
Provisional Outcomes of Affordable Custom Wheelchair Seating for an Individual with Cerebral Palsy: Case Report. Nattapong Polhan, Thanatat Charatrungolan*, Woratee Dacharux, Juthamas Siriwatsopon, and Gary Guerra
Published Date : 2019-08-23
DOI : https://doi.org/10.12982/CMUJNS.2019.0021
Journal Issues :
Number 3 , July-September 2019
ABSTRACT
The person with cerebral palsy has a range of functional limitations which can restrict activities of daily living. Sitting for extended periods is a pertinent issue to address. Custom seating orthosis combined with a wheel- chair could reduce issues associated with long-term sitting in this population. The custom seating system for a child with cerebral palsy GMFCS Level IV was provided and outcome measures which measured functional grasping and seat pressure distribution was evaluated while the patient was seated in a traditional wheelchair as well as the custom seating wheelchair.Time to complete tasks while seated in the custom seating wheelchair was longer in duration than when seated in the traditional wheelchair, however, pressure was reduced in pressure prone areas and distributed more across pressure tolerant areas. The custom seating system provided to this patient evidences the utility and usefulness of a customized orthotic intervention for the wheel- chair intervention. Additional accommodation to the custom seating could posit differences in outcomes as would an increase in study participants.
Keywords: Orthosis, Cerebral palsy, Custom seating, Wheelchair, Assistive technology, Pressure distribution
INTRODUCTION
The individual with cerebral palsy has a potentially wide range of func- tional limitations as a result of their condition (Beckung et al., 2008) The na- ture of this condition lends itself to a loss of an individual’s ability to maintain postural control, and move and control muscles (CDC, 2014) Gross restriction of mobility for some of these individuals results in confinement to wheelchair. As such, this limited mobility can predicate long-term restrictions in joint move- ment, muscle atrophy, sensation disturbances and contractures of the lower ex- tremities (Rosenbaum et al., 2007) Sitting in a fixed position with an inability to self-adjust posture and seating orientation is a cause for concern which can be a pre- cursor for prolonged sitting pressures (Kim, Yoo and Do, 2017) The use of custom seating for these individuals has been shown to provide postural support through reduced trunk flexion and prevention of abnormal gluteal pressures (Yoo, 2015) We provide a case report on the function and seat pressures for an individual with cerebral palsy after prescription of an easily replicable custom seating system.
MATERIALS AND METHODS
Case description
A 22-year old man with tetraplegia spastic cerebral palsy and a Gross Motor Function Classification System (GMFCS) Level IV was evaluated for a wheelchair with customized seating.(Wood and Rosenbaum, 2000) An as- sessment by a physiatrist for manual muscle testing (MMT), Ashworth scale and Thomas Test (negative) were performed. In addition, flexible neuromus- cular scoliosis with muscle tightness of 15° on the right knee and 25° on the left knee as well as pelvic obliquity was observed, see Table 1. Sitting balance was determined to be within normal limits for both static and dynamic balance. The patient was sitting for approximately 8 hours a day in a standard manual wheelchair and had been using custom-made seating for two years prior.
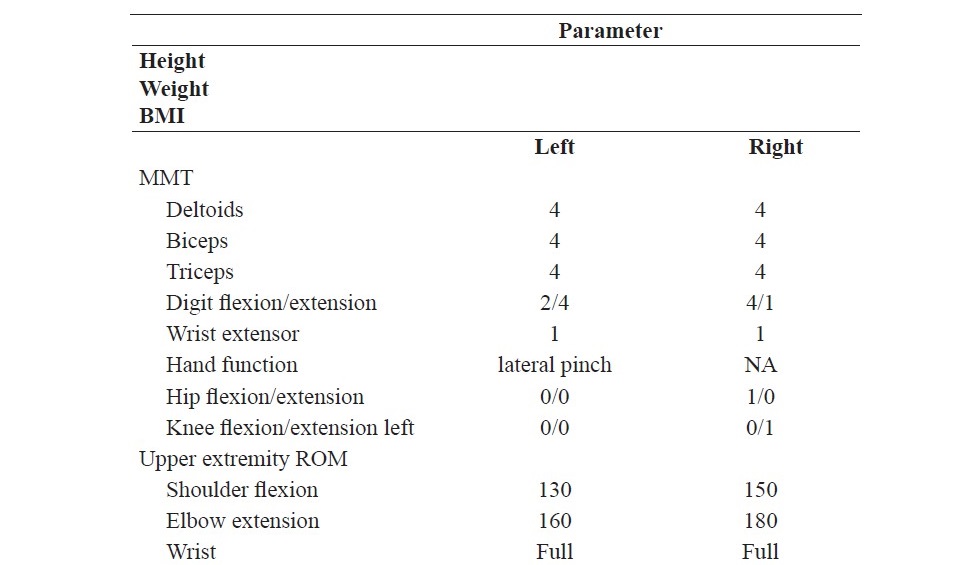
Table 1. Parameters of a 22-year-old male with cerebral palsy (GMFCS IV).
Custom seating orthosis
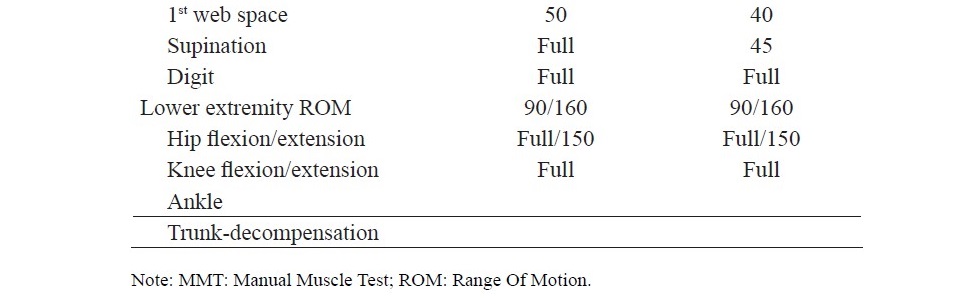
An orthotist created a custom-made seating orthosis which was prescribed by the physiatrist in order to provide a comfortable and optimal base of support for functional mobility. The participant was first seated in a vacuum bean bag appara- tus (VBBA) at 10° of posterior tilt, which enabled the acquisition of the individ- ual contours and corrections of the rear and lower back of the patient (Figure 1).
Figure 1. Image taken during fabrication of patients custom seating orthosis.
It is our anecdotal clinical experience that this orientation can reduce the asymmetrical hip flexion and posture which promotes a suitable weight bearing position.(Ágústsson, Sveinsson and Rodby-Bousquet, 2017) The par- ticipant was transferred out of the VBBA and a Plaster of Paris (POP) cast was made of the preserved custom seating of the VBBA. From the cast, a model was created, modified, and plastazote and polypropylene was then used and contoured to create the final wheelchair seat orthosis, see Figure 2.

Figure 2. Image of the definitive custom seating orthosis wheelchair.
Outcome measures
The patient was seated in their wheelchair which was positioned directly in front of a testing table. Task objects were situated at the umbilicus level of the patient, 30 cm in front of the body. On this table were cylindrical objects of 2 and 5 cm in size. Task 1 (object transfer) required the patient to grab the object with their dominant hand and transfer to a designated location. Task 2 (cup to mouth) required the patient to use their dominant hand to pick up a small plastic cup and bring to their mouth. Task 3 (long distance cup reach) re- quired the participant to reach to a longer distanced cup 60 cm in front of their body. A series of practice trials were permitted and finally three trials were per- formed and used for outcome data collection. During performance of these tasks an instrumented pressure distribution sensor (FSA, Vista Medical, Winnipeg, Canada) collected pressure metrics of the patient along the thighs, hip, and rear. Pressure distribution, peak pressures (Kpa), pressures at the ischial tuberosity, and average total pressures were all collected (Figure 3). We projected nine sections onto the detailed sensor output graphs for nine distinctive areas co- inciding with nine postures of wheelchair users.(Verbunt and Bartneck, 2010)
RESULTS
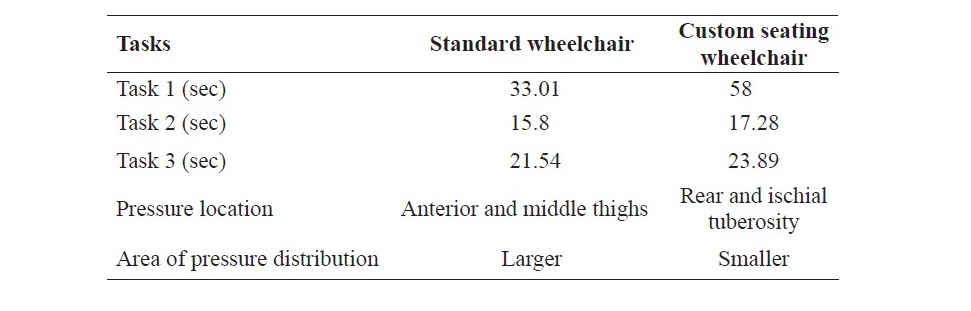
The patient performed all three tasks for a longer duration of time while in the custom seating wheelchair as compared to the standard wheelchair, per- cent time increases were as follows; Task 1 (54.9%), Task 2 (8.9%), Task 3 (5.8%). The visual results from the pressure mapping array evidenced increased localized pressure while the patient was in the standard wheelchair, up to the maximum set pressure of 200 mmHg at the patients rear and ischial tuberosity which was evident across all outcome measurement tasks. In contrast, when the patient was seated in the custom seating wheelchair, pressures shifted from pos- terior to anterior sections along the interior of the middle thighs. Moreover, the patients pressure showed a wider distribution across this same section (Figure 3).
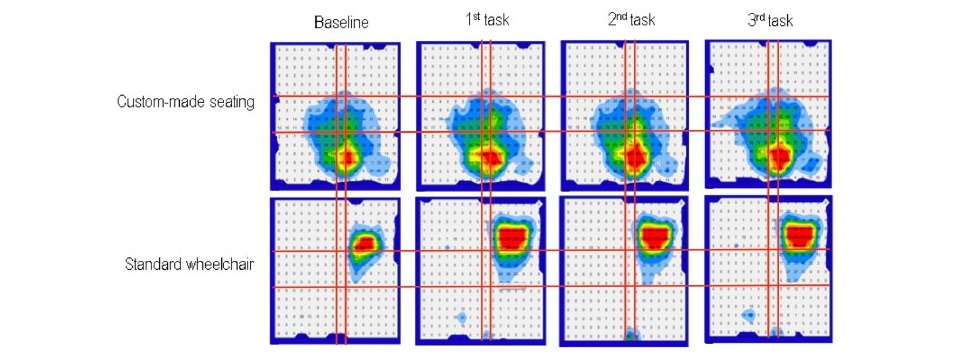
Figure 3. Pressure sensor pressure distribution mapping for the patient in the standard wheelchair (A), and custom seating wheelchair (B). Pres- sure readings from baseline and during three different tasks is il- lustrated. Patient pressure while seated in the standard wheelchair is centered around the ischial tuberosity as opposed to a more dis- tributed pressure while seated in the custom seating wheelchair.
Table 2. Summary of all result.
DISCUSSION
We evaluated the functional outcomes as well as pressure relieving capabilities of the wheelchair. Sitting in the custom seating orthosis wheel- chair saw no decrease in the time taken to complete tasks, however, reduced pressures along the buttocks and an improved distribution of pressures were observed. Previous scholarship has evidenced the propensity for asymmetrical sitting postures in individuals with CP. (Lee and Park, 2015) In our case we were capable of reducing asymmetrical pressure which might have been re- lated to a correction of the patient’s posture. The greater time required for the patient to complete tasks might be related to the cognitive ability of the patient as we observed some inability of the patient to follow our guidance. Trunk con- trol and the ensuing postural control is cornerstone to the functional abilities of the individual with CP. (Wu et al., 2004). Thus, the seat might play an inte- gral role in dictating functional outcomes and should be investigated further.
CONCLUSION
A custom seating orthosis was developed to evaluate the force dis- tribution occurred at the bottom during upper limb functions. The force was satisfied distribution with acceptable time spending compare with seating on a traditional wheelchair. However, the time spending on the custom seat- ing orthosis was not significant improve which may cause from the severity of scoliosis and tilting angle of the orthosis effect trunk flexion motion re- sult in a performance of upper limb function. On the other hand, tradition- al wheelchair allows some translation when the upper body perform some activities, but the excessive pressure remain present all the time. From these result, the further research can be focus on the relationship between the tilt- ing angle and upper limb function during using a custom seating orthosis.
ACKNOWLEDGEMENTS
This project was mainly worked at Sirindhorn School of Prosthetics and Orthotics (SSPO School).
REFERENCES
Ágústsson, A., Sveinsson, Þ., and Rodby-Bousquet, E. 2017. The effect of asymmetrical limited hip flexion on seating posture, scoliosis and windswept hip distortion. Research in Developmental Disabilities. 71: 18–23. https://doi.org/10.1016/j.ridd.2017.09.019
Beckung, E., Hagberg, G., Uldall, P., Cans, C., and for Surveillance of Cerebral Palsy in Europe. 2008. Probability of walking in children with cerebral palsy in Europe. Pediatrics. 121(1): e187-92. https://doi.org/10.1542/peds.2007- 0068
CDC. 2014. Center for Disease Control and Prevention, Cerebral Palsy. Retrieved from http://www.cdc.gov/ncbddd/cp/facts.html.
Kim, D.H., Yoo, W.-G., and Do, J.-H. 2017. Changes in gluteal pressure and cen- ter of force during sitting in children with cerebral palsy. Journal of Physical Therapy Science. 29(12): 2210–2211. https://doi.org/10.1589/jpts.29.2210 Lee, I.-H., and Park, S.-Y. 2015. Abnormal sitting pressures of hemiplegic cerebral palsy children on a school chair. Journal of Physical Therapy
Science. 27(2): 499–500. https://doi.org/10.1589/jpts.27.499
Rosenbaum, P., Paneth, N., Leviton, A., Goldstein, M., Bax, M., Damiano, D., Dan, B., and Jacobsson, B. 2007. A report: The definition and classification of cerebral palsy April 2006. Developmental Medicine and Child Neurology Supplement. 109: 8–14.
Verbunt, M., and Bartneck, C. 2010. Sensing senses: Tactile feedback for the pre- vention of decubitus ulcers. Applied Psychophysiology and Biofeedback. 35(3): 243–50. https://doi.org/10.1007/s10484-009-9124-z
Wood, E., and Rosenbaum, P. 2000. The gross motor function classification system for cerebral palsy: A study of reliability and stability over time. Developmental Medicine and Child Neurology. 42(5): 292–6.
Wu, Y.W., Day, S.M., Strauss, D.J., and Shavelle, R.M., 2004. Prognosis for ambulation in cerebral palsy: A population-based study. Pediatrics. 114(5): 1264–71. https://doi.org/10.1542/peds.2004-0114
Yoo, W.-G. 2015. Effect of a suspension seat support chair on the trunk flex- ion angle and gluteal pressure during computer work. Journal of Physical Therapy Science. 27(9): 2989–90. https://doi.org/10.1589/jpts.27.2989
Nattapong Polhan, Thanatat Charatrungolan*, Woratee Dacharux, Juthamas Siriwatsopon, and Gary Guerra
Sirindhorn School of Prosthetics and Orthoics, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, 10700 Thailand
*Corresponding author. E-mail: thanatat.cha@mahidol.edu
Total Article Views
Article history:
Received: July 24, 2018;
Revised: December 6, 2018;
Accepted: January 11, 2019

