
Lateral Abdominal Muscles Thickness in Sitting and Standing Positions During Abdominal Drawing-In Maneuver and Abdominal Bracing Among Chronic Low Back Pain Individuals
Aisha Tukur Mohammed, Patraporn Sitilertpisan, Sompong Sriburee, Chich-Haung Richard Yang, and Aatit Paungmali*Published Date : August 23, 2024
DOI : https://doi.org/10.12982/NLSC.2024.054
Journal Issues : Number 4, October-December 2024
Abstract Low back pain (LBP) is a general problem that influences most working populations throughout their lifetime. Spinal stabilization exercises, such as abdominal drawing maneuver (ADIM) and abdominal bracing (AB) are potential for the management of low back pain, especially in functional positions such as sitting and standing. This study aimed to determine the effects of testing positions (sitting, standing) and types of exercises (ADIM, AB) on muscle thickness of the lateral abdominal muscles among chronic LBP individuals. Twenty-four adults (12 males, 12 females) with chronic non-specific low back pain were assessed in sitting and standing positions while performing ADIM and AB exercises. Ultrasound imaging was used to quantify the thickness of the lateral abdominal muscles during the exercises. The Wilcoxon signed-rank test was used to compare the muscle thickness of Transversus Abdominis (TrA), Internal Oblique (IO), and External Oblique (EO) at rest, ADIM, and AB. The results showed that during ADIM, the thickness of the TrA and IO muscles increased compared to rest (P <0.05). Furthermore, TrA was thicker during ADIM than during AB exercise at both positions (P <0.05). The thickness of IO increased during AB compared to rest in both positions, but the EO muscle thickness significantly greater during ADIM compared to rest and AB in the standing position (P <0.05). In conclusion, ADIM stimulates the TrA and IO muscles, whereas AB stimulates IO in individuals with LBP. Therefore, ADIM can initially be included in exercise regimes to improve spinal stability in individuals with chronic non-specific LBP.
Keywords: Low back pain, Abdominal muscles, Abdominal drawing maneuver, Abdominal bracing, Ultrasound imaging
Funding: This work was supported by the CMU Presidential Scholarship and the Institutional Research Funding (grant number: AMS2566-06).
Citation: Mohammed, A. T., Sitilertpisan, P., Sriburee, S., Yang, C-H. R., and Paungmali, A. 2024. Lateral abdominal muscles thickness in sitting and standing positions during abdominal drawing-in maneuver and abdominal bracing among chronic low back pain individuals. Natural and Life Sciences Communications. 23(4): e2024054.
INTRODUCTION
Low back pain (LBP) is a general problem that influences most working populations throughout their lifetime. The lifetime attack rate for LBP is between 60-80% for the general population (Meucci et al., 2015). Most of the symptoms are resolved naturally in those persons affected. However, other individuals experience ongoing pain for more than 3 months and recurrences are known as chronic LBP pain (Nieminen et al., 2021). Core stability (spinal stability or stability of the trunk) is crucial for preventing and alleviating LBP. Numerous types of research have demonstrated their efficiency in reducing back pain (Hosseinifar et al., 2013). Core stability can be achieved by synchronizing the contraction of a certain set of muscles in the body, specifically the abdominal muscles in the front, the back muscles of the spine, the diaphragm, and the pelvic floor muscles (Arnold et al., 2015). The lateral abdominal muscles such as transversus abdominis (TrA), internal oblique (IO), and external oblique (EO) muscles contribute primarily to core stability during motions and weight-bearing (Ehsani et al., 2016). The TrA muscle is the inner most of the three flat abdominal muscles. It originates from the internal surfaces of the 7th to 12th costal cartilages, thoracolumbar fascia, iliac crest, and lateral third inguinal ligament, and attaches to the linea alba. Its primary role is to compress the abdominal viscera. The muscle fibers extend horizontally (Grevious et al., 2006). The IO muscle arises from the anterior part of the iliac crest, the exterior half to two-thirds of the inguinal ligament, and the back aponeurosis of the transversus abdominis muscle and it fibers flow in a superior-anterior direction perpendicular to the external oblique and attach to the cartilages of the lower four ribs while the EO muscle is considerably flat muscles that make up the abdominal wall. The muscle arises from the lower eight ribs, interlocks with slips of the latissimus dorsi and serratus anterior muscles, and runs in a downward and inward direction. It attaches centrally at the linea alba through its aponeurosis. Major nerves to the anterolateral abdominal wall include the thoracoabdominal, lateral cutaneous, subcostal, iliohypogastric, and ilioinguinal nerves (Grevious et al., 2006).
Spinal stabilization programs are potential active mode of exercises for management of LBP by promoting stability to the spinal segments (Gomes-Neto et al., 2017). Unlike the massage therapy that is a passive mode of management schemes to facilitate muscle relaxation and alleviating tension in different areas of the body, such as the lower back resulting in increased flexibility of the lower back muscles and tendons (Areewan et al., 2021). In recent years, numerous spinal stabilization exercises have been suggested for lumbo-pelvic instability and spinal pain. Thus, commonly used activities, such as the abdominal drawing-in maneuver (ADIM) and abdominal bracing (AB), are believed to activate core muscles (Teyhen et al., 2009; Hosseinifar et al., 2013). The ADIM is a popular exercise technique for the activation of TrA and multifidus muscles (Hlaing et al., 2021) while minimizing the contraction of the synergistic muscles (Internal Oblique (IO), External Oblique (EO), rectus abdominis (RA), and erector spinae). Previous studies have shown that exercises for the activation of TrA and multifidus improve trunk stability and reduce the reoccurrence of LBP (Halliday et al., 2016). Abdominal bracing, which involves consciously contracting all abdominal muscles, is an efficient technique for increasing deep abdominal muscle activation, particularly the IO (Maeo et al., 2013). Research has shown that AB is efficient at raising intra-abdominal pressure which makes it an essential exercise for trunk stability (Tayashiki et al., 2016). Rehabilitative ultrasound imaging (RUSI) is a non-invasive method to measure the changes in lateral abdominal muscle thickness during ADIM and AB. These muscle thickness alterations may indicate the level of muscle activation (Calvo-Lobo et al., 2019). Several investigations addressed the reliability and validity of RUSI for measuring various muscle geometries, and it was found to be an accurate and valid instrument (Calvo-Lobo et al., 2019). RUSI when compared to the gold standard, Magnetic Resonance Imaging (MRI) and fine wire electromyography (EMG), is relatively cheaper, easily accessible, and non-invasive, thus making it less dangerous (Whittaker et al., 2007). Although superficial EMG has been used previously to overcome the high risk of needle/fine wire EMG, it has limitations in crosstalk signaling (i.e., noise signal) of superficial muscles and cannot study the morphology of muscles (McMeeken et al., 2004; Johnson et al., 2021).
Teyhen et al. (2005) evaluated the lateral abdominal muscles during ADIM in chronic LBP individuals using ultrasound imaging (Teyhen et al., 2005). The result reported that ADIM activates the TrA muscle with minimal activation of IO and EO muscles, which can be an essential component in lumbar stabilization. However, there is limited study on activation of the lateral abdominal muscles in AB using ultrasound imaging. In sitting and supine positions, the thicknesses of TrA and IO when ADIM was performed increased significantly, while during AB, the thicknesses of TrA, IO, and EO did not increase significantly (Madokoro et al., 2020). Investigation of the thicknesses of TrA, IO, and EO when ADIM and AB are performed in a standing position is unclear. During clinical practice, initial training for contracting the lateral abdominal muscle involves exercises performed in fundamental functional positions, such as sitting and standing. Previous studies have employed many positions, including supine lying, hook lying, supine with 90° flexed knee and hip, supine with stretched knees and 90° flexed hips, and bridge position, to examine the activation of lateral abdominal muscles during the ADIM and AB exercises which show that TrA muscle had a higher activation in the bridge position (Vera-Garcia et al., 2010; Ishida et al., 2019). Recently, Mohammed et al. (2024) investigated muscle morphology of anterior and lateral abdomen during ADIM and AB in upright positions among healthy participants. They found that ADIM and AB can produce contraction of the lateral abdominal muscles in both sitting and standing positions. However, ADIM can activate TrA and IO muscles better than AB. Before transferring this knowledge to teach individuals who need core stability exercises especially for people with low back pain, we need to validate its characteristics because muscle activating patterns in LBP individuals is different from healthy people (Hodges and Danneels, 2019). Since, there is a lack of information on the impact of lateral abdominal muscles during ADIM and AB in functional weight bearing positions (sitting and standing), particularly among individuals with low back pain. So, the purpose of this study is to determine the effects of testing positions (sitting, standing) and types of exercises (ADIM, AB) on muscle thickness of the lateral abdominal muscles (i.e., TrA, IO, and EO) among non-specific chronic LBP individuals. The significance of this study is to understand certain information about core muscles (i.e., lateral abodominal muscles) and provide a recommendation for the clinicians for the appropriate exercise regimen to promote core stability in the management of LBP.
MATERIALS AND METHODS
Study design
This study is a cross-sectional design on the muscle thickness of the lateral abdominal muscles during ADIM and AB among individuals with chronic low back pain.
Ethical approval
The study was approved by the Institution Human Research Ethics Committee (AMSEC-66EX-033). The present study adhered to the ethical standards of the Declaration of Helsinki. In addition, the consent form was obtained from all subjects before data collection.
Study participants
A total sample of 25 chronic low back pain individuals (13 males and 12 females) was initially recruited through an advertising campaign. The sample size was calculated using G-power, version 3.1.9.7, with an effect size of 0.25 (based on the muscle thickness of TrA and IO muscles), a power level of 0.80, and a p-value of 0.05 (Madokoro et al., 2020). The inclusion criteria were participants from 18-45 years old with non-specific chronic LBP (previously diagnosed with the physician, pain localized below the costal margin and above the inferior gluteal folds) lasting more than three months from mild to moderate pain intensity on the numerical rating scale (3/10 – 7/10) and a normal range of BMI (18.5-24.9 kg/m2), which was measured and calculated by the researcher, were recruited into the study. The exclusion criteria include participants with a history of vertebral surgeries, any medical conditions affecting the spinal tissues, spinal pathology, neurological impairment, pregnancy, impaired standing balance or inability to stand for at least 30 seconds, or participants with stress urinary incontinence, and participants who not be able to obey instructions were excluded from the study (Figure 1). The participants who had regular core exercise or abdominal muscle training and athletes were also excluded from the study. Participants were requested not to take a heavy meal at least 2 hours before the measurement.
Measurement procedure
The main study involved measurements in standing and sitting positions, at rest, and during ADIM and AB exercises. Before data collection, familiarization sessions were conducted in sitting and standing positions. All participants underwent training in ADIM and AB exercises using a pressure biofeedback unit (PBU) at the L1-L5 level to standardize the exercises (for the upright position, a lumbar belt was wrapped around the participant's abdomen just above the anterior superior iliac spine (ASIS), and a pressure biofeedback unit was placed between trunk and lumbar belt which was inflated to 40 +/- 10 mmHg). Measurements were made only after ensuring participants had a clear understanding of the procedures.
Following the methodology of a previous study, an ultrasound transducer (Canon, model Xario – 100, Japan, linear head transducer, multifrequency 5-12 MHz) with B-mode were placed midway between the lower end of the rib cage and the upper border of the iliac crest, using the anterior midaxillary line as a reference point (Madokoro et al., 2020). The TrA, IO, and EO muscles were measured three times at their thickest portion during expiration (measuring perpendicular to the muscles’ fascia alignment), in both sitting and standing positions at rest, as well as during the ADIM and AB exercises using the ImageJ program, and the average values of the images were analyzed. During ADIM, participants were instructed to pull the navel towards the spine (i.e., pull in the belly like zip up) and hold for 10 seconds while maintaining the neutral position of the lumbopelvic region. For AB, participants were asked to contract their abdominal muscles (i.e., push the belly to tighten), while holding for 10 seconds and controlling the neutral position of the lumbopelvic region (Madokoro et al., 2020). All measurements were taken on the right side of the body and in a randomly assigned order, with a 3-second resting phase between each repetition (i.e., 3 repetitions, calculating for an average value) and a 60-second rest between each position during the procedure (Figures 1 and 2).
Statistical analysis
The data were analyzed using a statistical program SPSS (SPSS version 26.0, IBM, Armonk, NY, USA). The intra-rater reliability of muscle thickness measurement was conducted before the main data collection, and the intra-class correlation coefficient (ICC) was used to determine the acceptability of the measurement reliability. To test the normal distribution of the main data, the Shapiro-Wilk test was used. Since the data was not a normal distribution, non-parametric tests were used to analyze the data (Friedman’s Rank test with Wilcoxon Signed Rank post-hoc analysis). The level of statistical significance was set at P < 0.05.

Figure 1. Muscle thickness measurement using ultrasound imaging in sitting position.

Figure 2. Muscle thickness measurement using ultrasound imaging in standing position.
RESULTS
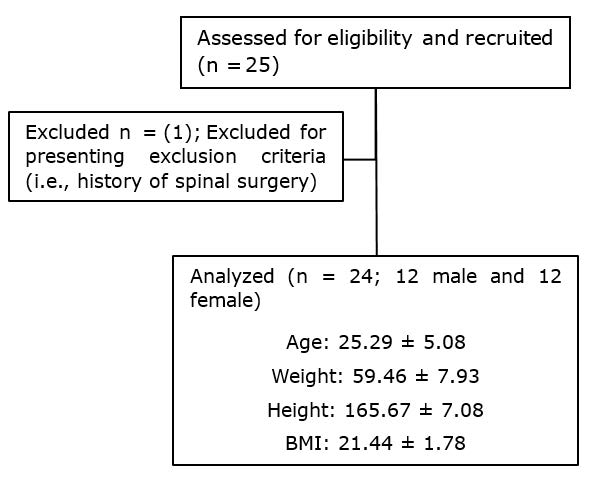
Figure 3. Flowchart for recruitment
Reliability study of the lateral abdominal muscle thickness
Table 1 shows the intraclass correlation coefficient (ICC3,1) for the intra-rater reliability for lateral abdominal muscle thickness. The measurements were higher than 0.95, indicating high reliability.
Table 1. Intra-rater reliability of lateral abdominal muscle thickness during ADIM and AB.
|
Position |
Intraclass correlation coefficients (ICC2,1) |
|||
|
|
TrA |
IO |
EO |
|
|
|
Rest |
0.975 |
0.979 |
0.988 |
|
Standing |
ADIM |
0.979 |
0.994 |
0.983 |
|
|
AB |
0.955 |
0.996 |
0.974 |
|
|
Rest |
0.972 |
0.988 |
0.961 |
|
Sitting |
ADIM |
0.988 |
0.986 |
0.979 |
|
|
AB |
0.958 |
0.988 |
0.995 |
|
|
||||
Note: Intraclass correlation coefficients for the same participants on the same day and between days; TrA: transverse abdominis, IO: internal abdominal oblique, EO: external abdominal oblique, ADIM: abdominal drawing-in maneuver, AB: abdominal bracing
Lateral abdominal muscle thickness
The thicknesses of TrA and IO increased during ADIM compared to those of rest, with TrA showing a greater during ADIM than AB in both positions. Moreover, IO thickness increased during AB compared to rest in both positions. However, the thickness of the EO experienced a significantly greater during ADIM compared to the AB in the standing position (see Tables 2 and 3 for details).
Table 2. Mean and standard deviation of lateral abdominal muscle thickness and comparison between ADIM and AB in a sitting position.
|
Muscle thickness (cm) |
Sitting |
||
|
Rest |
ADIM |
AB |
|
|
TrA |
0.39 ± 0.15 |
0.60 ± 0.18*† |
0.41 ± 0.18 |
|
IO |
0.75 ± 0.19 |
1.11 ± 0.37* |
1.07 ± 0.34# |
|
EO |
0.56 ± 0.13 |
0.53 ± 0.13 |
0.52 ± 0.20 |
|
|
|||
Note: TrA: transverse abdominis, IO: internal abdominal oblique, EO: external abdominal oblique, ADIM: abdominal drawing-in maneuver, AB: abdominal bracing, *: muscle thickness between ADIM and rest (P <0.05), #: muscle thickness between AB and rest (P <0.05), †: comparison of muscle thickness between ADIM and AB using Wilcoxon signed rank test (P <0.05)
Table 3. Mean and standard deviation of lateral abdominal muscle thickness and comparison between ADIM and AB in a standing position.
|
Muscle thickness (cm) |
Standing |
||
|
Rest |
ADIM |
AB |
|
|
TrA |
0.32 ± 0.08 |
0.51 ± 0.16*† |
0.36 ± 0.12 |
|
IO |
0.80 ± 0.22 |
1.09 ± 0.36* |
1.01 ± 0.30# |
|
EO |
0.57 ± 0.13 |
0.55 ± 0.12 |
0.47 ± 0.11#† |
|
|
|||
Note: TrA: transverse abdominis, IO: internal abdominal oblique, EO: external abdominal oblique, ADIM: abdominal drawing-in maneuver, AB: abdominal bracing, *: muscle thickness between ADIM and rest (P <0.05), #: muscle thickness between AB and rest (P <0.05), †: comparison of muscle thickness between ADIM and AB using Wilcoxon signed rank test (P <0.05)
Comparison between sitting and standing
Table 4 presents the mean and standard deviation of the thickness of TrA, IO, and EO thickness during sitting and standing positions. The findings indicate that no significant difference was observed between ADIM and AB in both positions for TrA, IO, and EO.
Table 4. Mean and standard deviation of lateral abdominal muscle thickness and comparison between ADIM and AB in standing and sitting.
|
Exercise |
Sitting |
Standing |
P-value |
||||||||
|
Mean SD |
/Mean diff./ |
Mean SD |
/Mean diff./ |
||||||||
|
TrA |
-Rest |
0.39 ± 0.15 |
|
0.32 ± 0.08 |
|
|
|||||
|
|
-ADIM |
0.60 ± 0.18 |
0.21 ± 0.13 |
0.51 ± 0.16 |
0.19 ± 0.14 |
0.166 |
|||||
|
|
-AB |
0.41 ± 0.18 |
0.02 ± 0.21 |
0.36 ± 0.12 |
0.04 ± 0.12 |
0.819 |
|||||
|
IO |
-Rest |
0.75 ± 0.19 |
|
0.80 ± 0.22 |
|
|
|||||
|
|
-ADIM |
1.11 ± 0.37 |
0.35 ± 0.25 |
1.09 ± 0.36 |
0.29 ± 0.25 |
0.224 |
|||||
|
|
-AB |
1.07 ± 0.34 |
0.32 ± 0.24 |
1.01 ± 0.30 |
0.21 ± 0.16 |
0.550 |
|||||
|
EO |
-Rest |
0.56 ± 0.13 |
|
0.57 ± 0.13 |
|
|
|||||
|
|
-ADIM |
0.53 ± 0.13 |
0.03 ± 0.14 |
0.55 ± 0.12 |
0.02 ± 0.12 |
0.775 |
|||||
|
|
-AB |
0.52 ± 0.20 |
0.04 ± 0.17 |
0.47 ± 0.11 |
0.10 ± 0.13 |
0.109 |
|||||
|
|
|||||||||||
Note: TrA: transverse abdominis, IO: internal abdominal oblique, EO: external abdominal oblique, ADIM: abdominal drawing-in maneuver, AB: abdominal bracing, Mean diff: mean difference between exercises and rest, /Mean dif./: Absolute Mean Difference.
DISCUSSION
This study investigated the thickness of the lateral abdominal muscles (TrA, IO, and EO) during ADIM and AB in sitting and standing positions. No previous study has investigated the thickness of the lateral abdominal muscle in functional positions (sitting and standing) among people with chronic LBP. From the result of this study, it was found that TrA and IO thickness increased significantly during ADIM compared to those at rest in both positions. A study by Madokoro et al. (2020) reported that a similar result was attributed to increased muscle activity of the TrA and IO. Furthermore, there was a significant increase in the thickness of TrA during ADIM than AB in both positions. Teyhen et al. (2005) reported that patients with LBP demonstrated an increase in TrA muscle activity during the ADIM in the supine position, which was similar to the results of this study. This suggests that ADIM can activate TrA muscle in this population. Several studies have also reported that IO can be activated during AB, which plays an important role in the execution of abdominal bracing exercises. (Vera-Garcia et al., 2010; Maeo et al., 2013). Maeo et al. (2013) utilized surface electromyography to investigate the activation of the rectus abdominis, EO, IO, and erector spinae muscles in a supine position during AB exercise, and confirmed that the IO muscle had higher activation than the other trunk muscles. The result agrees with the current study because, in both positions, there was a significant increase in IO thickness in the AB compared to rest in both sitting and standing positions. Previous research findings indicate that an increase in the thickness of the IO muscle may inhibit or partially cover the EO muscle, resulting in its visual reduction (Teyhen et al., 2005). Surprisingly, the EO muscle thickness significantly changed during AB compared to rest and increased in ADIM compared to AB in a standing position. The finding is novel and considerable new information among the previous studies. Possible reasons for this may be the antigravity posture and alignment of EO muscles. An EO is the superficial area of the abdominal muscles, and the muscle fibres extend down the iliac crest from the ribs and move diagonally downward and inward. So, change in the EO thickness may be influenced by the muscle fibre alignment, as well as the compression force from deep core muscle contraction during the maneuvers. Therefore, further studies may be recommended to confirm the assumption.
Comparisons between ADIM and AB in sitting and standing showed that there was no significant increase in TrA, IO, and EO. On the contrary, Madokoro et al. (2020) discovered that the IO was significantly thicker during ADIM and AB, while the EO was significantly thicker during AB only in a sitting position using real-time ultrasound imaging. This may be due to chronic LBP patients used in the current study; there might be a change in muscle characteristics of the muscles due to muscle disuse. More research is required to confirm the findings of this study.
Clinical Implications
The study findings provide information on the activity of the lateral abdominal muscles (TrA, IO, and EO) during ADIM and AB. First, this study shows that the thickness of the lateral abdominal muscles can be measured and monitored using real-time ultrasound imaging. ADIM was shown to activate TrA and IO, which can be potential components of spinal stabilization. Additionally, IO has shown a significant increase in thickness during AB, which can be considered to have a crucial role in maintaining spinal stability. The EO muscle was also found to be a significant change in the standing position, this is a new finding apart from previous studies. The findings of this study did not provide a definitive answer to the most effective position, either sitting or standing, it should also account for the individual’s LBP symptom. The subjective difficulty of verbal instruction for the stabilization exercises were also challenging in some participants, the familiarization session and using a standardized simply verbal instruction were good strategies to cope the problem. For the adverse effect, only one participant experienced pain when performing the AB exercise during the initial 1-2 attempts of the maneuver, then the pain intensity subsided. Interestingly, this study in LBP individuals did not show a significant difference between sitting and standing positions, this may be because the subject’s pain characteristic in this population was not too severe (e.g., 4.9/10 NRS), and the intensity of contraction during the maneuvers was minimal (e.g., ±10 mmHg). Future study may need to investigate these notions.
This study had several limitations which are that the additional information regarding the degree of physical activity, lifestyle, and subjective difficulty of the exercises was not monitored. Also, simple randomization happened by chance, further investigation may need to balance between ADIM and AB conditions to encounter carry-over effects by conducting the AB-BA balance randomization design. Lastly, the result of this study cannot be generalized to all age groups because only individuals with CLBP aged between 18-45 were recruited, and an exercise program with long-term follow-up is warranted for further study.
CONCLUSION
This study shows that in both functional positions (sitting and standing), the core stabilizing exercises (i.e., ADIM and AB) can activate the lateral abdominal muscles. Nonetheless, ADIM activates TrA and IO muscles, whereas AB predominately activates IO muscles. Suggests that ADIM exercise can be included in exercise regimes to maintain trunk stability in people with chronic non-specific LBP. While AB exercise may be useful in the progressive stage of core stabilizing exercise as its subjective difficulty to instruct, and it requires more level of co-contraction of trunk muscles.
ACKNOWLEDGEMENTS
The first author is a graduate student in Movement and Exercise Sciences, Faculty of Associated Medical Sciences at Chiang Mai University, Thailand, supported by the CMU Presidential Scholarship. The authors are thankful to all studied participants, the Department of Physical Therapy and the Department of Radiologic Technology at Chiang Mai University, Thailand, for providing the necessary infrastructure for this research.
AUTHOR CONTRIBUTIONS
Concept design and development: Aisha Tukur Mohammed, Patraporn Sitilertpisan, Aatit Paungmali
Data collection, analysis, and interpretation: Aisha Tukur Mohammed, Patraporn Sitilertpisan, Sompong Sriburee, Aatit Paungmali
Literature search and manuscript writing: Aisha Tukur Mohammed, Chich-Haung Richard Yang, Aatit Paungmali
Final manuscript review and approval: Aisha Tukur Mohammed, Patraporn Sitilertpisan, Sompong Sriburee, Chich-Haung Richard Yang, Aatit Paungmali.
CONFLICT OF INTEREST
The authors declared no conflict of interest.
REFERENCES
Areewan, K.A., Sansiriphun, N., Viseskul, N., Sawasdisingha, P., Sripetchwandee, N., Chaisang, S., and Prachayaporn C.P. 2021. Lanna-spa model for health in Thailand. Chiang Mai University Journal Natural Science. 20(4): 2021071.
Arnold, C., Lanovaz, J., Oates, A., Craven, B., and Butcher, S. 2015. The effect of adding core stability training to a standard balance exercise program on sit to stand performance in older adults: A pilot study. Journal of Aging and Physical Activity. 23(1): 95–102.
Calvo-Lobo, C., Almazan-Polo, J., Becerro-de-bengoa-vallejo, R., Losa-Iglesias, M.E., Palomo-Lopez, P., Rodriguez-Sanz, D., and Lopez-Lopez, D. 2019. Ultrasonography comparison of diaphragm thickness and excursion between athletes with and without lumbopelvic pain. Physical Therapy in Sport. 37:128–137.
Ehsani, F., Arab, A.M., Assadi, H., Karimi, N., and Shanbehzadeh, S. 2016. Evaluation of pelvic floor muscles activity with and without abdominal maneuvers in subjects with and without low back pain. Journal of Back and Musculoskeletal Rehabilitation. 29(2): 241–247.
Gomes-Neto, M., Lopes, J.M., Conceicao, C.S., Araujo, A., Brasileiro, A., Sousa, C., Carvalho, V.O., and Arcanjo, F.L. 2017. Stabilization exercise compared to general exercises or manual therapy for the management of low back pain: A systematic review and meta-analysis. Physical therapy in Sport. 23: 136-142.
Grevious, M. A., Cohen, M., Shah, S. R., and Rodriguez, P. 2006. Structural and functional anatomy of the abdominal wall. Clinics in Plastic Surgery. 33(2): 169–179.
Halliday, M. H., Pappas, E., Hancock, M. J., Clare, H. A., Pinto, R. Z., Robertson, G., and Ferreira, P. H. 2016. A randomized controlled trial comparing the McKenzie method to motor control exercises in people with chronic low back pain and a directional preference. Journal of Orthopaedic & Sports Physical Therapy. 46(7): 514-522.
Hlaing, S.S., Puntumetakul, R., and Khine, E.E. 2021. Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain-related outcomes in patients with subacute nonspecific low back pain: A randomized controlled trial. BMC Musculoskeletal Disorder. 22(1): 998.
Hodges, P.W. and Danneels, L. 2019. Changes in structure and function of the back muscles in low back pain: Different time points, observations, and mechanisms. Journal of Orthopaedic & Sports Physical Therapy. 49(6): 464-476.
Hosseinifar, M., Akbari, M., Behtash, H., Amiri, M., and Sarrafzadeh, J. 2013. The effects of stabilization and Mckenzie exercises on transverse abdominis and multifidus muscle thickness, pain, and disability: A randomized controlled trial in non-specific chronic low back pain. Journal of Physical Therapy Sciences. 25(12): 1541-1545.
Ishida, S.N., Furtado, R.N.V., Rosenfeld, A., Proglhof, J.E.P., Estrela, G.B.Q., and Natour, J. 2019. Ultrasound of entheses in ankylosing spondylitis patients: The importance of the calcaneal and quadriceps entheses for differentiating patients from healthy individuals. Clinics. 74: e727.
Johnson, A.W., Adams, L., Kho, J.B., Green, D.M., Pace, N.B., and Mitchell, U.H. 2021. Extended field-of-view ultrasound imaging is reliable for measuring transversus abdominis muscle size at rest and during contraction. BMC Musculoskeletal Disorders. 22: 1-10
Madokoro, S., Yokogawa, M., and Miaki, H. 2020. Effect of the abdominal draw-in maneuver and bracing on abdominal muscle thickness and the associated subjective difficulty in healthy individuals. Healthcare. 8(4): 496.
Maeo, S., Takahashi, T., Takai, Y., and Kanehisa, H. 2013. Trunk muscle activities during abdominal bracing: Comparison among muscles and exercises. Journal of Sports Sciences and Medicine. 12(3): 467-474.
Meucci, R. D., Fassa, A. G., and Faria, N. M. X. 2015. Prevalence of chronic low back pain: Systematic review. Revista de Saude Publica. 49:73.
McMeeken, J.M., Beith, I.D., Newham, D.J., Milligan, P., and Critchley, D.J. 2004. The relationship between EMG and change in thickness of transversus abdominis. Clinical Biomechanics. 19(4): 337-342.
Mohammed, A.T., Petchsont, H., Sitilertpisan, P., Sriburee, S., Joseph, L., Paungmali, A. 2024. Muscle thickness of lateral abdominal muscles in sitting and standing positions during abdominal drawing-in maneuver and abdominal bracing among healthy adults. Journal of Associated Medical Sciences, 57(3): 177-183.
Nieminen, L. K., Pyysalo, L. M., and Kankaanpää, M. J. 2021. Prognostic factors for pain chronicity in low back pain: A systematic review. Pain Reports. 6(1): 919.
Tayashiki, K., Takai, Y., Maeo, S., and Kanehisa, H. 2019. Intra-abdominal pressure and trunk muscular activities during abdominal bracing and hollowing. International Journal of Sports Medicine. 37(2): 134-143.
Teyhen, D.S., Bluemle, L.N., Dolbeer, J.A., Baker, S.E., Molloy, J.M., Whittaker, J., and Childs, J.D. 2009. Changes in lateral abdominal muscle thickness during the abdominal drawing-in maneuver in those with lumbopelvic pain. Journal of Orthopaedic & Sports Physical Therapy. 39(11): 791-798.
Teyhen, D.S., Miltenberger, C.E., Deiters, H.M., Del Toro, Y.M., Pulliam, J.N., Childs, J.D., Boyles, R.E., and Flynn, T.W. 2005. The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. Journal of Orthopaedic & Sports Physical Therapy. 35(6): 346-355.
Vera-Garcia, F.J., Moreside, J.M., and McGill, S.M. 2010. MVC techniques to normalize trunk muscle EMG in healthy women. Journal of Electromyography and Kinesiology. 20(1): 10-16.
Whittaker, J.L., Teyhen, D.S., Elliott, J.M., Cook, K., Langevin, H.M., Dahl, H.H., and Stokes, M. 2007. Rehabilitative ultrasound imaging: understanding the technology and its applications. Journal of Orthopaedic & Sports Physical Therapy. 37(8): 434-449.
OPEN access freely available online
Natural and Life Sciences Communications
Chiang Mai University, Thailand. https://cmuj.cmu.ac.th
Aisha Tukur Mohammed1,6, Patraporn Sitilertpisan1, Sompong Sriburee2, Chich-Haung Richard Yang3, 4, 5, and Aatit Paungmali1, *
1 Department of Physical Therapy, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai 50200 Thailand.
2 Department of Radiologic Technology, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai 50200, Thailand.
3 Department of Physical Therapy, College of Medicine, Tzu Chi University, Taiwan 97004.
4 Department of Biomedical Sciences & Engineering, College of Biomedical Engineering and Technology, Tzu Chi University, Taiwan 97004.
5 Institute of Medicine Science, College of Medicine, Tzu Chi University, Taiwan 97004.
6 Department of Physiotherapy, University of Maiduguri, Borno state, P.M.B 1069, Nigeria.
Corresponding author: Aatit Paungmali, E-mail: aatit.p@cmu.ac.th
Total Article Views
Editor: Waraporn Boonchieng,
Chiang Mai University, Thailand
Article history:
Received: May 17, 2024;
Revised: August 10, 2024;
Accepted: August 14, 2024;
Online First: August 23, 2024

