
Use of Routine Dual-Energy X-Ray Absorptiometry-Based Bone Mineral Density Measurement in Individuals with Self-Reported Falls within 1 Year as a Warning Sign of Sarcopenia Assessment
Alisara Wongsuttilert, Sirirat Kiatkulanusorn, Wanlop Jaidee, and Pitagorn Thamronglaohaphan*Published Date : September 17, 2024
DOI : https://doi.org/10.12982/NLSC.2024.062
Journal Issues : Number 4, October-December 2024
Abstract This study evaluated the association between self-reported falls within 1 year and fragility fracture among patients who underwent dual-energy X-ray absorptiometry (DXA)-based bone mineral density (BMD) measurement.
This retrospective cross-sectional analytic study included 1,283 women and men aged 40–90 years who underwent BMD measurement using DXA. The variables assesses were age, sex, body mass index, self-reported falls within 1 year, fragility fractures and bone site, parental hip fracture, current history of daily smoking and daily excess alcohol consumption, long-term steroid use, rheumatoid arthritis, secondary osteoporosis, BMD and BMD T-scores of the lumbar spine and hip, vertebral fracture assessment results, and diagnostic classifications of osteoporosis. The participants were divided into the faller group (those with at least one fall incident within 1 year) and the non-faller group.
Overall, 375 (29.2%) patients reported history of falls within 1 year. A previous history of hip fracture (aOR = 7.674, 95% CI: 3.96– 14.86, P = 0.000), previous non-vertebral fracture (aOR = 6.305, 95% CI: 3.41–11.66, P = 0.000), previous vertebral fracture (aOR = 2.466, 95% CI: 1.61–3.78, P = 0.000), and parental hip fracture (aOR = 2.354, 95% CI: 1.46–3.80, P = 0.000) was associated with self-reported falls within 1 year.
In conclusion, self-reported falls within 1 year were strongly associated with fragility fracture. The simultaneous testing of DXA- based appendicular skeletal mass and hand grip strength is recommended for diagnosing coincident sarcopenia on routine DXA- based BMD measurement.
Keywords: Dual-energy X-ray absorptiometry, Falls, Fragility fractures, Sarcopenia, Assessment, Mineral density measurement
Funding: The authors received research funding from the Faculty of Medicine, Burapha University, Chonburi, Thailand.
Citation: Wongsuttilert, A., Kiatkulanusorn, S., Jaidee, W., and Thamronglaohaphan, P. 2024. Use of routine dual-energy x-ray absorptiometry-based bone mineral density measurement in individuals with self-reported falls within 1 year as a warning sign of sarcopenia assessment. Natural and Life Sciences Communications. 23(4): e2024062.
INTRODUCTION
Fragility fracture can result in disability, dependency, reduced quality of life, and increased public health costs (Alarkawi et al., 2020). Further, it is associated with a high mortality rate (Johnell et al., 2004). Therefore, several studies have evaluated the risk factors of initial or repeated fragility fractures within 2 years. In addition to advanced age, osteoporosis, low bone mineral density (BMD), previous history of fractures, low physical activities, high comorbidities, and a history of falls within 1 year were also related to fragility fractures (Adachi et al., 2019; Iconaru et al., 2019,2022; Afrin et al., 2020; Sujic et al., 2022).
The risk factors of falls were categorized as biological, behavioral, environmental, and socioeconomic (World Health Organization, 2008). Elderly individuals frequently experience falls. However, a recent study found that falls also often occur in the middle-aged population (aged ≥40 years) (Peeters et al., 2018). The incidence rates of fragility fractures in the middle-aged population were 12% in women and 6.7% in men (Holmberg et al., 2006). Sarcopenia is a significant potentially modifiable biological factor of falls (Yeung et al., 2019). Sarcopenia is defined as age-related loss of appendicular skeletal mass (ASM), with low muscle strength and/or diminished physical performance (Chen et al., 2020), and osteosarcopenia is described as a subset of older persons affected by osteoporosis and sarcopenia (Hirschfeld et al., 2017), which demonstrates a strong bidirectional relationship between them. Osteosarcopenic older adults also presents significantly higher risk of falls (odds ratios (OR): 2.83–3.63; P < 0.05) and fractures (OR: 3.86–4.38; P < 0.05) when compared to nonosteosarcopenic individuals (Kirk et al., 2020).
In clinical settings, the detection of sarcopenia can be effectively integrated into osteoporosis investigations via dual-energy X-ray absorptiometry (DXA) (Figure 1). Recurrent falls increased fragility fracture (Adachi et al., 2019; Iconaru et al., 2019; Sujic et al., 2022) and mortality (Kanis et al., 2023). Previous studies have revealed a significant association between DXA-measured BMD and falls, with nearly 28% of participants reporting a history of fall within 1 year and 10.9% experiencing recurrent falls (Berry et al., 2014). Despite this notion, clinicians often underutilize DXA-based body composition assessments for diagnosing sarcopenia. Although additional testing of sarcopenia increases cost (approximately $27.85 USD), early diagnosis gives patients the opportunity to receive comprehensive treatment and reduces risk of future falls and fractures (Kirk et al., 2020).
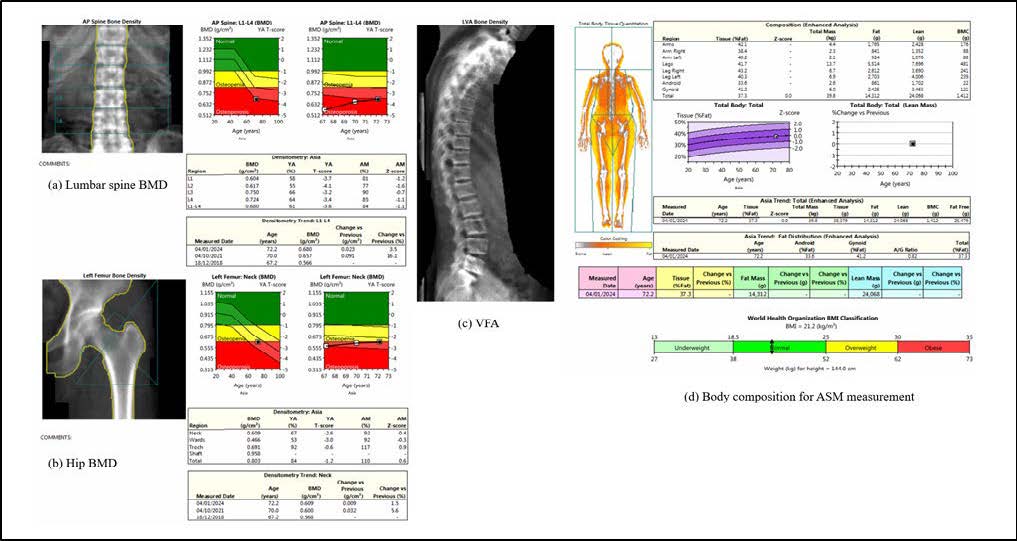
Figure 1. Images of the simultaneous measurements of DXA-based BMD and ASM. Abbreviations: ASM = appendicular skeletal mass; BMD = bone mineral density; DXA= dual-energy X-ray absorptiometry; VFA = vertebral fracture assessment.
To address clinical gap and potentially enhance fall risk management strategies, this study aimed to evaluate the association between self-reported falls within 1 year and fragility fracture within the last 12 months among patients who underwent BMD measurement using DXA. Moreover, we also investigated the association of self- reported falls within 1 year and DXA-based BMD T-scores of the lumbar spine (LS) and hip. Our results can help radiologists/nuclear physicians to make decisions for requesting the simultaneous assessment of DXA-based ASM and hand grip strength in patients who underwent BMD measurement and who have a fall history.
MATERIAL AND METHODS
Study design and patient enrollment
This retrospective cross-sectional study enrolled female and male patients aged 40–90 years who underwent BMD and/or ASM using DXA at Burapha University Hospital from October 2017 to April 2023. All eligible patients were included and initially underwent BMD measurement. The Institutional Review Board of Burapha University approved the study protocol (certificate number: HS013/2566(E1)).
Sample size calculation
The sample size in the simple logistic regression analysis (Hsieh et al., 1998) was calculated using the following equation:
Here, n is the required sample size, P is the rate of prior fractures (9.3%) (P = 0.093) (Afrin et al., 2020), P1–P2 is the difference in the rate of fractures between groups with a history of frequent falls within 1 year (P1 = 0.313), and a history of frequent falls is a factor that increases the risk of fracture when falling with an odds ratio (OR) of 1.45 (Afrin et al., 2020). P2 was calculated using the following equation:
P1–P2 was equal to 0.050. Using an alpha value of 5% (Z1-α/2 = 1.96) and a test power of 80% (Z1-β = 0.84), the sample size of this study was 1,283.
Outcome measures Primary outcomes
Primary outcome was fragility fractures within the last 12 months. Secondary outcome was DXA-based BMD T-scores of the LS and hip. Among all patients who underwent BMD testing, 226 patients (17.6%) had body composition measurement to assess for muscle mass. Furthermore, another secondary outcome was DXA-based ASM (Figure 1).
Definition of fragility fractures
Fragility fracture is defined as a fracture caused by low-energy trauma such as fall from standing height or less (International Osteoporosis Foundation, 2024). This study collected information about fractures of the major bones including the spine, hip, thigh, pelvis, upper arm, and radius. All fractures were radiologically confirmed or symptomatic clinical fractures.
BMD assessment
BMD assessment with DXA scan (GE Lunar Prodigy, Lunar, Madison, WI, the USA) of the LS, total hip, and femoral neck and vertebral fracture assessment (VFA) was performed. The results were analyzed in accordance with Adult Official Positions 2023 of the International Society for Clinical Densitometry (International Society for Clinical Densitometry, 2023). Osteoporosis can be diagnosed based on the criteria of the Thai Osteoporosis Foundation (TOPF) Clinical Practice Guideline 2021 (Charatcharoenwitthaya et al., 2023). Meanwhile, low bone mass can be diagnosed based on the BMD classification of the WHO (Kanis et al., 1994). The lowest BMD T-score of the LS, femoral neck, or total hip was selected for diagnosis (Kanis et al., 1994; Charatcharoenwitthaya et al., 2023). VFA was evaluated according to Genant et al. Patients with moderate or severe vertebral compression fracture with low-energy trauma based on VFA were diagnosed with fragility fractures (Genant et al., 1993).
Measurements of ASM
ASM measurement using DXA was also performed, and the results were analyzed according to the ISCD Adult Official Positions 2023. DXA-measured muscle mass was a component of sarcopenia diagnosis. We determined the relative skeletal muscle index (RSMI) as the following formula: RSMI (kg/m2) = ASM (kg) / height2 (m2). Based on the cutoffs of the RSMI according to the Asian Working Group for Sarcopenia 2019 (AWGS 2019), low muscle mass was interpreted as <7.0 kg/m2 in men and <5.4 kg/m2 in women (Chen et al., 2020).
Data collection
Before October 2017, a BMD request form was developed to systematically collect clinical data required for reporting. All clinical data were collected from the BMD technologist during BMD testing. To prevent falls, we added a fall question to the BMD request form from October 2017. The sentences were “Have you fallen in the last year?” and “If Yes, how many times of falls?”. All BMD request forms were scanned and stored in the picture archiving and communication system (PACS) of Burapha University Hospital. Then, all variables were reviewed and collected using the BMD request form, DXA images (Figure 1), and radiological report via the PACS. The variables included age, sex, body mass index (BMI), self-reported falls within 1 year, fragility fractures and bone site, parental hip fracture, current history of daily smoking, long-term steroid use, rheumatoid arthritis, secondary osteoporosis, current daily excess alcohol consumption, BMD and BMD T-scores of the LS and hip, VFA results, and diagnostic classifications of osteoporosis. The participants were divided into the faller group (those with at least one fall incident within 1 year) and the non-faller group (those without a history of fall incident).
Statistical analyses
The baseline and clinical variables between the faller and non-faller groups were compared. The independent t-test was used to assess continuous variables with a normal distribution. Meanwhile, the Mann–Whitney U test was applied to evaluate continuous variables with a non-normal distribution. The chi-square test was utilized to evaluate categorical variables with an expected count of ≥ 5, and the Fisher’s exact was used to examine categorical variables with an expected count of < 5. Univariate and multivariate logistic regression analyses were performed to investigate the association between self-reported falls within 1 year and fragility fracture, and BMD T-scores. The associations were presented as OR and 95% confidence intervals (CI). A P-value of < 0.05 in the multivariate analysis indicated statistically significant associations. All analyses were performed using Minitab (R) Statistics Software 20.2.0.0.
RESULTS
Of the 1,283 patients, 29.2% (n = 375) have fallen within 1 year. The faller group was older than the non-faller group (mean age: 69.6 vs. 66.3 years, P < 0.001). The faller group was more likely to have had a parent who had hip fracture (12.0% vs. 7.4%, P = 0.008), previous history of fragility fracture (48.0% vs. 16.5%, P < 0.001), and osteoporosis at hip (26.9% vs. 12.0%, P < 0.001) than the non-faller group (Table 1).
Table 1. Characteristics of patients with and without falls within 1 year (n = 1,283).
|
Variables |
Faller group (n = 375) |
Non-faller group (n = 908) |
P-value |
|
Age (years) (SD) |
69.6 (9.4) |
66.3 (8.3) |
<0.001* |
|
Male sex (%) |
44 (11.7) |
117 (12.9) |
0.571 |
|
BMI (kg/m2) (SD) |
24.1 (4.1) |
24.4 (4.0) |
0.379 |
|
Parental hip fracture (%) |
45 (12.0) |
67 (7.4) |
0.008* |
|
Current daily smoking (%) |
4 (1.1) |
5 (0.6) |
0.314 |
|
Long-term steroid use (%) |
7 (1.9) |
18 (2.0) |
0.892 |
|
Rheumatoid arthritisb (%) |
1 (0.3) |
16 (1.8) |
0.032* |
|
Secondary osteoporosis (%) |
62 (16.5) |
190 (20.9) |
0.072 |
|
Current daily excess alcohol consumptionb (%) |
2 (0.5) |
7 (0.8) |
0.643 |
|
Fragility fracture (%) |
180 (48.0) |
150 (16.5) |
<0.001* |
|
Frequency of fracturec (SD) |
1.4 (1.0) |
1.4 (1.0) |
0.865 |
|
>1 site (%) |
49 (13.1) |
39 (4.3) |
<0.001* |
|
Vertebral (%) |
101 (26.9) |
113 (12.4) |
<0.001* |
|
Hip (%) |
55 (14.7) |
19 (2.1) |
<0.001* |
|
Non-vertebral (%) |
45 (12.0) |
24 (2.6) |
<0.001* |
|
LS BMD exclusion (%) |
83 (22.1) |
124 (13.7) |
<0.001* |
|
BMD T-score (Q1, Q3) |
|||
|
Lumbar spinea |
−2.0 (−2.9, −1.0) |
−1.6 (−2.3, −0.4) |
<0.001* |
|
Femoral neck |
−1.7 (−2.4, −1.0) |
−1.3 (−1.9, −0.5) |
<0.001* |
|
Total hip |
−1.3 (−2.2, −0.6) |
−1.0 (−1.7, −0.2) |
<0.001* |
|
Spine BMD T-scorea (%) |
|||
|
Osteoporosis |
113 (38.7) |
169 (21.6) |
<0.001* |
|
Low bone mass |
96 (32.9) |
328 (41.8) |
0.007* |
|
Hip BMD T-score (%) |
|||
|
Osteoporosis |
101 (26.9) |
109 (12.0) |
<0.001* |
|
Low bone mass |
174 (46.4) |
444 (48.9) |
0.415 |
Note: *P < 0.05 represents significant differences. an = 1,076 (participants with severe degenerative spine disease and/or multi-level vertebral compression fractures on DXA images of the lumbar spine were excluded); bFisher’s exact test; cMann–Whitney U test.
Association between self-reported falls within 1 year and fragility fracture and BMD T-scores
Table 2 shows that self-reported falls within 1 year were associated with parental hip fracture (adjusted OR [aOR] = 2.354, 95% confidence interval CI: 1.46–3.80, P = 0.000), previous vertebral fracture (aOR = 2.466, 95% CI: 1.61–3.78, P = 0.000), previous hip fracture (aOR = 7.674, 95% CI: 3.96–14.86, P = 0.000), and previous non-vertebral fracture (aOR: = 6.305, 95% CI: 3.41–11.66, P = 0.000). However, self-reported falls within 1 year were not associated with LS and hip BMD T-scores.
Table 2. Univariate and multivariate logistic regression analyses were performed to investigate the association between self-reported falls within 1 year and fragility fracture, and BMD T-scores (n = 1,283).
|
Variables |
Crude OR (95% CI) |
P-value |
Adjusted ORb (95% CI) |
P-value |
|
Age (years) (SD) |
1.040 |
0.000 |
1.017 |
0.084 |
|
Parental hip fracture (%) |
(1.030–1.060) |
0.010 |
(1.000–1.040) |
0.000* |
|
Current daily smoking (%) |
1.710 |
0.320 |
2.354 |
0.139 |
|
Vertebral fracture (%) |
(1.150–2.550) |
0.000 |
(1.460–3.800) |
0.000* |
|
Hip fracture (%) |
1.950 |
0.000 |
4.909 |
0.000* |
|
Non-vertebral fracture (%) |
(0.520–7.290) |
0.000 |
(0.600–40.350) |
0.000* |
|
Spine BMD T-scorea (%) |
2.590 |
|
2.466 |
|
|
Osteoporosis |
(1.920–3.510) |
0.000 |
(1.610–3.780) |
0.141 |
|
Low bone mass |
8.040 |
0.010 |
7.674 |
0.205 |
|
Hip BMD T-scores (%) |
(4.700–13.760) |
|
(3.960–14.860) |
|
|
Osteoporosis |
5.020 |
0.000 |
6.305 |
0.224 |
|
Low bone mass |
(3.010–8.380) |
0.420 |
(3.410–11.660) |
0.228 |
Note: *P < 0.05 represents significant differences. an = 1,076 (participants with severe degenerative spine disease and/or multi-level vertebral compression fractures on DXA images of the lumbar spine were excluded); badjusted with age and parental hip fracture.
Subgroup analysis of patients who underwent simultaneous DXA-based BMD and ASM measurement
Table 3 shows information about 226 (17.6%) patients who underwent simultaneous BMD and ASM measurement using DXA. In this subgroup analysis, the results did not significantly differ from those in Table 1, except for a history of parental hip fracture. The faller group was more likely to have a lower skeletal muscle mass (mean RSMI: 5.9% vs. 6.3%, P =0.015) than the non-faller group.
Table 3. Characteristics of patients who underwent simultaneous DXA-based BMD and ASM measurement between the faller and non-faller groups (n = 226).
|
Variables |
Faller group (n = 57) |
Non-faller group (n = 169) |
P-value |
|
Age (years) (SD) |
68.5 (8.2) |
63.7 (7.9) |
< 0.001* |
|
Male sex (%) |
6 (10.5) |
29 (17.2) |
0.231 |
|
BMI (kg/m2) (SD) |
23.2 (4.2) |
24.1 (3.5) |
0.136 |
|
Parental hip fracture (%) |
6 (10.5) |
16 (9.5) |
0.816 |
|
Current daily smokingb (%) |
0 (0.0) |
2 (1.2) |
1.000 |
|
Long-term steroid useb (%) |
0 (0.0) |
3 (1.8) |
0.574 |
|
Rheumatoid arthritisb (%) |
0 (0.0) |
2 (1.2) |
1.000 |
|
Secondary osteoporosis (%) |
10 (17.5) |
34 (20.1) |
0.671 |
|
Current daily excess alcohol consumptionb (%) |
0 (0.0) |
1 (0.6) |
1.000 |
|
Fragility fracture |
26 (45.6) |
21 (12.4) |
< 0.001* |
|
Frequency of fracturec |
1.2 (0.4) |
1.5 (1.0) |
0.221 |
|
>1 siteb (%) |
5 (8.8) |
7 (4.1) |
0.184 |
|
Vertebral (%) |
11 (19.3) |
14 (8.3) |
0.022* |
|
Hip (%) |
6 (10.5) |
2 (1.2) |
0.001* |
|
Non-vertebralb (%) |
10 (17.5) |
7 (4.1) |
0.002* |
|
LS BMD exclusion |
15 (26.3) |
20 (11.2) |
< 0.001* |
|
BMD T-score (Q1, Q3) |
|||
|
Lumbar spinea |
−2.0 (−2.7, −0.8) |
−1.3 (−2.3, −0.3) |
0.014* |
|
Femoral neck |
−1.8 (−2.5, −1.2) |
−1.2 (−1.8, −0.3) |
< 0.001* |
|
Total hip |
−1.5 (−2.2, −0.8) |
−0.8 (−1.5 to 0.0) |
< 0.001* |
|
Spine BMD T-scorea (%) |
|||
|
Osteoporosis |
17 (37.8) |
33 (22.6) |
0.105 |
|
Low bone mass |
15 (33.3) |
52 (35.6) |
0.779 |
|
Hip BMD T-score (%) |
|||
|
Osteoporosis |
17 (29.8) |
9 (5.3) |
< 0.001* |
|
Low bone mass |
27 (47.4) |
90 (53.3) |
0.442 |
|
RSMI (kg/m2) (SD) |
5.9 (1.0) |
6.3 (1.0) |
0.015* |
|
Low muscle mass (%) |
20 (35.1%) |
46 (27.2%) |
0.259 |
Note: *P < 0.05 represents significant differences. an = 191 (participants with severe degenerative spine disease and/or multi-level vertebral compression fractures on DXA images of the lumbar spine were excluded); bFisher’s exact test; cMann–Whitney U test.
DISCUSSION
Falls are both a cause and a result of bone fractures. People who have frequent falls are at risk of bony fracture (World Health Organization, 2008). People with fragility fracture are at high risk of falling due to deficits in bone quality, physical function impairments, and biomechanical changes (Osipov and Christiansen, 2021). In Thailand, a recent study reported that the prevalence rates of osteoporosis, sarcopenia, and high fall risk in older Thai adults were 29.7%, 18.1%, and 38.5%, respectively. One-fifth (19.1%) of participants had at least 2 of 3 potential risk factors (i.e., osteoporosis, sarcopenia, and high fall risk). Moreover, 3.4% of participants had all three risk factors (Asavamongkolkul et al., 2024). Individuals with more risk factors have a higher risk of fragility fracture. In our study, one-quarter (29.2%) of patients who underwent BMD measurement using DXA reported a history of fall(s) within 1 year. Fall was strongly associated with fragility fractures of the spine (aOR = 2.466, 95% CI: 1.61–3.78, P = 0.000), hip (aOR = 7.674, 95% CI: 3.96–14.86, P = 0.000), and non-vertebral fracture (aOR = 6.305, 95% CI: 3.41–11.66, P = 0.000) (Table 2). These results were consistent with those of a previous study on patients who visited the fracture liaison service. That is, a higher incidence of falls was a significant risk factor of previous fractures among patients aged age 40 years or older (Sujic et al., 2022). Several cohort studies revealed that a history of falls, osteoporosis, fractures and advanced age were strongly associated with a risk of fragility fracture in postmenopausal women (Adachi et al., 2019; Afrin et al., 2020; Iconaru et al., 2019, 2022).
RSMI was a component of the sarcopenia diagnostic criteria (Chen et al., 2020), and sarcopenia was a potentially modifiable risk factor for falls in older people (Yeung et al., 2019). Considering the multifaceted role of the muscle, it is not only as a strength generator influencing physical performance but also an important organ involved in protein storage, glucose regulation, hormone production, and various cellular mechanisms (Kim and Choi, 2013). Ultimately, these factors affect BMD and fall susceptibility. Our study corresponds with this understanding, as the faller group exhibited a lower RSMI than the non-faller group (5.9 vs. 6.3 kg/m2, P = 0.015) in the subgroup analysis (Table 3). Then, with sarcopenia screening, clinicians can provide an appropriate fall prevention program and can reduce repeated falls among patients who have a history of falls within 1 year.
Patients with osteoporosis had a significantly lower back extensor muscle strength (Sinaki et al., 1993), balance and physical performance (Liu-Ambrose et al., 2006) than individuals with a normal BMD. Previous studies reported that a low BMD was associated with a history of fall (Möckel, 2021). In our study, the faller group had a higher prevalence of osteoporosis than the non-faller group (Table 1) even though the association was not statistically significant (Table 2).
Some patients who underwent BMD measurement via DXA had significant degenerative spine disease and/or vertebral compression fracture. Further, the faller group had a higher proportion of LS BMD exclusion than the non-faller group (22.1% vs. 13.7%, P < 0.001) (Table 1). During DXA examination, LS images must be excluded, and BMD could not be used for diagnosing osteoporosis if the LS presents with severe degenerative spine disease and/or multi-level vertebral compression fractures. However, degenerative spine (Ito et al., 2021) and vertebral compression fractures (Sinaki et al., 1993) are associated with reduced trunk muscle strength, resulting in a higher risk of falling. Then, patients with a history of fall within one year and severe degenerative and/or vertebral compression fracture were recommended to perform muscle strength tests, physical performance tests, and tests to measure ASM using either DXA or BIA for sarcopenia diagnosis.
Parental hip fracture was a clinical risk factor of FRAX tools (Kanis et al., 2018). This is because it was related to offspring hip fracture and major osteoporotic fracture, and incidences of offspring hip fracture and major osteoporotic fracture were decrease at older parental age at hip fracture (Yang et al., 2016). Interestingly, our study showed that parental hip fracture was associated with a history of falls within 1 year (aOR = 2.354, 95% CI: 1.46–3.80, P = 0.000) (Table 2). Explanation for this finding is unknown. However, familial associations with premature frailty, falls, or other comorbidities might lead to the early onset of parental hip fracture. Therefore, future investigations regarding this notion should be performed.
Our study is the first to report the strong association between self-reported falls within 1 year and fragility fracture within the last 12 months in a routine DXA-based BMD measurement. These results can guide radiologists and nuclear physicians in simultaneous assessment of DXA-based ASM and hand grip strength for early detection of osteosarcopenia.
This study had some limitations. First, it was cross-sectional in nature, and the result only showed an association between self-reported falls within 1 year and prevalence of fragility fracture. Therefore, it cannot be used to predict future fragility fracture, and further cohort studies should be conducted. Second, other factors associated with fragile fractures, such as physical activities (Adachi et al., 2019) and comorbidities (Iconaru et al., 2022), were not investigated in our study. Third, recall bias could occur in cross-sectional studies. However, we did not have an issue with missing data because all data were recorded in a routine BMD request form.
CONCLUSION
Self-reported falls within 1 year were strongly associated with fragility fracture. Hence, the simultaneous testing of DXA-based ASM and hand grip strength is recommended for patients who underwent BMD measurement using DXA and those who had a history of falls within 1 year, when available.
ACKNOWLEDGEMENTS
The authors greatly appreciate the Faculty of Medicine, Burapha University, Chonburi, Thailand, for providing support for this study.
AUTHOR CONTRIBUTIONS
Study protocol development: Alisara Wongsuttilert, Pitagorn Thamronglaohaphan Data collection and data management: Alisara Wongsuttilert
Data analysis: Wanlop Jaidee, Alisara Wongsuttilert
Manuscript writing: Alisara Wongsuttilert, Pitagorn Thamronglaohaphan
Final manuscript review and approval: Alisara Wongsuttilert, Sirirat Kiatkulanusorn, Wanlop Jaidee, and Pitagorn Thamronglaohaphan
CONFLICT OF INTEREST
The authors declare that they hold no competing interests.
REFERENCES
Adachi, J.D., Berger, C., Barron, R., Weycker, D., Anastassiades, T.P., Davison, K.S., Hanley, D.A., Ioannidis, G., Jackson, S.A., Josse, R.G., et al. 2019. Predictors of imminent non-vertebral fracture in elderly women with osteoporosis, low bone mass, or a history of fracture, based on data from the population-based Canadian Multicentre Osteoporosis Study (CaMos). Archives of Osteoporosis. 14(1): 53.
Afrin, N., Sund, R., Honkanen, R., Koivumaa-Honkanen, H., Rikkonen, T., Williams, L., and Kröger, H. 2020. A fall in the previous 12 months predicts fracture in the subsequent 5 years in postmenopausal women. Osteoporosis International. 31(5): 839-847.
Alarkawi, D., Bliuc, D., Tran, T., Ahmed, L.A., Emaus, N., Bjørnerem, A., Jørgensen, L., Christoffersen, T., Eisman, J.A., et al. 2020. Impact of osteoporotic fracture type and subsequent fracture on mortality: The Tromsø study. Osteoporosis International. 31(1): 119-130.
Asavamongkolkul, A., Adulkasem, N., Chotiyarnwong, P., Vanitcharoenkul, E., Chandhanayingyong, C., Laohaprasitiporn, P., Soparat, K., and Unnanuntana, A. 2024. Prevalence of osteoporosis, sarcopenia, and high falls risk in healthy community-dwelling Thai older adults: A nationwide cross-sectional study. Journal of Bone and Mineral Research Plus. 8(2): ziad020.
Berry, S.D., McLean, R.R., Hannan, M.T., Cupples, L.A., and Kiel, D.P. 2014. Changes in bone mineral density may predict the risk of fracture differently in older adults according to fall history. Journal of the American Geriatrics Society. 62(12): 2345–2349.
Charatcharoenwitthaya, N., Jaisamrarn, U., Songpatanasilp, T., Kuptniratsaikul, V., Unnanuntana, A., Sritara, C., Nimitphong, H., Wattanachanya, L., Chotiyarnwong, P., Amphansap, T., et al. 2023. Summary of the Thai osteoporosis foundation (TOPF) clinical practice guideline on the diagnosis and management of osteoporosis 2021. Osteoporosis and Sarcopenia. 9(2): 45-52.
Chen, L.K., Woo, J., Assantachai, P., Auyeung, T.W., Chou, M.Y., Iijima, K., Jang, H.C., Kang, L., Kim, M., Kim, S., and Kojima, T. 2020. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. Journal of the American Medical Directors Association. 21(3): 300-307.
Genant, H.K., Wu, C.Y., Van Kuijk, C., and Nevitt, M.C. 1993. Vertebral fracture assessment using a semiquantitative technique. Journal of Bone and Mineral Research. 8(9): 1137-1148.
Hirschfeld, H. P., Kinsella, R., and Duque, G. 2017. Osteosarcopenia: Where bone, muscle, and fat collide. Osteoporosis International. 28(10): 2781–2790.
Holmberg, A.H., Johnell, O., Nilsson, P.M., Nilsson, J., Berglund, G., and Åkesson, K. 2006. Risk factors for fragility fracture in middle age. A prospective population- based study of 33,000 men and women. Osteoporosis International. 17(7): 1065-1077.
Hsieh, F.Y., Bloch, D.A., and Larsen, M.D. 1998. A simple method of sample size calculation for linear and logistic regression. Statistics in Medicine. 17(14): 1623-1634.
Iconaru, L., Moreau, M., Kinnard, V., Baleanu, F., Paesmans, M., Karmali, R., Body, J.J., and Bergmann, P. 2019. Does the prediction accuracy of osteoporotic fractures by BMD and clinical risk factors vary with fracture site? Journal of Bone and Mineral Research Plus. 3(12): e10238.
Iconaru, L., Charles, A., Baleanu, F., Surquin, M., Benoit, F., Mugisha, A., Moreau, M., Paesmans, M., Karmali, R., Rubinstein, M., et al. 2022. Prediction of an imminent fracture after an index fracture - models derived from the Frisbee cohort. Journal of Bone and Mineral Research. 37(1): 59-67.
International Osteoporosis Foundation. 2024. Fragility fractures. Retrieved 26 February 2024 from HYPERLINK "https://www.osteoporosis.foundation/Health-%20professionals/fragility-fractures" https://www.osteoporosis.foundation/health-professionals/fragility-fractures.
International Society for Clinical Densitometry. 2023. Adult official positions of the ISCD as updated in 2023. Retrieved 24 August 2023 fromhttps://iscd.org/official-positions-2023/.
Ito, T., Sakai, Y., Sugiura, H., Kawai, K., Morita, Y., and Yamazaki, K. 2021. Association between trunk muscle strength and fall risk in older men and women with lumbar spondylosis. Healthcare (Basel). 9(5): 521.
Johnell, O., Kanis, J.A., Oden, A., Sernbo, I., Redlund-Johnell, I., Petterson, C., De Laet, C., and Jönsson, B. 2004. Mortality after osteoporotic fractures. Osteoporosis International. 15(1): 38-42.
Kanis, J.A., Melton, L.J. 3rd, Christiansen, C., Johnston, C.C., and Khaltaev, N. 1994. The diagnosis of osteoporosis. Journal of Bone and Mineral Research. 9(8): 1137-1141.
Kanis, J.A., Johansson, H., Harvey, N.C., and McCloskey, E.V. 2018. A brief history of FRAX. Archives of Osteoporosis, 13(1): 118.
Kanis, J. A., Johansson, H., Harvey, N. C., Lorentzon, M., Liu, E., Vandenput, L., Morin, S., Leslie, W. D., and McCloskey, E. V. 2023. Adjusting conventional FRAX estimates of fracture probability according to the number of prior falls in the preceding year. Osteoporosis International. 34(3): 479–487.
Kim, T.N., and Choi, K.M. 2013. Sarcopenia: Definition, epidemiology, and pathophysiology. Journal of Bone Metabolism. 20(1): 1-10.
Kirk, B., Zanker, J., and Duque, G. 2020. Osteosarcopenia: Epidemiology, diagnosis, and treatment-facts and numbers. Journal of Cachexia, Sarcopenia and Muscle. 11(3): 609–618.
Liu-Ambrose, T., Khan, K.M., Donaldson, M.G., Eng, J.J., Lord, S.R., and McKay, H.A. 2006. Falls-related self-efficacy is independently associated with balance and mobility in older women with low bone mass. The Journals of GErontology. Series A, Biological Sciences and Medical Sciences. 61(8): 832-838.
Möckel, L. 2021. Risk of falls in patients with low bone mineral density: Analysis of placebo arms from clinical trials. Zeitschrift für Gerontologie und Geriatrie. 54(6): 576-581.
Osipov, B. and Christiansen, B.A. 2021. Mechanisms for increased systemic fracture risk after index fracture. Medicine in Novel Technology and Devices. 11: 100072.
Peeters, G., van Schoor, N.M., Cooper, R., Tooth, L., and Kenny, R.A. 2018. Should prevention of falls start earlier? Co-ordinated analyses of harmonized data on falls in middle-aged adults across four population-based cohort studies. PLoS One. 13(8): e0201989.
Sinaki, M., Khosla, S., Limburg, P.J., Rogers, J.W., and Murtaugh, P.A. 1993. Muscle strengthin osteoporotic versus normal women. Osteoporosis International. 3(1): 8–12.
Sujic, R., Yang, A., Ansari, H., Bogoch, E.R., Jain, R., Weldon, J., Elliot-Gibson, V., and Sale, J.E.M. 2022. Fragility fracture patients with history of prior fractures more likely to present with multiple risk factor: Findings from a province-wide fracture liaison service. Osteoporosis International. 33(8): 1769-1774.
World Health Organization. 2008. WHO global report on falls prevention in older age. Geneva: World Health Organization. Retrieved 15 January 2023 from https://www.who.int/publications/i/item/9789241563536.
Yang, S., Leslie, W.D., Yan, L., Walld, R., Roos, L.L., Morin, S.N., Majumdar, S.R., and Lix, L.M. 2016. Objectively verified parental hip fracture is an independent risk factor for fracture: A linkage analysis of 478,792 parents and 261,705 offspring. Journal of Bone and Mineral Research. 31(9): 1753-1759.
Yeung, S.S.Y., Reijnierse, E.M., Pham, V.K., Trappenburg, M.C., Lim, W.K., Meskers, C.G.M., and Maier, A.B. 2019. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta‐analysis. Journal of Cachexia, Sarcopenia and Muscle. 10(3): 485–500.
|
OPEN access freely available online Natural and Life Sciences Communications Chiang Mai University, Thailand. https://cmuj.cmu.ac.th |
Alisara Wongsuttilert1, Sirirat Kiatkulanusorn2, Wanlop Jaidee3, and Pitagorn Thamronglaohaphan1, *
1 Faculty of Medicine, Burapha University, Chonburi 20131, Thailand.
2 Faculty of Allied Health Sciences, Burapha University, Chonburi 20131, Thailand.
3 Faculty of Public Health, Burapha University, Chonburi 20131, Thailand.
Corresponding author: Pitagorn Thamronglaohaphan, E-mail: pitagorn.th@go.buu.ac.th
ORCID:
Alisara Wongsuttilert: https://orcid.org/0000-0002-0067-1045
Pitagorn Thamronglaohaphan: https://orcid.org/0009-0001-0234-3336
Total Article Views
Editor: Waraporn Boonchieng
Chiang Mai University, Thailand
Article history:
Received: June 11, 2024;
Revised: September 9, 2024;
Accepted: September 10, 2024;
Online First: September 17, 2024

