
The Effectiveness of Herbal Poultice in Relieving Pain and Flexibility in Osteoarthritis Patients
Nunthiya Srikaew*, Natthaphol Phewkham, Sucharat Tungsukruthai, Kusuma Sriyakul, Parunkul Tungsukruthai, Pratya Phetkate, Chuntida Kamalashiran, and Piracha Jumpa-ngernPublished Date : May 16, 2024
DOI : https://doi.org/10.12982/NLSC.2024.031
Journal Issues : Number 3, July-September 2024
Abstract Knee osteoarthritis (OA) is a chronic condition that causes joint degradation and primarily affects the elderly, reducing their quality of life and physical movements. The objective of this study was to determine the efficacy of Thai herbal poultice in relieving pain in OA patients. A single-blind, randomized controlled trial was conducted amongst OA patients at Integrative medicine clinic, Chulabhorn International College of Medicine, Thammasat University, Thailand. Participants were randomly allocated to the Thai herbal poultice or the diclofenac gel group (N=30). The main outcomes were evaluated using visual analog scale (VAS), isokinetic testing, goniometer, and knee injury and osteoarthritis outcome scores (KOOS) at different time assessment. Data were analyzed by the paired t-test and analysis of variance (ANOVA). Thai herbal poultice and diclofenac group showed a significant difference in both the VAS pain scores, extension and flexion as well as KOOS scores (P < 0.01 in both groups). In addition, when compared to diclofenac group, Thai herbal poultice group were significantly improve pain score at the sixth time point following the intervention (P < 0.01). Furthermore, no patients have experienced allergic reactions to therapies. In conclusion, Thai herbal poultice showed more efficiency in reducing pain scores than diclofenac gel without causing undesirable side effects.
Keywords: Thai herbal poultice, Knee osteoarthritis, Isokinetic tests, Visual analog scale, Diclofenac
Funding: The researchers are grateful for the research funding provided by the Research Fund of Chulabhorn International College of Medicine Contract No: G 7/2565
Citation: Srikaew, N., Phewkham, N., Tungsukruthai, S., Sriyakul, K., Tungsukruthai, P., Phetkate, P., Kamalashiran, C., and Jumpa-ngern, P. 2024. The effectiveness of herbal poultice in relieving pain and flexibility in osteoarthritis patients. Natural and Life Sciences Communications. 23(3): e2024031.
INTRODUCTION
Knee osteoarthritis (OA) is widely recognized as a prevalent degenerative joint condition that frequently affects the elderly population (Heidari, 2011). Prior research has indicated that approximately 30% of individuals aged 45 years and above experience osteoarthritis (Cui et al., 2020). Pain and postural dysfunction are prevalent complaints that have a considerable impact on physical mobility and greatly influence the overall quality of life among the senior population (Cook et al., 2007; Turcot et al., 2015). In addition, knee osteoarthritis is commonly associated with the cumulative effects of wear and tear, age-related processes, and obesity (Chen et al., 2020).
The pathophysiology of OA involves the degeneration and increasing deterioration of articular cartilage, accompanied by a decrease in synovial fluid, leading to enhanced inflammation inside the knee joint (Dulay et al., 2015). In addition, the three types of osteonecrosis that can affect the knee are secondary, post-arthroscopic, and spontaneous osteonecrosis of the knees (Serrano DV et al., 2022). Osteoarthritis in the knees affects most patients with pains that encourage them to find treatment. Doxycycline is a drug that has been proposed to modify osteoarthritis (OA) progression and its role as an antibiotic. (Shanmugasundaram S et al., 2023). However, non-steroidal anti-inflammatory medicines (NSAIDs) are typically the first-line pharmacologic therapy for knee osteoarthritis (Mora et al., 2018). Diclofenac is a well-known NSAID commonly prescribed as medication for pain relief, inflammation reduction, and fever alleviation (Bariguian Revel et al., 2020). The mechanism of action involves the suppression of cyclooxygenase 1 (COX-1) and cyclooxygenase 2 (COX-2) enzyme activity (van Erk et al., 2010). The suppression of COX-2 activity is the most likely mechanism by which NSAIDs exert their analgesic effects (Gallelli et al., 2013). Nevertheless, long-term use of NSAIDs for pharmacological therapy has a significant risk and only provides temporary relief (Bookman et al., 2004; Shep et al., 2019).
Previous research has established a correlation between the extended use of NSAIDs and the occurrence of stomach or duodenal ulcers, as well as erosions of the gastroduodenal mucosa (Tai and McAlindon, 2021). Because of the risk factors and restrictions associated with the use of NSAIDs, up to 90% of OA patients are unsatisfied with these medications and contemplate considering traditional and complementary medicine (TCM) (Nik Shafii et al., 2018). There is growing evidence that Complementary and Alternative Medicine (CAM), which includes practices and herbal medicines, is gaining popularity and being used by people around the world for its positive effects such as anti-inflammation and pain relief (Klajing et al., 2023).
In Thailand, the utilization of herbal poultice as a therapeutic intervention for Thai individuals suffering from OA has been an established practice. The poultice, which is typically wrapped in cotton sheets and heated with steam, combines aromatic herbs and spices (Chatawatee et al., 2022). The Thai herbal poultice (THP) has been combines with various ingradients including Zingiber cassumunar Roxb., Citrus hystrix DC., Piper nigrum L., Ludisia discolor (Ker Gawl.) A.Rich., Curcuma aromatic Salisb., Acorus calamus Linn., Gynura pseudochina (L.) DC., Alpinia galangal (L.) Willd., Plumbago indica L., Piper retrofractum Vahl., Drypetes roxburghii (Wall.), Tamarindus indica L., Acacia concinna (Willd.) DC., Dryobalanops aromatica Gaertn.
According to the literature, the medicinal plants used to manufacture THP have anti-inflammatory and analgesic properties. Zingiber cassumunar Roxb., commonly referred to as "Plai" in Thai, has been traditionally employed for the treatment of bruising, sprains, and musculoskeletal pain (B. Chongmelaxme et al., 2017). Plai exhibited anti-inflammatory action in rats with carrageenin-induced paw edema, along with analgesic properties (Han et al., 2021; Panthong et al., 1997). Moreover, prior research reported that Plai cream exhibited greater effect than diclofenac gel in a treatment of patients with mild to moderate OA (Srirochana, 2010). Another combination is Piper nigrum L., which has anti-inflammatory properties as well as analgesic effect (F. Tasleem et al., 2014). Several investigations have demonstrated that Piper nigrum L. has the potential to decrease the levels of proinflammatory cytokines, specifically Interleukin-1β (IL-1β), IL-6, and Tumor necrosis factor- α (TNF-α), together with COX-2 (Duan et al., 2022; Farhana Tasleem et al., 2014).
Altogether, the aforementioned information demonstrates that this THP has the ability to alleviate pain caused by inflammation. However, scientific evidence supporting the therapeutic effects of this THP is still limited. Therefore, the aim of this study was to determine the efficacy of the THP versus diclofenac gel for knee pain alleviation in patients with OA. We firstly examined extension and flexion by using isokinetic evaluation. Then, we utilized a visual analogue scale (VAS) to assess individuals' pain levels. Furthermore, we employed a Goniometer to estimate the range of motion of the knee joint in the flexion and extension planes. Likewise, we used the Knee Injury and Osteoarthritis Outcome Score (KOOS) to measure participants' overall symptom alleviation and quality of life.
MATERIAL AND METHODS
Trial design and study setting
This study was a single-blind randomized controlled trial, which the evaluator blind conducted at Integrative Medicine Clinic, Chulabhorn International College of Medicine, Thammasat University, Thailand. The study was approved by the 1st Ethics Review Committee for Research Involving Human Subjects, of Thammasat University (MTU-EC-OO-6-116/65).
Participants and intervention
The sample size was calculated by the G* Power program with a type I error rate of alpha of 0.05, a power of 90%, and an effect size of 0.91. As a result, the appropriated number of samples was 54 plus a 10% drop out. Hence, the total sample size was 60 people. A simple random technique using a computer-generated method was applied to allocate participants into two groups: (1) the herbal poultice group (N=30) and (2) the diclofenac group (N=30).
The research was conducted at the Integrative Medicine Clinic, Chulabhorn International College of Medicine, Thammasat University. The participants were sixty patients with knee pain who were screened by an applied Thai traditional medicine after which the patients were diagnosed by the orthopedists based on standard criteria for diagnosis for knee osteoarthritis (knee pain, joint crepitation on movement). The inclusion criteria consisted of pain in the knee and five of the following conditions: 1) Both male and female, age 40-80 years, 2) Participants with 20-29 score of Oxford Knee scores, 3), moderate level of pain (VAS 4–6 score), 4) participants must stop using NSAIDs, and/ or other forms of treatment for at least 2 weeks, and 5) participants oriented to the risks and benefits of the research and willing to sign the consent form. The subjects who met the inclusion criteria were asked to join and had to sign an informed consent form before participation. All individuals were able to walk and were assessed for all measurements. The exclusion criteria consisted of a diagnosis of OA caused by other diseases, such as rheumatoid arthritis, gouty arthritis or any accident/sports, contagious diseases, applying any other topical medicine on the knee, had knee replacement surgery, post meniscectomy, post traumatic, values/varus knee, medical and herbal sensibility, if the subjects plan to admit for surgery or move to other place during the study and failed to follow the conditions of the research or missed appointments.
Randomization
After the signed informed consent forms were obtained, sixty participants who met the inclusion criteria were randomly divided into two groups (30 persons each group); 1) the treatment group; and 2) control group. The treatment group was given a 30-minute herbal poultice twice a week. On the other hand, the control group received approximately 2-4 grams of diclofenac gel which was administered three to four times a day. The allocation sequence was carried out through placing the allocated cards in opaque, sealed, and stapled envelopes to preserve concealment by a traditional doctor who did not participate in this research.
Treatment
The treatment received herbal poultices twice a week (day1 and day 4) continuously for 3 weeks by Thai traditional medicine practitioners with licenses and experience of more than 5 years. The herbal poultice procedures are shown in Figures 1–2. In this research, the researcher used the herbal poultice formula of the Thai Traditional and Integrative Medicine Hospital (Yotse). The research assistant performed the herbal poultice. By cleaning the knee area first, then take a cotton pad size 15 x 15 cm., moistened with herbal solution that has already been fermented, use it in an amount of 20 cc. or soak the cotton pad. Then place the patch on the affected knee and leave it for 30 minutes. Once the time is up, clean the knee area twice a week.The control group received approximately 2-4 grams of diclofenac gel which was administered three to four times a day.

Figure 1. Prepare an herbal poultice pad

Figure 2. The herbal poultice was pasted on knee for 30 minutes
Outcome measures
The primary efficacy of the THP was assessed by the Biodex System 4 (Biodex Medical Systems Inc., New York, USA) dynamometer for measuring knee flexion and extension. The knee Injury and osteoarthritis outcome score (KOOS) under five domains; 1) symptoms, 2) pain, 3) functions and daily living, 4) sports and recreation and, 5) quality of life was assessed before and after treatment (week 1, day 1) and (week 3 day 4, final day of treatment). VAS consists of a score 0 - 10 with the endpoints defining extreme limits such as no pain (number 0) and extreme pain (number 10) and goniometer for measurement of the joints angle at extension and flexion positions. After intervention the subjects were evaluated at baseline, twice a week (day1 and day 4) continuously for 3 weeks.
Statistical analysis
Background characteristics data were presented as frequency, percentage, and mean ± standard deviation (SD). Data was analyzed using SPSS version 17. Statistical analysis was performed using Chi-square and F-test to compare the background characteristics data. Pair t-test was also used to analyze statistical differences of Isokinetic tests, VAS, Goniometer and KOOS score within the group, and the determination of differences between groups were compared by independent-samples-t-test. The minimal level of significance was identified at P < 0.05.
RESULTS
Patient characteristics
82 participants were screened, and sixty participants were enrolled in the study. A total of 60 patients (30 in the curcumin group and 30 in the diclofenac group) completed the study and were subjected to statistical analysis as shown in figure 3. The treatment groups were comparable in terms of demographic characteristics (i.e., gender age, body mass index, education, occupation, and side of pain) as shown in Table 1.
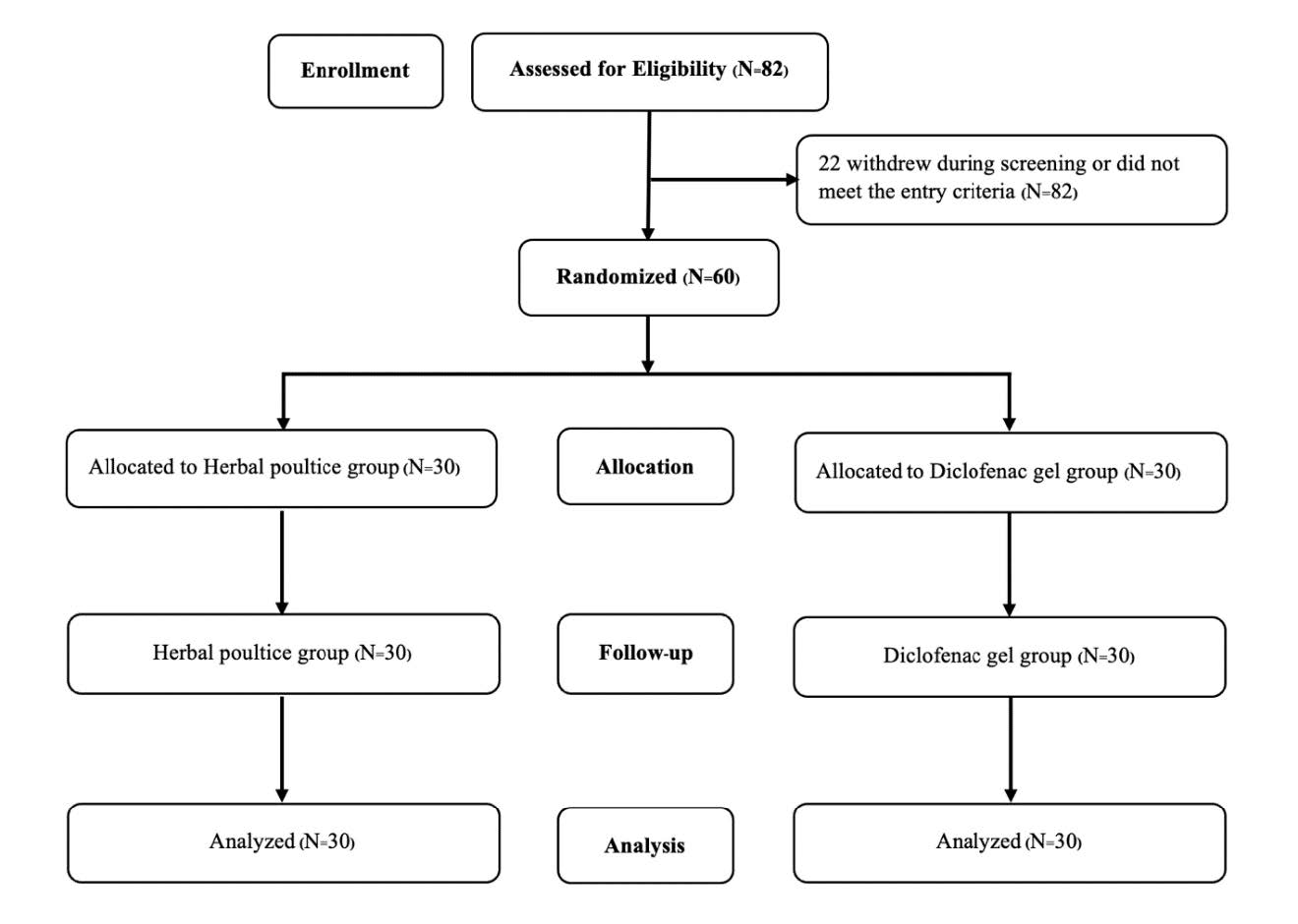
Figure 3. Flow chart of patients who participated in the clinical trial
Table 1. Demographic characteristics of participants.
|
Characteristics |
THP (N=30) |
Diclofenac gel (N=30) |
P-value |
|
Gender1 |
|
|
|
|
Female |
27 (90) |
26 (86.70) |
0.69a |
|
Male |
3 (10) |
4 (13.30) |
|
|
Aged (years)2 |
|
|
|
|
Mean± SD |
55.80 ± 9.06 |
51.63 ± 9.83 |
0.09b |
|
Body Mass Index (kg/m2)2 |
|
|
|
|
Mean± SD |
25.95 ± 3.82 |
25.22 ± 4.14 |
0.48b |
|
Education1 |
|
|
|
|
Primary School |
14 (46.70) |
9 (30) |
0.07b |
|
Secondary School |
12 (40) |
11 (36.70) |
|
|
Bachelor Degrees |
4 (13.30) |
10 (33.30) |
|
|
Occupation1 |
|
|
|
|
Employee |
24 (80) |
17 (56.70) |
0.08b |
|
Government officer |
5 (16.70) |
10 (33.30) |
|
|
Self-employed |
1 (3.30) |
3 (10) |
|
|
Side of pain1 |
|
|
|
|
Right |
18 (60) |
20 (66.70) |
0.60a |
|
Left |
12 (40) |
10 (33.30) |
|
Note: Chi-square test a, F-testb, Number of percentage1, Mean ± standard deviation2
The effect of THP on extension and flexion by using isokinetic assessment
One technique that is frequently used to evaluate muscle pathology and performance is isokinetic dynamometry. This method can accurately and sensitively evaluate the effects of therapeutic interventions (Batalha et al., 2023; Ong et al., 2024). Consequently, we employ this evaluation to assess the effectiveness of the Diclofenac gel and THP. When comparing the results of isokinetic knee muscle strength testing between groups, the THP group performed superior in the Flexion test than the Diclofenac gel group, with a statistical significance of P <0.05 after the sixth treatment (Table 2).
Table 2. Comparison of Extension and Flexion by Isokinetic Testing (60 Deg/Sec).
|
Outcome |
Group |
1st time |
6 th time |
P-value |
|
Extension |
THP |
79.21 ± 44.81 |
106.08 ± 45.81 |
0.01a |
|
|
Diclofenac gel |
66.19 ± 40.22 |
83.90 ± 43.47 |
0.02a |
|
|
P-value |
0.24 |
0.06 |
|
|
Flexion |
THP |
29.92 ± 21.93 |
46.88 ± 22.24 |
0.01a |
|
|
Diclofenac gel |
22.18 ±19.52 |
29.11 ± 17.20 |
0.06 |
|
|
P-value |
0.15 |
0.01b |
|
Note: P-valuea Pair t-test compare within group, P-valueb Independent Samples t-test compare between groups.
The effect of THP on VAS pain score
Both treatment groups exhibited a significant decrease in VAS scores at the sixth time point compared to their baseline measurements (P <0.01). The VAS score of the THP group exhibited a significant decrease from an initial value of 5.53 ± 0.51 to a final value of 2.73 ± 1.11 (P <0.01). Similarly, the diclofenac group also had a significant decrease in VAS from 5.17 ± 0.70 to 3.50 ± 1.23. Although there was a significant difference in the VAS scores across groups initially, the impact of THP (the intervention) was found to be significant at the sixth time point following the intervention (Table 3).
Table 3. The comparison of VAS mean score between and within the groups.
|
Outcome |
Group |
1st time |
2nd time |
3rd time |
4th time |
5th time |
6th time |
P-value |
|
VAS |
THP |
5.53 ± 0.51 |
4.70 ± 0.92 |
4.33 ± 1.06 |
3.90 ± 0.89 |
3.33 ± 1.24 |
2.73 ± 1.11 |
0.01a |
|
|
Diclofenac gel |
5.17 ± 0.70 |
4.73 ± 1.20 |
4.87 ± 1.25 |
4.23 ± 1.28 |
3.80 ± 1.35 |
3.50 ± 1.23 |
0.01a |
|
|
P-value |
0.02b |
0.90 |
0.08 |
0.25 |
0.17 |
0.01b |
|
Note: P-valuea Repeated Measures ANOVA compare within group, P-valueb Independent Samples t-test compare between groups.
The effect of THP on Extension and Flexion measured by goniometer
Measuring knee range of motion is critical for both examination and post-operative outcomes (Hancock et al., 2018). The goniometer was utilized to evaluate the angle of joints, and it was observed that the average extension score exhibited a significant reduction following therapy in both groups. Moreover, the average flexion score of both groups exhibited significant increase when comparing pre-treatment and post-treatment. Remarkably, even on the first measurement, the flexion in the diclofenac group was significantly higher than that THP group. The flexion outcome of the THP group was significantly higher than that of the diclofenac group after the sixth treatment as shown in Table 4.
Table 4. The mean score of Extension and Flexion measured by goniometer.
|
Outcome |
Group |
1st time |
2nd time |
3rd time |
4th time |
5 th time |
6 th time |
P-value |
|
Extension |
THP |
2.77 ± 0.86 |
2.33 ± 0.96 |
2.13 ± 1.01 |
1.70 ± 0.70 |
1.60 ± 0.89 |
1.30 ± 0.60 |
0.01a |
|
|
Diclofenac gel |
3.40 ± 1.10 |
3.23 ± 1.31 |
3.17 ± 1.37 |
2.50 ± 1.11 |
2.47 ± 0.90 |
1.90 ± 0.92 |
0.01a |
|
|
P-value |
0.02b |
0.01b |
0.01b |
0.01b |
0.01b |
0.01b |
|
|
Flexion |
THP |
125.47 ± 8.83 |
132.10 ± 10.61 |
133.17 ± 11.61 |
139.90 ± 7.07 |
140.63 ± 6.36 |
143.40 ± 5.21 |
0.01a |
|
|
Diclofenac gel |
134.00 ± 9.04 |
134.53 ± 8.09 |
134.73 ± 7.03 |
133.77 ± 9.92 |
138.17± 7.64 |
139.03 ± 8.07 |
0.01a |
|
|
P-value |
0.01b |
0.32 |
0.53 |
0.01b |
0.18 |
0.02b |
|
Note: P-valuea Repeated Measures ANOVA compare within group, P-valueb Independent Samples t-test compare between groups.
The effect of THP on KOOS mean score
Knee Injury and Osteoarthritis Outcome Score (KOOS) was an accurate, reliable, and responsive instrument used for evaluating short-term and long-term follow-up (Roos, 2023; Roos and Lohmander, 2003). The results found that when comparing the data before and after therapy in the two groups, there was a significant difference (P < 0.05) in the mean values of symptoms, pain severity, daily living score, and quality of life. In addition, at the sixth time point, there was no significant difference among the two treatment groups as shown in Table 5. Moreover, patients have not experienced any allergic responses.
Table 5. The comparison of KOOS mean score between and within the groups.
|
Outcome |
Group |
1st time |
6 th time |
P-value |
|
Symptoms |
THP |
41.55 ± 10.04 |
70.83 ± 9.43 |
0.01a |
|
|
Diclofenac gel |
30.60 ± 12.61 |
69.40 ± 14.88 |
0.01a |
|
|
P-value |
0.01b |
0.66 |
|
|
Pain score |
THP |
44.72 ± 10.53 |
74.07 ± 11.93 |
0.01a |
|
|
Diclofenac gel |
32.04 ± 11.32 |
70.93 ± 12.65 |
0.01a |
|
|
P-value |
0.01b |
0.33 |
|
|
Daily living score |
THP |
41.86 ± 14.81 |
76.96 ± 12.76 |
0.01a |
|
|
Diclofenac gel |
29.56 ± 14.88 |
73.87 ± 14.02 |
0.01a |
|
|
P-value |
0.01b |
0.38 |
|
|
Sports and recreational score |
THP |
57.17 ± 15.35 |
62.17±16.22 |
0.31 |
|
|
Diclofenac gel |
42.83 ± 17.00 |
57.00±17.35 |
0.02a |
|
|
P-value |
0.01b |
0.24 |
|
|
Quality of life score |
THP |
50.00 ± 10.89 |
61.25 ± 15.08 |
0.01a |
|
|
Diclofenac gel |
43.13 ± 14.25 |
59.17 ± 17.66 |
0.01a |
|
|
P-value |
0.04b |
0.63 |
|
Note: P-valuea Repeated Measures ANOVA compare within group, P-valueb Independent Samples t-test compare between groups.
DISCUSSION
The results indicated that Thai herbal poultice (THP) ameliorated pain while also improve extension and flexion of knee in osteoarthritis patients. In addition, THP reported no adverse effect. Knee osteoarthritis was usually a progressive disease and might eventually cause disability. To the best of our knowledge, this was the first clinical trial of THP versus diclofenac gel in relieving knee pain in osteoarthritis patients. It most affected the elderly and was caused by gradual loss of articular cartilage (Dulay et al., 2015; Tong et al., 2022). Pharmaceutical treatments such as NSAIDs and corticosteroids were considered as the most effective therapies for knee osteoarthritis. However, NSAIDs were frequently associated with cardiovascular and digestive safety concerns (Magni et al., 2021; Richard et al., 2023). As a result, the alternative treatment needed to be investigated to relieve symptoms while also ensuring safety. To the best of our knowledge, this was the first clinical trial of THP versus diclofenac gel in relieving knee pain in osteoarthritis patients. The results indicated that THP ameliorated pain while also improve extension and flexion of knee in osteoarthritis patients. In addition, THP reported no adverse effect.
In mild to moderate OA, mostly patients experienced pain and decreased the function of knee flexor and extensor. According to Table 2, our findings showed that after the sixth treatment, the THP group outperformed the diclofenac group in terms of improvement on the flexion test. The THP group had a flexion of 46.88 ± 22.24, whereas the diclofenac group had a flexion of 29.11 ± 17.20 (P <0.05). Moreover, after using THP sixth treatment, the VAS scores of the THP group exhibited a significant reduction from 5.53 ± 0.51 to 2.73 ± 1.11, whereas diclofenac group lesser decreased VAS score from 5.17 ± 0.70 to 3.50 ± 1.23 (Table 3). Even though the initial VAS scores between groups were significantly different, the THP group was more effective in relieving pain in patients. Additionally, THP exhibited improvement equivalent to diclofenac for the KOOS mean score of symptoms such as functioning in daily living, and knee-related quality of life (Table 5).
These results were consistent with previous studies on the advantages of utilizing complementary and alternative medicine (CAM) to treat knee pain (Vina et al., 2021; Yu et al., 2020). For instance, using cabbage leaf application was a considerably more effective treatment than topical pain drug for alleviating pain and lowering the severity of osteoarthritis (Chobpenthai et al., 2022). Besides, recent studies had reinforced the evidence that CAM was useful for people with knee osteoarthritis. OA patients who received curcumin showed comparable improvement in severity of pain and KOOS scale when compared with diclofenac. In addition, adverse events were significantly less in the curcumin group than in the diclofenac group (Shep et al., 2019). Also, curcumin extract reduced inflammatory and oxidative stress biomarkers in osteoarthritis of knee (Srivastava et al., 2016). As a results, we hypothesized that the effectiveness of THP in reducing pain was probably due to the anti-inflammatory effect of each extract which utilized in this herbal poultice including Zingiber cassumunar Roxb., Piper nigrum L. and Piper longum L.
To support our hypothesis, recent research identified that Piper longum L. could alleviate joint inflammation, cartilage destruction, and arthritic pain. The results showed that Piper longum L. inhibited the expression of LPS-induced proinflammatory cytokine including IL-1β, IL-6, and TNF-β in both in vitro and animal model (He et al., 2016; Lee et al., 2013). Besides, Zingiber cassumunar Roxb. (Plai) also had anti-inflammatory effect. 14% Plai cream had a significant advantage in pain reduction for muscle pain and ankle sprain (Bunchai Chongmelaxme et al., 2017). In addition, an active compound of Plai, (E)-4-(3′,4′-dimethoxyphenyl) but-3-en-1-ol (compound D) could decrease cytokine-induced up-regulation of catabolic genes involved in cartilage degradation while simultaneously lowering IL-1β expression (Panthong et al., 1997). Moreover, Piper nigrum L. (Black pepper) suppressed the expression of IL-6 and MMP13 as well as PGE2 in a dose dependent manner. Additionally, black pepper also significantly reduced histological staining of the inflammatory area in the ankle joints in rat model (Bang et al., 2009). As a result, the favorable findings in this study were almost certainly related to the combination of Thai herbs. There were some limitations to this study. The first limitation would be a small sample size of this study might contribute to an inadequate power to differentiate the significant difference in clinical efficacy among groups. Therefore, further study using sufficiently. Secondly, the majority of the participants still working as usual which affect the results. Additionally, the selection of subjects with osteoarthritis did not use knee x-rays to confirm the disease. Osteoarthritis is diagnosed using only signs and symptoms from the Oxford Knee score, and future studies should address this limitation. Consequently, further studies with a larger sample size and investigate by using X-ray to confirm the findings.
CONCLUSION
In conclusion, THP could be considered as a potential alternative therapy for osteoarthritis of the knee in reducing pain and improve quality of life. THP is as effective as the standard medication diclofenac and has no adverse effects. Altogether, THP is a safe and cost-effective treatment to alleviate knee osteoarthritis.
ACKNOWLEDGEMENTS
This study was supported by the Research Fund of Chulabhorn International College of Medicine Contract No: G 7/2565."
AUTHOR CONTRIBUTIONS
Nunthiya Srikaew participated in the study design, data collection, analysis and manuscript preparation. Natthaphol Phewkham and Sucharat Tungsukruthai participated in the study design and manuscript preparation. Kusuma Sriyakul, Parunkul Tungsukruthai, and Pratya Phetkate participated in the data collection and manuscript preparation. Chuntida Kamalashiran and Piracha Jumpa-ngern participated in the study design, data analysis, and manuscript preparation.
CONFLICT OF INTEREST
The researchers state that there were no conflicts of interest.
REFERENCES
Bang, J. S., Oh, D. H., Choi, H. M., Sur, B. J., Lim, S. J., Kim, J. Y., Yang, H. I., Yoo, M. C., Hahm, D. H., and Kim, K. S. 2009. Anti-inflammatory and antiarthritic effects of piperine in human interleukin 1beta-stimulated fibroblast-like synoviocytes and in rat arthritis models. Arthritis Research & Therapy. 11(2): R49, 19327174.
Bariguian Revel, F., Fayet, M., and Hagen, M. 2020. Topical diclofenac, an efficacious treatment for osteoarthritis: A narrative review. Rheumatology and Therapy. 7(2): 217-236.
Batalha, N., Sousa, J. P., Fernandes, O., Dias, E., Parraca, J. A., and Villafaina, S. 2023. Effects of an 11-week detraining, imposed by the COVID-19 confinement, on handball players' shoulder rotator isokinetic profile, shoulder range of motion, and ball release velocity. Medicina (Kaunas). 59(9): 37763667.
Bookman, A. A., Williams, K. S., and Shainhouse, J. Z. 2004. Effect of a topical diclofenac solution for relieving symptoms of primary osteoarthritis of the knee: A randomized controlled trial. Canadian Medical Association Journal. 171(4): 333-338.
Chatawatee, B., Chokpaisarn, J., Yusuf, M., Waehama, F., Kunworarath, N., Kongsuwan, C., and Salaemae, M. 2022. Effectiveness of knee acupressure along with herbal knee poultice for knee osteoarthritis treatment: A pilot pre-post clinical study. Journal of Herbal Medicine. 32: 100498.
Chen, L., Zheng, J. J. Y., Li, G., Yuan, J., Ebert, J. R., Li, H., Papadimitriou, J., Wang, Q., Wood, D., Jones, C. W., and Zheng, M. 2020. Pathogenesis and clinical management of obesity-related knee osteoarthritis: Impact of mechanical loading. Journal of Orthopaedic Translation. 24: 66-75.
Chobpenthai, T., Arunwatthanangkul, P., and Mahikul, W. 2022. Efficacy of cabbage leaf versus cooling gel pad or diclofenac gel for patients with knee osteoarthritis: A randomized open-labeled controlled clinical trial. Pain Research and Management. 2022: 3122153.
Chongmelaxme, B., Sruamsiri, R., Dilokthornsakul, P., Dhippayom, T., Kongkaew, C., Saokaew, S., Chuthaputti, A., and Chaiyakunapruk, N. 2017. Clinical effects of Zingiber cassumunar (Plai): A systematic review. Complementary Therapies in Medicine. 35: 70-77.
Cook, C., Pietrobon, R., and Hegedus, E. 2007. Osteoarthritis and the impact on quality of life health indicators. Rheumatology International. 27(4): 315-321.
Cui, A., Li, H., Wang, D., Zhong, J., Chen, Y., and Lu, H. 2020. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. eClinicalMedicine. 29-30: 100587.
Duan, Z., Xie, H., Yu, S., Wang, S., and Yang, H. 2022. Piperine derived from Piper nigrum L. inhibits LPS-induced inflammatory through the MAPK and NF-κB signalling pathways in RAW264.7 cells. Foods. 11(19): 36230067.
Dulay, G. S., Cooper, C., and Dennison, E. M. 2015. Knee pain, knee injury, knee osteoarthritis & work. Best Practice & Research Clinical Rheumatology. 29(3): 454-461.
Gallelli, L., Galasso, O., Falcone, D., Southworth, S., Greco, M., Ventura, V., Romualdi, P., Corigliano, A., Terracciano, R., Savino, R., Gulletta, E., Gasparini, G., and De Sarro, G. 2013. The effects of nonsteroidal anti-inflammatory drugs on clinical outcomes, synovial fluid cytokine concentration and signal transduction pathways in knee osteoarthritis. A randomized open label trial. Osteoarthritis Cartilage. 21(9): 1400-1408.
Han, A. R., Kim, H., Piao, D., Jung, C. H., and Seo, E. K. 2021. Phytochemicals and Bioactivities of Zingiber cassumunar Roxb. Molecules. 26(8): 33921835.
Hancock, G. E., Hepworth, T., and Wembridge, K. 2018. Accuracy and reliability of knee goniometry methods. Journal of Experimental Orthopaedics. 5(1): 46, 30341552.
He, H., Guo, W. W., Xu, R. R., Chen, X. Q., Zhang, N., Wu, X., and Wang, X. M. 2016. Alkaloids from Piper longum protect dopaminergic neurons against inflammation-mediated damage induced by intranigral injection of lipopolysaccharide. BMC Complementary and Alternative Medicine. 16(1): 412, 27776556.
Heidari, B. 2011. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian Journal of Internal Medicine. 2(2): 205-212.
Klajing, W., Sumneang, N., Tan, Y.S., Jaengpromma, P., and Kobroob, A. 2023. Efficacy of knee acupuncture added sanyinjiao point for patients with knee osteoarthritis through attenuated systemic inflammations. Natural and Life Sciences Communications. 22(3): e2023051.
Lee, W., Yoo, H., Kim, J. A., Lee, S., Jee, J.-G., Lee, M. Y., Lee, Y.-M., and Bae, J.-S. 2013. Barrier protective effects of piperlonguminine in LPS-induced inflammation in vitro and in vivo. Food and Chemical Toxicology. 58: 149-157.
Magni, A., Agostoni, P., Bonezzi, C., Massazza, G., Menè, P., Savarino, V., and Fornasari, D. 2021. Management of osteoarthritis: Expert opinion on NSAIDs. Pain and Therapy. 10(2): 783-808.
Mora, J. C., Przkora, R., and Cruz-Almeida, Y. 2018. Knee osteoarthritis: Pathophysiology and current treatment modalities. Journal of Pain Research. 11: 2189-2196.
Nik Shafii, N. A. H., Yaacob, L. H., Ishak, A., and Kadir, A. A. 2018. Traditional and complementary medicine use in knee osteoarthritis and its associated factors among patients in northeast Peninsular Malaysia. Oman Medical Journal. 33(2): 148-153.
Ong, M. T., Chan, J. S., Man, G. C., Qiu, J., He, X., Wang, Q., and Yung, P. S. 2024. Effect of eccentric isokinetic exercise on muscle strength and functional recovery after anterior cruciate ligament reconstruction. Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology. 35: 20-26.
Panthong, A., Kanjanapothi, D., Niwatananant, W., Tuntiwachwuttikul, P., and Reutrakul, V. 1997. Anti-inflammatory activity of compound D {(E)-4-(3',4'-dimethoxyphenyl)but-3-en-2-ol} isolated from Zingiber cassumunar Roxb. Phytomedicine. 4(3): 207-212.
Richard, M. J., Driban, J. B., and McAlindon, T. E. 2023. Pharmaceutical treatment of osteoarthritis. Osteoarthritis and Cartilage. 31(4): 458-466.
Roos, E. M. 2023. 30 years with the knee injury and osteoarthritis outcome score (KOOS). Osteoarthritis and Cartilage, 37838308.
Roos, E. M. and Lohmander, L. S. 2003. The Knee injury and Osteoarthritis Outcome Score (KOOS): From joint injury to osteoarthritis. Health and Quality of Life Outcomes. 1: 64, 14613558.
Serrano, D.V., Saseendar, S., Shanmugasundaram, S., Bidwai, R., Gómez, D., and D'Ambrosi, R. spontaneous osteonecrosis of the knee: State of the Art. Journal of Clinical Medicine. 2022 Nov 25; 11(23): 6943.
Shanmugasundaram S, Solanki K, Saseendar S, Chavada VK, D'Ambrosi R. Role of doxycycline as an osteoarthritis disease-modifying drug. Journal of Clinical Medicine. 2023 Apr 18; 12(8): 2927.
Shep, D., Khanwelkar, C., Gade, P., and Karad, S. 2019. Safety and efficacy of curcumin versus diclofenac in knee osteoarthritis: A randomized open-label parallel-arm study. Trials. 20(1): 214, 30975196.
Srirochana, S. 2010. Efficacy of plai cream compared with diclofenac gel in osteoarthritis of knee. Mahasarakham Hospital Journal. 7: 53-60.
Srivastava, S., Saksena, A. K., Khattri, S., Kumar, S., and Dagur, R. S. 2016. Curcuma longa extract reduces inflammatory and oxidative stress biomarkers in osteoarthritis of knee: A four-month, double-blind, randomized, placebo-controlled trial. Inflammopharmacology. 24(6): 377-388.
Tai, F. W. D. and McAlindon, M. E. 2021. Non-steroidal anti-inflammatory drugs and the gastrointestinal tract. Clinical Medicine (Lond). 21(2): 131-134.
Tasleem, F., Azhar, I., Ali, S. N., Perveen, S., and Mahmood, Z. A. 2014. Analgesic and anti-inflammatory activities of Piper nigrum L. Asian Pacific Journal of Tropical Medicine. 7s1: S461-468.
Tong, L., Yu, H., Huang, X., Shen, J., Xiao, G., Chen, L., Wang, H., Xing, L., and Chen, D. 2022. Current understanding of osteoarthritis pathogenesis and relevant new approaches. Bone Research. 10(1): 60, 36127328.
Turcot, K., Sagawa, Y., Hoffmeyer, P., Suvà, D., and Armand, S. 2015. Multi-joint postural behavior in patients with knee osteoarthritis. The Knee. 22(6): 517-521.
van Erk, M. J., Wopereis, S., Rubingh, C., van Vliet, T., Verheij, E., Cnubben, N. H., Pedersen, T. L., Newman, J. W., Smilde, A. K., van der Greef, J., Hendriks, H. F., and van Ommen, B. 2010. Insight in modulation of inflammation in response to diclofenac intervention: A human intervention study. BMC Medical Genomics. 3: 5, 20178593.
Vina, E. R., Youk, A. O., Quinones, C., Kwoh, C. K., Ibrahim, S. A., and Hausmann, L. R. M. 2021. Use of complementary and alternative therapy for knee osteoarthritis: Race and gender variations. ACR Open Rheumatology. 3(9): 660-667.
Yu, H., Wang, H., Cao, P., Ma, T., Zhao, Y., Xie, F., Yao, C., and Zhang, X. 2020. Complementary and alternative therapies for knee osteoarthritis: A protocol for systematic review and network meta-analysis. Medicine (Baltimore). 99(44): e23035.
OPEN access freely available online
Natural and Life Sciences Communications
Chiang Mai University, Thailand. https://cmuj.cmu.ac.th
Nunthiya Srikaew1,*, Natthaphol Phewkham2, Sucharat Tungsukruthai3, Kusuma Sriyakul1, Parunkul Tungsukruthai1, Pratya Phetkate1, Chuntida Kamalashiran1, and Piracha Jumpa-ngern1
1 Chulabhorn International College of Medicine, Thammasat University, Pathum Thani, Thailand.
2 Department of Sport Science and Sport Development, Faculty of Allied Health Sciences Thammasat University, Pathum Thani, Thailand.
3 Division of Health and Applied Sciences, Faculty of Science, Prince of Songkla University, Songkhla, Thailand.
Corresponding author: Nunthiya Srikaew, E-mail: snunthiy@tu.ac.th
Total Article Views
Editor: Waraporn Boonchieng,
Chiang Mai University, Thailand
Article history:
Received: February 8, 2024;
Revised: April 19, 2024;
Accepted: April 24, 2024;
Online First: May 16, 2024

