Malik et al., 2022). Furthermore, this complex interplay of factors makes post-COVID-19 a significant challenge for healthcare systems worldwide (Jazieh and Kozlakidis, 2020).
Nowadays, the persistence of post-COVID-19 symptoms even in highly vaccinated populations points to the need for effective therapeutic interventions. While pharmacological treatments are commonly utilized, there is a growing recognition of the benefits of non-pharmacological interventions in managing these symptoms (Chandan et al., 2023; He et al., 2024). In Thailand, herbal steam bath (HSB) therapy is a traditional non-pharmacological practice widely used to alleviate various ailments. Typically, the HSB formula used in practice is adapted from the hot herbal compress formula listed in the National List of Essential Medicine. This standardized HSB formula is used in traditional medicine units within general hospitals, as it relies on locally available herbs that are easily sourced and well-documented for their safety and efficacy (Tungsukruthai et al., 2018; Nootim et al., 2019). For example, a previous study reported that HSB can significantly reduce the symptoms of allergic rhinitis including sneezing, nasal itching, and nasal congestion (Tungsukruthai et al., 2018). Moreover, preliminary observations suggest that HSB may offer potential benefits for treating and rehabilitating patients with post-COVID-19 symptoms, potentially improving depression, insomnia, and overall quality of life (Nootim et al., 2019; Cohen, 2020; Wattanakittikul et al., 2022; Thairatnopas et al., 2023). However, empirical research on its efficacy in this context remains limited, necessitating structured clinical studies to assess its effectiveness. This study specifically aims to address this gap by examining the impact of HSB on sleep quality and quality of life in post-COVID-19 patients, with a focus on alleviating distress and related symptoms.
MATERIAL AND METHODS
Materials
Preparation of the herbal formula
The herbal formula for the steam bath therapy was prepared by a Thai traditional pharmacist at the hospital, which is under the department of Thai traditional and alternative medicine, ministry of public health, Thailand. This formula includes fresh herbs such as Zingiber cassumunar Roxb. (rhizome) 50 g., Curcuma longa L. (rhizome) 10 g., Cymbopogon citratus Stapf. (leaves and stalks)10 g., Acacia concinna (Willd.) DC. (leaves) 10 g., Tamarindus indica L. (leaves) 30 g., and Citrus hystrix DC. (peel) 20 g., along with camphor 30 g. and rock salt 15 g. These ingredients were carefully chosen and combined to maintain the authenticity and effectiveness of the treatment according to Thai traditional medicine practices.
Methods
Study design & setting
This research is a clinical study using a randomized controlled trial design. Data collection was conducted at the Thai Traditional and Complementary Medicine Hospital, under the department of Thai traditional and alternative medicine, ministry of public health, Thailand. The study protocol was approved by the Ethics Committee of the Faculty of Medicine at Thammasat University (approval no. MTU-MTU-EC-OO-0-013/66).
Participants
This study required a sample size of 64 participants, calculated using the G-Power program to ensure statistical validity, with parameters set for a significance level of 0.05 (α-error), a power of 0.9, and an effect size of 0.72. These parameters were based on findings from a previous study conducted by Tungsukruthai et al. in 2018 (Tungsukruthai et al., 2018). To achieve the necessary statistical power, the trial included a minimum of 34 participants in each group. Eligible participants were adults between the ages of 20 and 60 who had previously been diagnosed with COVID-19, confirmed either through RT-PCR or an antigen test kit (ATK). Furthermore, participants were required to have recovered from the virus, as evidenced by a negative test result obtained from 2 weeks to 6 months prior to the study. A normal chest x-ray was also a prerequisite for inclusion. Participants were required to display at least two post-COVID-19 symptoms to qualify for the study. Such criteria ensured that the study focused on individuals experiencing lingering effects of the virus. The study excluded certain populations to maintain the integrity of the results and ensure participant safety. Excluded groups included pregnant or lactating women, individuals presenting with a fever, and persons experiencing acute symptoms such as dizziness, nausea, vomiting, or diarrhea. Additionally, patients with severe skin conditions, open wounds, or a history of allergies to herbs, steam, or heat were not eligible. The trial also excluded individuals with congenital diseases like asthma, kidney disease, heart disease, epilepsy, high blood pressure, paralysis, or severe respiratory diseases, such as chronic obstructive pulmonary disease. These exclusions helped to focus the study on a participant group whose conditions did not confound the assessment of post-COVID-19 symptoms.
Randomization and blinding
Participants were randomly assigned to either the intervention (HSB) or control (standard care) groups using a computer-generated randomization sequence. Allocation was performed by an independent researcher who was not involved in data collection or analysis. Although blinding of participants was not feasible due to the nature of the intervention, outcome assessors were blinded to group allocation to minimize bias.
Interventions
The first group received HSB therapy combined with standard care for post-COVID-19, administered three times a week for four consecutive weeks. The standard group (STD) received only the standard care for post-COVID-19, which included physician consultations, symptom monitoring, and guidance on lifestyle modifications. No herbal or steam therapies were provided to this group. This ensured a clear comparison between HSB therapy and conventional post-COVID-19 management. The HSB process adhered to the standards set by the guidelines of the Thai traditional medicine practice, department of Thai traditional and alternative medicine, ministry of public health, Thailand. The HSB included herbs known for their essential oils, anti-inflammatory properties, and bronchodilator effects, with the primary ingredient being Zingiber cassumunar Roxb., along with other herbs. The herbal steam mixture was prepared by a Thai traditional pharmacist at the hospital, under the standards of Thai traditional medicine pharmacology, ensuring the quality of the raw materials.
Outcome measurements
To evaluate the effects of HSB therapy combined with standard care versus standard care alone on post-COVID-19 patients, outcome measurements were taken both before treatment and at the endpoint. The outcome measures included: the WHOQOL-BREF-THAI, which assesses quality of life through perceived objective and self-report subjective questions across four domains such as physical health, psychological state, social relationships, and environment; the Pittsburgh Sleep Quality Index (PSQI), a questionnaire evaluating seven components of sleep quality over the past month, such as subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction, where scores of 5 or less indicate good sleep quality and scores above 5 indicate poor sleep quality; and the Thai Distress Thermometer, a tool comprising a 1-10 scale for distress levels over the past week and a checklist of 21 factors contributing to distress, categorized into emotional issues, physical problems, and overall distress.
Statistical analysis
The data were analyzed using a per-protocol approach with SPSS software, version 25.0. Participant characteristics were summarized and reported as frequencies and percentages. Normality of the outcome variables was performed using the Shapiro–Wilk and Kolmogorov–Smirnov tests. Changes in outcome measures from baseline to post-intervention were examined using paired t-test. For comparisons between the two groups, independent samples t-tests were used. A P-value of less than 0.05 was considered statistically significant.
RESULTS
Participant characteristics
118 potential participants with post-COVID-19 symptoms were screened, 68 individuals met the inclusion criteria. They were randomly assigned to two groups according to the research methodology, with 34 individuals in each group. All participants agreed to participate and remained engaged until the end of the research project, with no loss to follow-up during the study period (Figure 1). The demographic and baseline characteristics of the participants, including gender, age, education level, occupation, monthly income, presence of chronic illness, mental illness, and the number of time for COVID-19 infections, are summarized (Table 1). Statistical analyses revealed no significant differences between the two groups regarding these demographic characteristics, except for the number of time for COVID-19 infections, which showed a statistically significant difference.
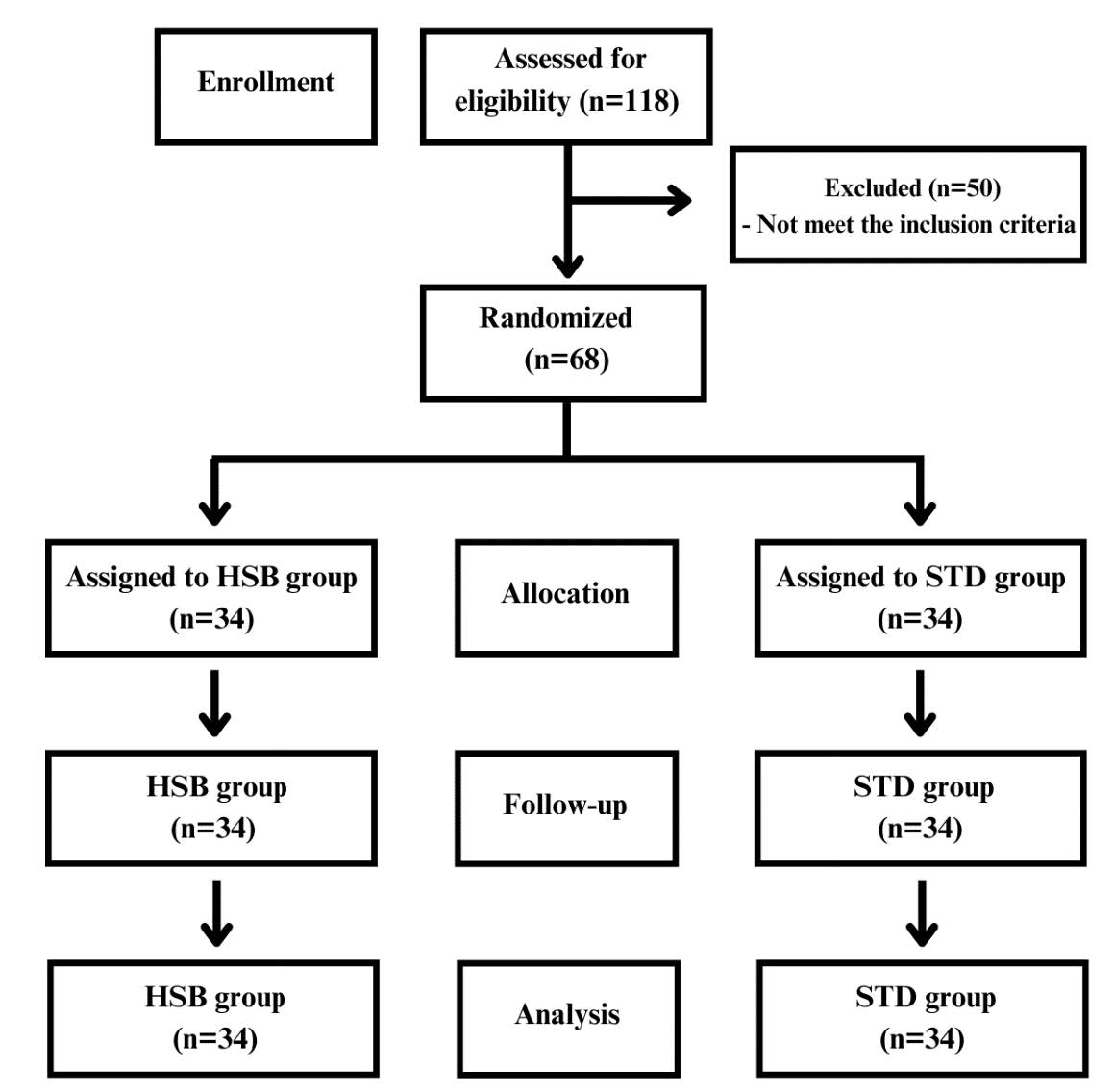
Figure 1. Flow chart of study.
Table 1. Demographic variables of the participants.
|
Demographic variables |
Number (Percentage) |
aP-value |
|
|
HSB group |
STD group |
||
|
Gender |
|
|
|
|
Women Men |
27 (79.4) 7 (20.6) |
23 (67.6) 11 (32.4) |
0.272 |
|
Age (years) |
|
|
|
|
20 – 30 years 31 – 40 years 41 – 50 years 51 – 60 years |
13 (38.2) 10 (29.4) 8 (23.6) 3 (8.8) |
13 (38.2) 15 (44.2) 5 (14.7) 1 (2.9) |
0.442 |
|
Education |
|
|
|
|
Undergraduate Bachelor Postgraduate |
10 (29.4) 19 (55.9) 5 (14.7) |
2 (5.8) 28 (82.4) 4 (11.8) |
0.062 |
|
Occupation |
|
|
|
|
Worker Officer Freelance Retired |
10 (29.4) 20 (58.9) 3 (8.8) 1 (2.9) |
4 (11.8) 26 (76.4) 0 (0.0) 4 (11.8) |
0.063 |
|
Monthly income |
|
|
|
|
≤ 20,000 > 20,000 |
21 (61.8) 13 (38.2) |
17 (50.0) 17 (50.0) |
0.053 |
|
Chronic illness |
|
|
|
|
No |
27 (79.4) |
28 (82.4) |
0.803 |
|
Yes |
7 (20.6) |
6 (17.6) |
|
|
Mental illness |
|
|
|
|
No |
34 (100.0) |
34 (100.0) |
- |
|
Yes |
0 (0) |
0 (0) |
|
|
COVID infected times |
|
|
|
|
1 time 2 times 3 times > 3 times |
24 (70.6) 9 (26.5) 1 (2.9) 0 (0.0) |
12 (35.3) 19 (55.9) 2 (5.9) 1 (2.9) |
0.031* |
Note: Data were expressed as number percentage, aStudent t-test or Fisher’s exact test, *significant difference at P ≤ 0.05.
The effect of herbal steam bath therapy on quality of life
The results of the quality-of-life assessment using the 26-Item WHOQOL BREF (Thai version) demonstrated significant improvements in the HSB group across multiple domains. Specifically, the physical health domain showed substantial enhancement post-intervention (P < 0.01), indicating a shift from moderate to good quality of life, while the STD group also showed some improvements (P < 0.01) but remained within the moderate range. The psychological health domain improved significantly in the HSB group (P < 0.01), moving from moderate to good quality, while the STD group showed no significant change, remaining in the moderate range. Social relations remained relatively unchanged in both groups, with no significant differences observed post-intervention, indicating a consistent level of moderate quality. The environment domain did not show significant changes in either group, remaining in the moderate quality range. Notably, the overall quality of life score significantly improved in the HSB group (P < 0.01), indicating a shift from moderate to good quality, compared to the STD group, which also showed improvement (P < 0.01) but remained within the moderate range. The between-group comparison post-intervention (P < 0.05) further highlights the effectiveness of HSB therapy in enhancing the quality of life in post-COVID-19 patients, as shown in Table 2.
Table 2. The comparison of the 26-Item WHOQOL BREF between groups before intervention and post-intervention.
|
WHOQOL BREF (Domain) |
Pre-intervention |
Post-intervention |
aP-value |
|
Physical health domain |
|
|
|
|
HSB |
18.15 ± 4.28 |
22.06 ± 4.27 |
< 0.001* |
|
STD |
17.7 ± 5.07 |
18.38 ± 4.79 |
< 0.001* |
|
bP-value |
0.699 |
0.001* |
|
|
Psychological health domain |
|
|
|
|
HSB |
17.88 ± 3.91 |
20.74 ± 3.74 |
< 0.001* |
|
STD |
19.29 ± 5.02 |
19.62 ± 5.19 |
0.078 |
|
bP-value |
0.200 |
0.312 |
|
|
Social relations domain |
|
|
|
|
HSB |
13.53 ± 1.21 |
13.26 ± 1.99 |
0.425 |
|
STD |
13.62 ± 1.16 |
13.71 ± 1.09 |
0.083 |
|
bP-value |
0.760 |
0.261 |
|
|
Environment domain |
|
|
|
|
HSB |
23.15 ± 3.87 |
23.38 ± 3.74 |
0.058 |
|
STD |
22.88 ± 3.49 |
23.18 ± 3.29 |
0.058 |
|
bP-value |
0.768 |
0.810 |
|
|
Overall QOL |
|
|
|
|
HSB |
72.71 ± 6.81 |
79.44 ± 6.02 |
< 0.001* |
|
STD |
73.5 ± 9.77 |
74.88 ± 9.96 |
< 0.001* |
|
bP-value |
0.699 |
0.026* |
< 0.001* |
Note: Data were expressed as mean ± standard deviation, acompared within group; bcompared between group, *significant difference at P ≤ 0.05.
The effect of herbal steam bath therapy on symptoms of distress
The results of the symptoms of distress assessment using the Thai version of the distress thermometer measurement revealed significant improvements in the HSB group across multiple domains. Specifically, the emotional domain showed a significant reduction in distress post-intervention (P < 0.05), whereas the STD group showed no significant change. The physical domain demonstrated a substantial decrease in distress in both the HSB (P < 0.01) and STD groups (P < 0.01), with no significant difference between the groups post-intervention. Overall distress levels significantly decreased in the HSB group (P < 0.01), indicating a notable reduction in distress, while the STD group also showed a significant decrease (P < 0.05), though less pronounced. The between-group comparison for overall distress did not show a significant difference post-intervention, as shown in table 3.
Table 3. The Comparison of distress thermometer between groups before intervention and post-intervention.
|
Domain |
Pre-intervention |
Post-intervention |
aP-value |
|
Emotional domain (6 items) |
|
|
|
|
HSB |
4.21 ± 0.77 |
4.03 ± 0.67 |
0.012* |
|
STD |
4.24 ± 0.92 |
4.21 ± 0.88 |
0.325 |
|
bP-value |
0.887 |
0.357 |
|
|
Physical domain (21 items) |
|
|
|
|
HSB |
7.82 ± 2.12 |
6.44 ± 1.81 |
< 0.001* |
|
STD |
7.44 ± 2.55 |
6.38 ± 2.22 |
< 0.001* |
|
bP-value |
0.504 |
0.905 |
|
|
Overall distress |
|
|
|
|
HSB |
5.35 ± 0.73 |
4.74 ± 0.45 |
< 0.001* |
|
STD |
5.06 ± 0.89 |
4.85 ± 0.74 |
0.033* |
|
bP-value |
0.141 |
0.432 |
0.012* |
Note: Data were expressed as mean ± standard deviation, acompared within group; bcompared between group, *significant difference at P ≤ 0.05.
The effect of herbal steam bath therapy on sleep quality
Measurement of sleep quality using the PSQI revealed that HSB therapy significantly improved various components of sleep quality in post-COVID-19 patients. Sleep latency decreased (P < 0.01), sleep duration increased (P < 0.01), and sleep disturbances were reduced (P < 0.05) after the intervention. Notably, overall sleep quality showed a statistically significant improvement (P < 0.01) in the HSB group compared to the control group (P = 0.046). Although sleep efficiency showed a positive trend, it did not reach statistical significance. The use of sleeping medication and daytime dysfunction remained relatively unchanged in both the HSB and STD groups. Notably, the total PSQI score significantly improved in the HSB group (P < 0.01) compared to the STD group, as shown in table 4.
Table 4. The Comparison of PSQI components between groups before intervention and post-intervention.
|
PSQI components |
Pre-intervention |
Post-intervention |
aP-value |
|
Sleep quality |
|
|
|
|
HSB |
2.03 ± 0.58 |
1.53 ± 0.51 |
< 0.001* |
|
STD |
1.94 ± 0.74 |
1.82 ± 0.67 |
0.044* |
|
bP-value |
0.584 |
0.046* |
|
|
Sleep latency |
|
|
|
|
HSB |
2.44 ± 0.75 |
2.06 ± 0.65 |
< 0.001* |
|
STD |
2.21 ± 0.73 |
2.15 ± 0.7 |
0.160 |
|
bP-value |
0.193 |
0.592 |
|
|
Sleep duration |
|
|
|
|
HSB |
1.91 ± 0.57 |
1.71 ± 0.52 |
0.006* |
|
STD |
1.82 ± 0.52 |
1.76 ± 0.5 |
0.160 |
|
bP-value |
0.508 |
0.636 |
|
|
Sleep efficiency |
|
|
|
|
HSB |
1.88 ± 0.33 |
1.71 ± 0.52 |
0.056 |
|
STD |
1.85 ± 0.5 |
1.76 ± 0.5 |
0.184 |
|
bP-value |
0.775 |
0.636 |
|
|
Sleep disturbance |
|
|
|
|
HSB |
1.79 ± 0.48 |
1.61 ± 0.55 |
0.012* |
|
STD |
1.56 ± 0.61 |
1.53 ± 0.61 |
0.325 |
|
bP-value |
0.082 |
0.535 |
|
|
Taking sleeping medication |
|
|
|
|
HSB |
1.56 ± 0.61 |
1.53 ± 0.61 |
0.571 |
|
STD |
1.41 ± 0.57 |
1.32 ± 0.47 |
0.083 |
|
bP-value |
0.304 |
0.127 |
|
|
Daytime dysfunction |
|
||
|
HSB |
1.41 ± 0.56 |
1.35 ± 0.54 |
0.160 |
|
STD |
1.38 ± 0.55 |
1.32 ± 0.53 |
0.160 |
|
bP-value |
0.827 |
0.823 |
|
|
Total PSQI score |
|
|
|
|
HSB |
13.03 ± 1.88 |
11.5 ± 1.54 |
< 0.001* |
|
STD |
12.18 ± 2.29 |
11.68 ± 2.07 |
< 0.001* |
|
bP-value |
0.098 |
0.692 |
|
Note: Data were expressed as mean ± standard deviation, acompared within group; bcompared between group, *significant difference at P ≤ 0.05.
DISCUSSION
Patients suffering from post-COVID frequently experienced neuropsychiatric symptoms including distress, cognitive impairment, and sleep disturbances. These issues had been linked to both physical and emotional health challenges during the COVID-19 pandemic (Charoenporn et al., 2024). This randomized controlled trial provides the first empirical evidence supporting the efficacy of HSB therapy in improving the sleep quality, quality of life, and lessening distress in post-COVID-19 patients. An advantageous interpretation of our findings suggested that HSB could significantly reduce the severity of physical health domain, psychological health domain, emotional domain, and improved various components of sleep quality in post-COVID-19 patients.
Regarding post-COVID physical health domain, our investigation revealed that HSB significantly improved the physical health domain. Specifically, patients in HSB group exhibited a significant improvement from a pre-intervention score of 18.15 ± 4.28 to 22.06 ± 4.27 following the intervention. When compared to the control group, the HSB group had a significantly higher score in the physical health after four weeks of intervention (P < 0.01). Moreover, the overall quality of life score significantly improved from pre-intervention score of 72.71 ± 6.81 to 79.44 ± 6.02 post-intervention. Interestingly, the HSB group exhibited a statistically significant improvement in overall quality of life compared to the STD group after four weeks of intervention (P = 0.026). To support our finding, previous study demonstrated that steam inhalation was frequently utilized to control viral infections of the respiratory tract such as common cold. Moreover, steam inhalation might assist in symptomatic relief of COVID-19 symptoms (Kumar et al., 2022). In addition, steam inhalation at 45°C for 20 minutes could activate immune cells and suppress rhinovirus growth by more than 90% in vitro (Ali et al., 2015). Besides, prior research reported that steam inhalation with added essential oils or herbal products could assist prevent the coronavirus, especially for the treatment of patients with not very serious symptoms (Marwah and Marwah, 2020). Furthermore, inhaling essential oils from herbs to the upper respiratory tract could prevent virus spread and lower cytokines (IL-10, IL-1β and TNF-α) expression in the lung (Elsebai and Albalawi, 2022). Altogether, we summarized that HSB might alleviate the symptoms of post-COVID-19 which resulting in improvement of quality of life.
Nowadays, there is growing evidence indicating that a significant consequence of impaired sleep quality was neuroinflammation, which could lead to disruption of the blood-brain barrier (BBB). This disruption might facilitate the entry of COVID-19 into the brain, thereby exacerbating hyper-inflammation of the central nervous system (CNS) and contributing to the development of COVID-19 related sleep disorders (Semyachkina-Glushkovskaya et al., 2021). Additionally, COVID-19 was associated to approximately a 50% increased possibility of reaching the clinical threshold for serious psychological distress (Rastogi et al., 2023). In our study, we found that HSB significantly decreased the emotional domain in post-COVID-19 patients (P < 0.05), whereas the STD group exhibited no significant alteration. In addition, the PSQI results displayed that HSB significantly improved sleep quality, reduced sleep latency, prolonged sleep duration, and minimized sleep disturbance. While there was a notable increase in the total PSQI score, this difference did not reach statistical significance when compared to the STD group. This finding aligned with the earlier research which found that warm steam inhalation could shorten deep non-REM (NREM) sleep latency and increased the sleep electroencephalograms delta power value (Ichiba et al., 2019). Furthermore, another heat-based therapies such as sauna bathing could enhance sleep and modulate immune function as well as provide physical and psychological relief (Cohen, 2020). Together with those previous findings, our present findings indicated the notion that HSB could improve sleep quality and induce psychological relaxation in post-COVID-19 patients. The potential mechanism by which HSB improves sleep quality likely arises from its primary constituents, especially the volatile oils, with Zingiber cassumunar Roxb. playing a notable role due to its recognized sedative effects. This plant contains bioactive compounds, including sabinene and terpenoids, known for their ability to induce relaxation and promote sleep (Deng et al., 2022). Previous research indicates that these compounds can modulate neurotransmitter levels, particularly serotonin (5-HT) and gamma-aminobutyric acid (GABA), which are essential for sleep regulation and enhancement, leading to improved sleep quality and reduced insomnia symptoms (Li et al., 2024). This neurotransmitter modulation presents a promising natural approach for managing sleep disorders using plant-based solutions (Ko et al., 2021).
Since this is the first randomized controlled trial on the effects of HSB in post-COVID-19 patients, there were some limitations to this study. Firstly, external factors such as lifestyle habits, including diet, physical activity, and the use of sleep aids, were not strictly controlled, which may have influenced the sleep quality outcomes. Future studies should incorporate methods to monitor adherence and control for these variables to better isolate the effects of HSB therapy. Additionally, inflammatory markers associated with neuroinflammation, such as IL-10 and TNF-α, which are involved in the body’s response to stress and play a role in sleep regulation (Krueger, 2008; Zielinski and Gibbons, 2022; Herrero Babiloni et al., 2023), must be investigated. Finally, we encourage that future studies use randomized controlled trial with a longer length of treatment (3 months) to provide explicit results.
CONCLUSIONS
In conclusion, HSB might be beneficial in reducing distress, improving sleep quality, and consequently enhancing the quality of life among post-COVID-19 patients. Therefore, health-care facilities are encouraged to endorse HSB as an alternative method to enhance sleep quality and alleviate distress among post-COVID-19 patients.
ACKNOWLEDGEMENTS
The authors express their gratitude to the Department of Integrative Medicine, Chulabhorn International College of Medicine, Thammasat University (Rangsit Campus) for providing the necessary instruments. Additionally, we acknowledge the Department of Thai Traditional and Alternative Medicine, Ministry of Public Health for providing the venue for this study. We also extend our heartfelt thanks to all the participants who took part in this study.
AUTHOR CONTRIBUTIONS
Rossarin Paithoon assisted in conducting the experiments, performed the statistical analysis, and created the data visualizations. Kusuma Sriyakul and Parunkul Tungsukruthai designed and conducted all the experiments. Nunthiya Srikaew designed the experiments. Pornchai Sawangwong provided the venue for the research. Sucharat Tungsukruthai verified the data and edited the manuscript. Pratya Phetkate was responsible for all aspects of the study, including study design, conducting the experiments, performing the statistical analysis and data visualization, and writing and editing the final manuscript. All authors have read and approved the final manuscript.
CONFLICT OF INTEREST
The authors declare that there are no economic, personal, or any other types of conflicts of interest that could have influenced the presented work.
REFERENCES
Ali, B., Al-Wabel, N. A., Shams, S., Ahamad, A., Khan, S. A., and Anwar, F. 2015. Essential oils used in aromatherapy: A systemic review. Asian Pacific Journal of Tropical Biomedicine. 5(8): 601-611.
Chandan, J. S., Brown, K. R., Simms-Williams, N., Bashir, N. Z., Camaradou, J., Heining, D., Turner, G. M., Rivera, S. C., Hotham, R., Minhas, S., et al. 2023. Non-pharmacological therapies for post-viral syndromes, including long COVID: A systematic review. International Journal of Environmental Research and Public Health. 20(4): 3477.
Charoenporn, V., Tungsukruthai, P., Charernboon, T., Sriyakul, K., Sukprasert, S., and Kamalashiran, C. 2024. Fatigue and neuropsychiatric manifestations of post-acute sequelae of COVID-19 (PASC): Examining the relationship with clinical and inflammatory markers. Fatigue: Biomedicine, Health & Behavior. 12(1): 14-31.
Cohen, M. 2020. Turning up the heat on COVID-19: Heat as a therapeutic intervention. F1000Research. 9: 292.
Deng, M., Yun, X., Ren, S., Qing, Z., and Luo, F. 2022. Plants of the genus Zingiber: A review of their ethnomedicine, phytochemistry and pharmacology. Molecules. 27(9): 2826.
DeSalvo, K., Hughes, B., Bassett, M., Benjamin, G., Fraser, M., Galea, S., and Gracia, J. N. 2021. Public health COVID-19 impact assessment: Lessons learned and compelling needs. National Academy of Medicine Perspectives. 2021: 10.31478/202104c.
Elsebai, M. F., and Albalawi, M. A. 2022. Essential oils and COVID-19. Molecules. 27(22): 7893.
Fernandez-de-Las-Peñas, C., Notarte, K. I., Macasaet, R., Velasco, J. V., Catahay, J. A., Ver, A. T., Chung, W., Valera-Calero, J. A., and Navarro-Santana, M. 2024. Persistence of post-COVID symptoms in the general population two years after SARS-CoV-2 infection: A systematic review and meta-analysis. Journal of Infection. 88(2): 77-88.
Filip, R., Gheorghita Puscaselu, R., Anchidin-Norocel, L., Dimian, M., and Savage, W. K. 2022. Global challenges to public health care systems during the COVID-19 pandemic: A review of pandemic measures and problems. Journal of Personalized Medicine. 12(8): 1295.
He, X., Chen, H., Zhu, X., and Gao, W. 2024. Non-pharmaceutical interventions in containing COVID-19 pandemic after the roll-out of coronavirus vaccines: A systematic review. BMC Public Health. 24(1): 1524.
Herrero Babiloni, A., Baril, A. A., Charlebois-Plante, C., Jodoin, M., Sanchez, E., De Baets, L., Arbour, C., Lavigne, G. J., Gosselin, N., and De Beaumont, L. 2023. The putative role of neuroinflammation in the interaction between traumatic brain injuries, sleep, pain and other neuropsychiatric outcomes: A state-of-the-art review. Journal of Clinical Medicine. 12(5): 1793.
Huerne, K., Filion, K. B., Grad, R., Ernst, P., Gershon, A. S., and Eisenberg, M. J. 2023. Epidemiological and clinical perspectives of long COVID syndrome. American Journal of Medicine Open. 9: 100033.
Ichiba, T., Kakiuchi, K., Suzuki, M., and Uchiyama, M. 2019. Warm steam inhalation before bedtime improved sleep quality in adult men. Evidence-Based Complementary and Alternative Medicine. 2019: 2453483.
Javed, B., Sarwer, A., Soto, E. B., and Mashwani, Z. U. 2020. The coronavirus (COVID-19) pandemic's impact on mental health. The International Journal of Health Planning and Management. 35(5): 993-996.
Jazieh, A. R. and Kozlakidis, Z. 2020. Healthcare transformation in the post-coronavirus pandemic era. Frontiers in Medicine. 7: 429.
Ko, L. W., Su, C. H., Yang, M. H., Liu, S. Y., and Su, T. P. 2021. A pilot study on essential oil aroma stimulation for enhancing slow-wave EEG in sleeping brain. Scientific Reports. 11(1): 1078.
Krueger, J. M. 2008. The role of cytokines in sleep regulation. Current Pharmaceutical Design. 14(32): 3408-3416.
Kumar, B. D., Verma, S. K., Chaurasia, A., and Dubey, D. 2022. Data on steam inhalation in combating Covid-19. Bioinformation. 18(9): 825-830.
Li, X., He, C., Shen, M., Wang, M., Zhou, J., Chen, D., Zhang, T., and Pu, Y. 2024. Effects of aqueous extracts and volatile oils prepared from Huaxiang Anshen decoction on p-chlorophenylalanine-induced insomnia mice. Journal of Ethnopharmacology. 319(Pt 3): 117331.
Malik, P., Patel, K., Pinto, C., Jaiswal, R., Tirupathi, R., Pillai, S., and Patel, U. 2022. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-A systematic review and meta-analysis. Journal of Medical Virology. 94(1): 253-262.
Marwah, A. K. and Marwah, P. 2020. Coronavirus (COVID-19): A protocol for prevention, treatment and control. Journal of Applied and Natural Science. 12(2): 119-123.
Moreno, C. R. C., Conway, S. G., Assis, M., Genta, P. R., Pachito, D. V., Tavares, A., Jr., Sguillar, D. A., Moreira, G., Drager, L. F., and Bacelar, A. 2022. COVID-19 pandemic is associated with increased sleep disturbances and mental health symptoms but not help-seeking: A cross-sectional nation-wide study. Sleep Science. 15(1): 1-7.
Nootim, P., Sittikraipong, K., and Tungsukruthai, P. 2019. Efficacy of herbal steam bath in reducing muscle pain: A randomized controlled trial. Journal of Health Science. 28(S2): S101-112.
Parotto, M., Gyöngyösi, M., Howe, K., Myatra, S. N., Ranzani, O., Shankar-Hari, M., and Herridge, M. S. 2023. Post-acute sequelae of COVID-19: Understanding and addressing the burden of multisystem manifestations. The Lancet Respiratory Medicine. 11(8): 739-754.
Pei, Y., Li, Y., Wu, L., Xi, J., and Zhou, N. 2024. Psychological distress during the COVID-19 pandemic normalization phase in China: A multigroup latent profile analysis among healthcare workers and the general population. International Journal of Disaster Risk Reduction. 108: 104567.
Peter, R. S., Nieters, A., Kräusslich, H.-G., Brockmann, S. O., Göpel, S., Kindle, G., Merle, U., Steinacker, J. M., Rothenbacher, D., and Kern, W. V. 2022. Post-acute sequelae of covid-19 six to 12 months after infection: Population based study. British Medical Journal. 379: e071050.
Rastogi, R., Cerda, I. H., Ibrahim, A., Chen, J. A., Stevens, C., and Liu, C. H. 2023. Long COVID and psychological distress in young adults: Potential protective effect of a prior mental health diagnosis. Journal of Affective Disorders. 340: 639-648.
Semyachkina-Glushkovskaya, O., Mamedova, A., Vinnik, V., Klimova, M., Saranceva, E., Ageev, V., Yu, T., Zhu, D., Penzel, T., and Kurths, J. 2021. Brain mechanisms of COVID-19-sleep disorders. International Journal of Molecular Sciences. 22(13): 6917.
Shaik, L., Boike, S., Ramar, K., Subramanian, S., and Surani, S. 2023. COVID-19 and sleep disturbances: A literature review of clinical evidence. Medicina. 59(5): 818.
Thaikruea, L., Srikitjakarn, L., Chakpitak, N., Pornprasert, S., Ouncharoen, R., Khamduang, W., Kaewpinta, B., Pattamakaew, S., Laiya, E., Chanaim, S., and Wongyai, J. 2022. Model of COVID-19 surveillance system for a community-industry setting. Chiang Mai University Journal of Natural Sciences. 21(1): e202206.
Thairatnopas, V., Morsup, T., Akkarapitakpong, B., and Khumsunthorn, S. 2023. The effects of using innovative herbal steam boilers on the health and comfort of patients with COVID-19. NU Journal of Nursing and Health Sciences. 18(1): 102-113.
Tungsukruthai, P., Nootim, P., Worakunphanich, W., and Tabtong, N. 2018. Efficacy and safety of herbal steam bath in allergic rhinitis: A randomized controlled trial. Journal of Integrative Medicine. 16(1): 39-44.
Wattanakittikul, J., Somchat, K., Meechai, T., Rattanawongsamethakul, D., Boonleang, V., Vannabhum, M., Suwanatrai, S., and Akarasereenont, P. 2022. Guideline practice of Thai traditional medicine treatment for prevention and reducing risk from COVID-19 transmission. Siriraj Medical Bulletin. 15(2): 93-99.
Yong, S. J. 2021. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infectious Diseases. 53(10): 737-754.
Zielinski, M. R. and Gibbons, A. J. 2022. Neuroinflammation, sleep, and circadian rhythms. Frontiers in Cellular and Infection Microbiology. 12: 853096.
OPEN access freely available online
Natural and Life Sciences Communications
Chiang Mai University, Thailand. https://cmuj.cmu.ac.th
Rossarin Paithoon1, Kusuma Sriyakul1, Parunkul Tungsukruthai1, Nunthiya Srikaew1, Pornchai Sawangwong2, Sucharat Tungsukruthai3, and Pratya Phetkate1, *
1 Department of Integrative Medicine, Chulabhorn International College of Medicine, Thammasat University (Rangsit Campus), Pathum Thani 12120, Thailand.
2 Department of Thai Traditional and Alternative Medicine, Ministry of Public Health, Nonthaburi 11000, Thailand.
3 Division of Health and Applied Sciences, Faculty of Science, Prince of Songkla University, Hat Yai, Songkhla 90110, Thailand.
Corresponding author: Pratya Phetkate, E-mail: pratya@tu.ac.th
ORCID:
Rossarin Paithoon: https://orcid.org/0009-0009-6446-2590
Kusuma Sriyakul: https://orcid.org/0000-0002-2245-9336
Parunkul Tungsukruthai: https://orcid.org/0000-0002-0536-8002
Nunthiya Srikaew: https://orcid.org/0000-0001-9982-2781
Pornchai Sawangwong: https://orcid.org/0009-0007-5125-0615
Sucharat Tungsukruthai: https://orcid.org/0000-0002-3843-706X
Pratya Phetkate: https://orcid.org/0000-0001-8906-9968
Total Article Views
Editor: Areewan Klunklin,
Chiang Mai University, Thailand
Article history:
Received: August 5, 2024;
Revised: November 9, 2024;
Accepted: November 12, 2024;
Online First: November 22, 2024

