
Effects of Arm Swing Exercise Program on HbA1C and Nutritional Status in Adults and Older Adults with Type 2 Diabetes: A Quasi-Experimental Study
Sangthong Terathongkum and Kamonrat Kittipimpanon*Published Date : July 10, 2023
DOI : https://doi.org/10.12982/NLSC.2023.048
Journal Issues : Number 3, July-September 2023
Abstract Regular physical activity is recommended for managing type-2 diabetes to achieve optimal glycemic control. Limited studies compared the effects of exercise between adults and older adults with type-2 diabetes. This quasi-experimental aim to investigate the effects of the Arm Swing Exercise Program on HbA1C and nutritional status among four groups of adults and older adults with type-2 diabetes. Eighty eligible participants were assigned to the experimental groups (20 adults and 21 older adults) receiving the 12-week Arm Swing Exercise Program 30 minutes/day 5 day/week along with standard care, whereas the control groups (17 adults and 22 older adults) received standard care. Data were obtained, using the demographics questionnnaire, HbA1C, and nutritional status including waist circumference, body mass index, visceral fat, and skeletal muscle, before and after the Program. Paired t-tests, ANCOVA, and ANOVA were used for data analysis. The findings revealed no significant difference in HbA1C, waist circumference, body mass index, visceral fat, and skeletal muscle after receiving the Program between adults and older adults in the experimental groups. Older adults in the experimental group had significantly lower waist circumference than older adults in the control group, while adults in the experimental group had significantly lower waist circumference than adults and older adults in the control groups. This program was effective in only waist circumference reduction. Thus, nurses should encourage people with type-2 diabetes to continuously practice both the arm swing exercise and standard care to achieve glycemic control and better nutritional status. Further study should have more participants using randomized controlled trials and control other sensitive outcomes to the arm swing exercise.
Keywords: Arm swing exercise, Hemoglobin A1C, Nutritional status, Adults, Older adults, exercise
Citation: Terathongkum, S. and Kittipimpanon, K. 2023. Effects of arm swing exercise program on HbA1C and nutritional status in adults and older adults with type 2 diabetes: A quasi-experimental study. Natural and Life Sciences Communications. 22(3): e2023048.
INTRODUCTION
Regular physical activity (PA) is a key protecting factor for self-management of non-communicable diseases (NCDs) such as type 2 diabetes (T2DM) (American Diabetes Association Professional Practice Committee: ADA, 2022; World Health Organization: WHO, 2020). T2DM is a systemic metabolic and degenerative disease leading to insulin resistance and relative deficiencies in insulin secretion, especially in older adults (Liangruenrom et al., 2018; Yang et al., 2019; Mahmudiono et al., 2021; Mekić et al., 2021). These metabolic dysregulation mechanisms are related with age increased resulting in a decrease in the pancreatic cell capacity to produce insulin and the insulin receptor sensitivity to capture insulin. Moreover, the onset of aging-related insulin resistance is attributed specifically to an increase in intra-myocellular fatty acid metabolites leading to a decrease in the mitochondrial oxidative capability. Body composition also changes during older adulthood resulting in a lowering of the fat oxidation rate leading to a gradual accumulation of body fat in the body and a decrease in skeletal muscle. Thus, insulin activity declines. Besides, lifestyle influences, such as a lack of exercise, a decrease in daily activities, and saturated fat consumption, of older adults can also contribute to an increased risk of T2DM more than adults (Chia et al., 2018; Mahmudiono et al., 2021; Mekić et al., 2021). A meta-analysis revealed the protective effect of PA was stronger in the adult group than the older adult group resulting in the prevention of the development of chronic diseases, such as metabolic syndrome, T2DM, hypertension, and stroke (Lin et al., 2020).The PA also upsurges muscle strength, insulin sensitivity, longevity and survival (Lin et al., 2020; Mahmudiono et al., 2021; Mekić et al., 2021).
To date, the World Health Organization and the American Diabetes Association recommend performing lifestyle modification, especially various exercises approximately 150 minutes/week for mild to moderate PA or 75 minutes/week for moderate to high-intensity exercise (WHO, 2020; ADA, 2022). Regular PA has been confirmed in many studies not only to control blood glucose by reducing insulin resistance and promoting insulin secretion but also to reduce risks of cardiovascular disease and obesity in both adults and older adults with T2DM (Chia et al., 2018; Liangruenrom et al., 2018; Phonyiam et al., 2019; Putri et al., 2020; Zheng et al., 2020; Mahmudiono et al., 2021; Mekić et al., 2021; Ooi et al., 2021; Terathongkum et al., 2021).
Arm swing exercise (ASE) has been a type of PA and mind-body intervention from China for more than 50 years, and is a mild to moderate exercise performed without supervision. The ASE is a relaxed, easy and low risk of musculoskeletal injury for people. This exercise focuses on the upper part of the body by moving arms forward lightly about 30 degrees and backward approximately 60 degrees (Khamsom et al., 2017; Wanna et al., 2018; Phonyiam et al., 2019; Terathongkum et al., 2021). Performing the ASE continuously in people with T2DM helps not only decrease inflammatory imbalances of T2DM but also stimulates various mechanisms (Kleebbua et al., 2018; Wanna et al., 2018). Positive emotion will make the hypothalamus release hormones that control the immunity system (Kleebbua et al., 2018; Prasertsri and Leelayuwat, 2019). The modulation, in turn, results in lowered hypothalamic-pituitary-adrenal (HPA) axis activity bringing to reduce cortisol levels affecting metabolism that improves insulin sensitivity and decreases insulin resistance (Khamsom et al., 2017; Pahlevi et al., 2017; Kleebbua et al., 2018; Wanna et al., 2018; Yang et al., 2019; Putri et al., 2020). Hence, the body improves blood glucose uptake into the cells and prevents glucogenesis.
This modality can also increase fat oxidation bringing to decrease in total fat mass and an increase in skeletal muscle. In addition, the skeletal muscle is the major source of glucose uptake in the postprandial state leading to better glucose uptake by translocation of Glucose Transporter 4 (GLUT4) in the muscles (Yang et al., 2019; Putri et al., 2020; Ooi et al., 2021). Furthermore, the ASE can decrease C-reactive protein (CRP), which is an inflammatory marker secreted from the liver stimulated by cytokines. The consequences are impaired insulin signaling, insulin resistance, and beta-cell dysfunction (Khamsom et al., 2017; Kleebbua et al., 2018; Prasertsri et al., 2019; Prasertsri and Leelayuwat, 2019; Putri et al., 2020; Ooi et al., 2021). Hence, the liver assists to produce glucose from the lipolysis of body parts resulting in reduced waist circumference (WC) and body mass index (BMI). Therefore, the ASE can help decrease hemoglobin A1C (HbA1C), WC, BMI, and visceral fat (VF), as well as increase skeletal mass (SM). Previous studies revealed that this training for 8-12 weeks has confirmed the effectiveness in either adults or older adults with T2DM (Khamsom et al., 2017; Wanna et al., 2018; Phonyiam et al., 2019; Sitkulanan et al., 2020; Zheng et al., 2020; Ooi et al., 2021; Terathongkum et al., 2021) including lower HbA1C (Phonyiam et al., 2019; Terathongkum et al., 2021), WC (Khamsom et al., 2017; Wanna et al., 2018), BMI (Wanna et al., 2018; Phonyiam et al., 2019; Terathongkum et al., 2021), VF (Terathongkum et al., 2021) and increase SM (Phonyiam et al., 2019; Terathongkum et al., 2021).
The ASE program based on integration of the psychoneuroimmunology (PNI) (Pahlevi et al., 2017) and the Self-Efficacy Theory of Bandura (1977) which applied four principal sources to enhance outcome expectations for better health. The first is mastery experience being the highest powerful resource emerging from prosperous performance or previous experiences. The second is vicarious experience originating from observing social models and then performing similar activities for health behavior changes. The third is verbal persuasion to inspire people to have more skills and competencies for their health behavior goals. The last resource is physiological and affective states in terms of relaxation and readiness assisting people’ confidence to complete tasks (Bandura, 1977). Hence, this theory was applied in this current study to build confidence and motivate adults and older adults with T2DM to regularly perform ASE.
Although the researchers have examined the effectiveness of the ASE Program on HbA1C and the nutritional status separately for each group of adults (Wanna et al., 2018) and older adults (Khamsom et al., 2017) with T2DM in two Sub-district Health Promotion Hospitals, in a province adjacent to Bangkok, Thailand, we did not compare the effectiveness of the Program between the two age groups. Thus, this study examined the effectiveness of the ASE home-based program between adults and older adults with T2DM on lowering HbA1C and better nutritional status. We hypothesized that in the experimental group, adults with T2DM would have lower HbA1C, WC, BMI, and VF, and higher SM than older adults; older adults with T2DM in the experimental group would have lower HbA1C, WC, BMI, and VF, and higher SM than older adults in the control group; and adults with T2DM in the experimental group would have lower HbA1C, WC, BMI, and VF, and higher SM than adults and older adults in the control groups.
MATERIALS AND METHODS
Design
A quasi-experimental, comparative study with a pretest-posttest design was conducted following the Transparent Reporting of Evaluations with Non-randomized Designs (TREND) (Des Jarlais et al., 2004).
Sample and setting
Two Sub-district Health Promotion Hospitals (SHPH), adjacent to Bangkok, Thailand was selected because of an increasing number of people with diabetes. They were assigned using a lottery without replacement technique to be an experimental group and a control group. Both SHPHs provide the same standard of care. The following inclusion criteria were used to recruit the participants: 1) aged 18 years and up in the adult group and aged 60 years and up in the older adult group; 2) T2DM diagnosed without severe diabetic complications containing cerebrovascular disease, heart disease, retinopathy, nephropathy, and neuropathy; 3) taking oral hypoglycemic medications; 4) being capable to perform an exercise, and 5) willing to participate in this study. We excluded participants who could not participate throughout the program, perform the ASE less than 80% using self-report, and were admitted to the hospital during this study.
The sample size was calculated by using G*Power software with the following parameters: a statistical power = 0.80, a p-value = 0.05, and an effect size = 0.67 estimated from a previous study (Saelao, 2012). Potential sample size for four groups including approximately 20% drop out (Manickum et al., 2022) among adults and older adults in the experiment groups, and adults and older adults in the control groups were 24 participants each group with a total of 96 participants.
Unfortunately, some participants among four groups withdrew from the study with some reasons. Seven participants in both experimental groups were referred to a district hospital for proper management. Similary, nine participants in both control groups were referred to a district hospital for proper management and going back to their homes. Thus, the study continued with eighty participants including 20 adults and 21 older adults in the experiment groups, and 17 adults and 22 older adults in the control groups. Three sub-groups had enough sample size as calculated with the G*power, except adults in the control group being limited in this study.
Research instruments
There were research interventions, data collection instruments, and research control instruments, as follows:
Research interventions
The ASE Program was developed by the principal investigator (PI) based on the Self-efficacy Theory and the PNI. The program was delivered for 12 weeks. The participants received the group-based diabetic education and the ASE training in the first week before assigning to perform the home-based exercise for approximately 150 minutes per week individually, for twelve weeks with recording exercise and daily food consumption (Table 1). This modality began with five minutes-warming up, 30 minutes of continuous ASE, by swinging both arms forward at thirty degrees and backward at sixty degrees in a second, and gradually five minutes-cooled down (Figure 1). Besides, the participants obtained telephone followed up to assess ASE problems and how they solved the problems, and motivated them for continuing exercise, except during the fourth, eighth, and twelfth weeks of visiting the physician and getting the standard care at SHPH with participation in the ASE program through group discussions (6-8 participants per group) for approximately 60 minutes. Three diabetic experts, including a physician, a nursing instructor, and an advanced practice nurse, approved the content of this intervention. They assessed all activities in the intervention protocol for congruency and relevance to the conceptual framework yielding a content validity index (CVI) of 1.0.
Table 1. Schedule of the arm swing exercise (ASE) program and standard care.
|
Week |
Component of Bandura’s Theory |
Activities |
|
Arm Swing Exercise Program |
||
|
1 |
Vicarious experience
|
Group Discussion (6-8 persons for 60 mins) 1. Share a model case achieving glycemic control and waist circumference reduction. |
|
|
Verbal persuasion |
2. Give the benefit of ASE |
|
|
Psychological and affective states |
3. Educate ASE instruction via VDO, demonstration, and return demonstration ASE |
|
|
Mastery Experience
|
4. Assigning the participants to perform ASE at home for 30 minutes/day, 5 days/week for 12 weeks. |
|
2,3 and 5,6,7 and 9,10,11
|
Verbal persuasion Psychological and affective states Mastery experience |
Telephone Follow-up individually (20 mins) 1. Encourage participants to share their experiences, feelings, and existing problems 2. Share problem-solving strategies between nurses and the participants 3. Encourage participants to continuously perform ASE regularly |
|
4,8, and 12 |
Vicarious experience Mastery experience Verbal persuasion Psychological and affective states |
Group Discussion (6-8 people for 60 mins) 1. Encourage participants to share their ASE experience, feelings, existent problems, and problem-solving through group discussion. 2. Motivating the participants to perform ASE regularly 3. Meet with a physician and receive medication. |
|
Standard care (Seven colors of ping pong) |
||
|
1 |
|
1. Diabetic education included lifestyle modification, taking medicine regularly, and diabetic complication assessment. 2. Meet with a physician and receive medication. |
|
4, 8, and 12 |
|
1. Diabetic education included lifestyle modification, taking medicine regularly, and diabetic complication assessment. 2. Meet with a physician and receive medication. |
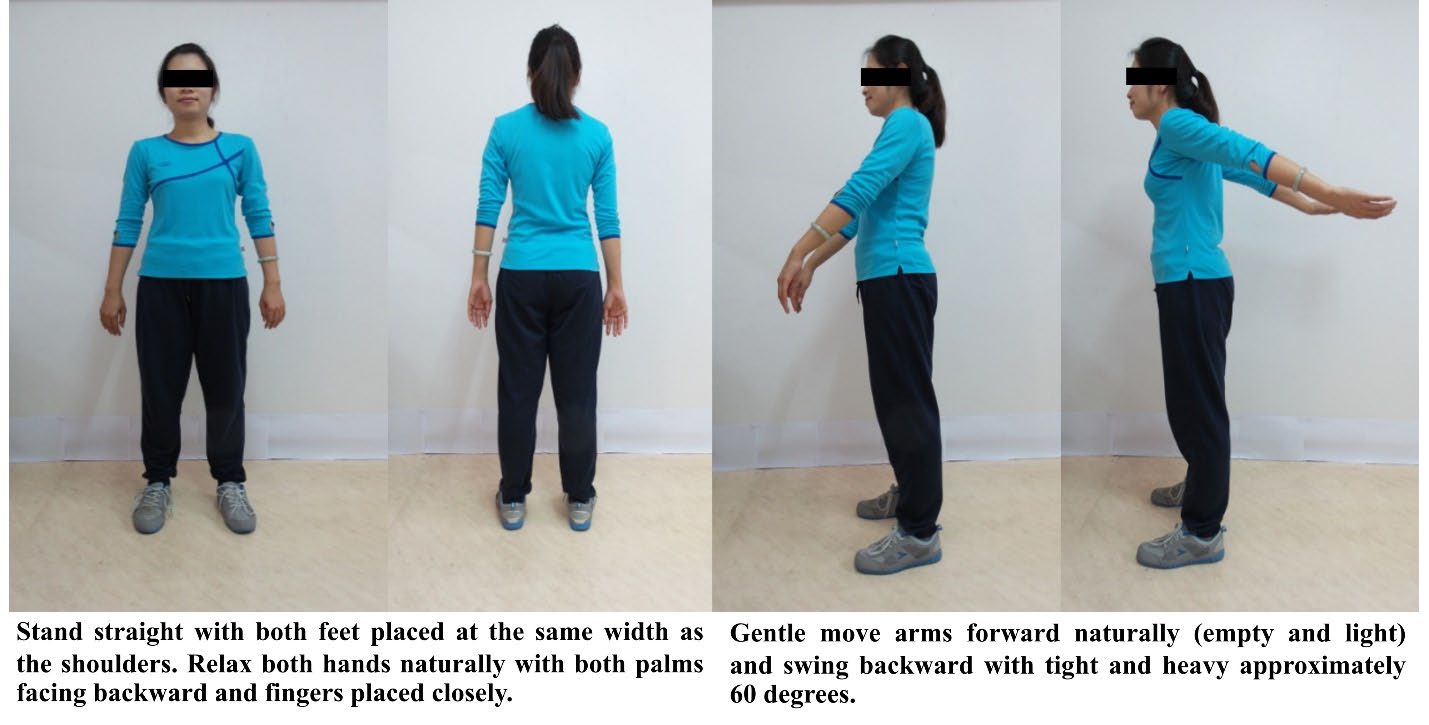
Figure 1. Method of the arm swing exercise.
Standard care: Nurses at the NCD clinic provide care for people with DM using “Seven-Color Life Traffic Ping-Pong” developed by Vichai Teintavorn using the primary health care system for surveillance and epidemiology in people with diabetes and hypertension (Teintavorn, 2013). This tool is applied in NCD clinic in primary care dividing people following blood glucose and severity into four groups including a normal group, a pre-diabetes/ risk group, a diabetes group, and a diabetic group with complications (Table 2). All participants were in the third group of “Seven Color Life Traffic Ping-Pong.” They received diabetic education including lifestyle modification, taking diabetic medicine, assessing diabetic complications (retinopathy, nephropathy, neuropathy, and cardiovascular risk), and meeting with a physician every 4 weeks.
Table 2. Standard care following “Seven-Color Life Traffic Ping Pong”29.
|
Colors |
CBG Level |
Care |
|
1. White |
< 100 mg% |
Diabetic education-related lifestyle modification |
|
2. Light Green |
100-125 mg% |
Every visit (4 weeks) |
|
3. Green |
< 126 mg% |
1. Meeting with a physician every 4 weeks and receiving medication treatment 2. Diabetic education included lifestyle modification, taking medicine regularly, diabetic complication assessment Every visit (4 weeks) * Orange and Red colors will receive home visits from nurses with the purpose of follow-up and encouraging their self-management |
|
4. Yellow |
126-154 mg%/ HbA1C < 7 % |
|
|
5. Orange |
155-182 mg%/HbA1C |
|
|
6.Red |
< 183 mg%/HbA1C > 8 % |
|
|
7.Black |
Present Complication |
Refer to the District Hospital for proper management |
Data collection instruments consisted of a Demographic Questionnaire and an Outcomes Record Form.
Demographic Questionnaire was developed by the PI consisting of age, gender, highest education, marital status, occupation, family income, diabetic duration, co-morbidities, exercise or PA, smoking, and alcohol consumption.
Outcomes Record Form was developed by the PI to record anthropometric measures and laboratory findings including HbA1C, WC, BMI, VF, and SM. All outcomes were measured at baseline and 13th week. The outcomes measurement was described below:
HbA1C is a blood glucose test drawn by a research assistant and examined by a technician in the laboratory of the same district hospital in order to examine the HbA1C value.
Waist circumference (WC) was measured by standard tape at the horizontal plane midway between the lowest rib and the iliac crest of the participants on centimeters (cm) and millimeters (mm) scale.
Body mass index (BMI), visceral fat (VF), and skeletal muscle (SM) were measured using a body composition analyzer (OMRON-HBF-375, model) being standardized. It was calibrated before collecting the data and applying the same one throughout the study.
Research control instruments were developed by the PI including the ASE record form to self-monitor compliance with the ASE protocol, a food consumption form to memo the type and amount of food intake covered in a day, and a researcher’s telephone follow-up record form to note problems and problem-solving during the ASE activity of the participants.
Ethical considerations
After IRB approval from the Institutional Review Board, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Thailand (ID 08-58-33), the researchers introduced themselves and asked eligible participants for involvement in the study. We informed the purpose of the study, the data collection procedure, and the right to refuse and withdraw from this study at any time without affecting the standard services. Moreover, we acquainted assurances of privacy and confidentiality of all information. Then, we asked the eligible participants to sign an informed consent. Finally, the research assistants collected data and the researchers conducted all interventions.
Data collection process
We recruited two research assistants (RAs) who were registered nurses, had nursing experience at least one year, and did not work in the research setting. We demonstrated all procedures for collecting data and asked them to return demonstration with the same samples until they felt confident to get an accurate measurement. This was done to ensure the accuracy of the measurement, especially for those anthropometry measures without calculating reliability coefficients.
After the informed consent was obtained, the RAs who were single-blind, in which group assignment was not revealed to the RAs, collected all data before starting the program by (1) asking the participants to respond to the Demographic Questionnaire, (2) drawing participants’ blood before sending to the technician in the laboratory for HbA1C examination and measured WC, BMI, VF, and SM. If RAs had any problems during data collection, the PI was available to assist. Then, the researchers conducted the 12-week program as shown in Figure 1. After that, the RA collected all data again at week 13.
Data Analysis
SPSS version 18.0 for Windows was used to analyze descriptive statistics and inferential statistics. The first one described the participants’ characteristics and all dependent variables using the range, mean, standard deviation (SD), frequency (n), and percentage (%). Between-group comparisons were conducted to examine the differences in categorical characteristics variables by using chi-square or Fisher’s exact test, and ANOVA for continuous variables. The assumptions were checked and achieved for all outcome variables. Paired t-test, ANCOVA, ANOVA, and Post-hoc analysis with Least Significant Difference (LSD) were used to examine the differences in average HbA1C, WC, BMI, VF, and SM within and among four groups. A one-tailed test for a significance level (α) was set at .05.
RESULTS
Eighty participants with T2DM in this study had four groups, including both experimental groups contained with 21 older adults and 20 adults each group receiving the ASE program and both control groups receiving standard care comprised with 22 older adults and 17 adults each group. Most participants were female with the highest education of a primary school and the average age of 68.2 + 5.7 years, 52.9 + 4.9 years, 68.9 + 4.9 years, and 52.0 + 6.5 years, respectively. The average diabetic durations in both experimental and control groups were 5.3-10.7 and 8.8-10.6 years, respectively. There were no significant differences among the four groups (P >.05), except in age, marital status, and diabetic duration (P <.001, P <.01, and P <.05, respectively) as shown in Table 3.
Table 3. Comparison of characteristics between adults and older adults with T2DM in the experimental and the control groups (N =80).
|
Variables |
Frequency (%) |
P-value |
|||
|
|
Older adult experiment (n=21) |
Adult experiment (n=20) |
Older adult control (n=22) |
Adult control (n=17) |
|
|
Gender Male |
3 (14.30) |
4 (20.00) |
5 (22.70) |
1 (5.90) |
0.515a |
|
Female |
18 (85.70) |
16 (80.00) |
17 (77.30) |
16 (94.10) |
|
|
Age (years) mean + SD |
68.20 ± 5.70 |
52.90 ± 4.90 |
68.90 ± 4.90 |
52.00 ± 6.50 |
0.000b |
|
range |
61-83 |
45-59 |
63-80 |
37-59 |
|
|
Education Primary school |
16 (76.20) |
14 (70.00) |
17 (77.30) |
13 (76.50) |
0.948a |
|
Higher primary school |
5 (23.80) |
6 (30.00) |
5 (22.70) |
4 (23.50) |
|
|
Marital status Single & divorce |
10 (47.60) |
3 (15.00) |
15 (68.20) |
5 (29.40) |
0.003a |
|
Married |
11 (52.40) |
17 (85.00) |
7 (31.80) |
12 (70.60) |
|
|
Income (Baths) mean + SD |
10,166.70 ± 6,854.40 |
13,550.00 ± 9,225.10 |
13,000.00 ± 11,058.30 |
14,470.60 ± 11,214.50 |
0.540 b |
|
(USD) |
294.26 ± 198.39 |
392.19 ± 267.00 |
376.27 ± 320.07 |
418.83 ± 324.59 |
|
|
range (Baths) |
1,500-25,000 |
3,000-30,000 |
4,000-50,000 |
1,000-40,000 |
|
|
(USD) |
43.42-723.59 |
86.83-868.31 |
115.77-1,447.18 |
28.94-1,157.74 |
|
|
Exercise No |
6 (28.60) |
6 (30.00) |
13 (59.10) |
8 (47.10) |
0.135 c |
|
Yes |
15 (71.40) |
14 (70.00) |
9 (40.90) |
9 (52.90) |
|
|
Smoking No |
21 (100.00) |
18 (90.00) |
21 (95.50) |
17 (100.00) |
0.298a |
|
Yes |
- |
2 (10.00) |
1 (4.50) |
- |
|
|
Alcohol No |
21 (100.00) |
17 (85.00) |
22 (100.00) |
17 (100.00) |
- |
|
Yes |
- |
3 (15.00) |
- |
- |
|
|
Comorbidity No |
- |
1 (5.00) |
1 (4.50) |
3 (17.60) |
0.149a |
|
Yes |
21 (100.00) |
19 (95.00) |
21 (95.50) |
14 (82.40) |
|
|
Diabetic duration mean + SD |
10.70 ± 7.40 |
5.30 ± 3.90 |
10.60 ± 3.40 |
8.80 ± 7.60 |
0.013b |
|
range |
2-30 |
1-14 |
5-20 |
1-29 |
|
Note: a = Fisher's Exact Test; b = one-way ANOVA; c = Chi-Square Test
When comparing before and after receiving the intervention program, it was found that older adults in the experimental group had significantly lower HbA1C and WC than before the Program (P < .05, P < .001, respectively). While adults in the experimental group had significantly lesser HbA1C, WC, BMI, and VF than before the Program (P < .05, P < .001, P < .01, P < .05, respectively). Coincidentally, we found that older adults in the control group had significantly lower HbA1C and BMI than before receiving standard care (P < .05) as shown in Table 4.
Table 4. HbA1C and nutritional status in experiment and control groups using paired t-test (N = 80).
|
Items Group |
before |
after |
t |
95% CI |
P-value |
||||||||
|
range |
M ± SD |
range |
M ± SD |
|
|
||||||||
|
HbA1C |
Older adult experimental |
5.60-13.80 |
7.80 ± 1.90 |
5.20-9.00 |
7.00 ±1.10 |
2.43 |
0.121, 1.574 |
.025* |
|||||
|
|
Adult experimental |
6.40-10.70 |
8.10 ± 1.10 |
5.90-7.60 |
7.60 ± 1.10 |
2.51 |
0.084, 0.926 |
.021* |
|||||
|
|
Older adult control |
5.90-10.80 |
8.00 ±1.50 |
5.30-10.00 |
7.30 ± 1.30 |
2.36 |
0.093, 1.470 |
0.028* |
|||||
|
|
Adult control |
6.30-11.90 |
8.90 ± 1.70 |
5.90-11.70 |
8.70 ± 1.70 |
0.37 |
-1.008, 1.432 |
0.718 |
|||||
|
WC |
Older adult experimental |
76.00-114.00 |
89.80 ± 11.00 |
73.00-107.00 |
86.30 ± 10.40 |
6.13 |
2.292, 4.660 |
0.000* |
|||||
|
|
Adult experimental |
79.00-106.00 |
91.30 ± 7.80 |
76.00-102.00 |
86.50 ± 7.80 |
5.98 |
3.135, 6.515 |
0.000* |
|||||
|
|
Older adult control |
75.00-117.00 |
92.20 ± 11.00 |
73.00-110.00 |
91.50 ± 10.00 |
0.93 |
-.0904, 2.359 |
0.364 |
|||||
|
|
Adult control |
68.00-129.00 |
92.50 ± 13.50 |
67.00-126.00 |
91.60 ± 13.90 |
0.89 |
-1.289, 3.171 |
0.384 |
|||||
|
BMI |
Older adult experimental |
20.10-36.20 |
26.30 ± 4.70 |
20.60-35.30 |
26.00 ± 4.60 |
1.85 |
-0.042, 0.699 |
0.079 |
|||||
|
|
Adult experimental |
22.00-35.50 |
27.70 ± 3.60 |
21.80-35.40 |
27.40 ± 3.60 |
3.34 |
.0127, 0.553 |
0.003* |
|||||
|
|
Older adult control |
19.70-41.30 |
28.50 ± 5.30 |
20.20-39.00 |
28.10 ± 4.90 |
2.22 |
0.026, 0.811 |
0.038* |
|||||
|
|
adult control |
15.90-45.80 |
28.90 ± 7.00 |
15.70-45.70 |
28.40 ± 7.10 |
1.16 |
-0.350, 1.197 |
0.263 |
|||||
|
VF |
Older adult experimental |
4.00-28.50 |
11.70 ± 6.40 |
4.5-25.0 |
11.00 ± 5.80 |
2.04 |
-0.013, 1.308 |
0.054 |
|||||
|
|
Adult experimental |
4.00-21.50 |
11.70 ± 5.20 |
4.0-21.5 |
11.50 ± 5.10 |
2.24 |
0.0016, -0.484 |
0.038* |
|||||
|
|
Older adult control |
5.50-30.00 |
14.00 ± 6.30 |
4.0-30.0 |
13.70 ± 6.20 |
0.52 |
-0.743, 1.243 |
0.606 |
|||||
|
|
adult control |
1.00-30.00 |
12.50 ± 7.80 |
0.5-30.0 |
12.00 ± 7.90 |
1.39 |
-0.276, 1.335 |
0.182 |
|||||
|
SM |
Older adult experimental |
18.20-28.80 |
22.60 ± 3.00 |
17.9-29.4 |
22.50 ± 3.10 |
0.45 |
-.0314, 0.485 |
0.659 |
|||||
|
|
Adult experimental |
20.60-30.60 |
24.20 ± 2.90 |
20.0-30.6 |
24.40 ± 3.10 |
-0.63 |
-0.954, 0.514 |
0.538 |
|||||
|
|
Older adult control |
18.90-28.90 |
22.20 ± 3.00 |
17.7-33.7 |
22.50 ± 3.80 |
-0.97 |
-0.915, 0.333 |
0.344 |
|||||
|
|
adult control |
18.80-27.70 |
23.00 ± 2.10 |
19.28.1 |
23.10 ± 2.40 |
-0.63 |
-0.774, 0.421 |
0.540 |
|||||
Note: HbA1C= Hemoglobin A1C; WC = Waist circumference; BMI = Body mass index; VF = Visceral fat; SM = Skeletal muscle; Older adult experimental (n=21); Adult experimental (n =20); Older adult control (n=22); Adult control (n =17); * = Statistical significance (P < .05)
Using one-way ANOVA, we found no significant differences of the baseline outcome variables across four sub-groups (P > .05). Then, we used ANCOVA to control potential confounders from age, marital status, and diabetic duration while examining differences in outcome variables among four sub-groups. There were no significant differences in HbA1C, WC, BMI, VF and SM after receiving the Program between adults and older adults in the experiment groups. Moreover, we found a significant difference in WC (F = 4.76, P < .01) among four sub-groups. Using Post-hoc analysis with LSD, older adults in the experimental group had significantly lower WC than older adults in the control group (P < .01), while adults in the experimental group had significantly lower WC than adults and older adults in the control groups (P < .05) as shown in Table 5 & 6.
Table 5. Comparing HbA1C and nutritional status among adults and older adults with T2DM after receiving the program between experiment and control groups using ANCOVA controlling for age, marital status, and diabetic duration.
|
Source of Variance |
SS |
df |
MS |
F |
P-value |
|
HbA1C |
|||||
|
Groups |
0.897 |
3 |
0.299 |
0.107 |
.956 |
|
Age |
7.682 |
1 |
7.682 |
2.747 |
.102 |
|
Marital Status |
2.757 |
1 |
2.757 |
0.986 |
.324 |
|
Diabetic duration |
1.576 |
1 |
1.576 |
0.564 |
.455 |
|
Groups*Age*Marital Status*Diabetic duration a |
9.141 |
8 |
1.143 |
0.394 |
.920 |
|
Error |
195.767 |
70 |
2.797 |
|
|
|
Total |
241.530 |
80 |
|
|
|
|
WC |
|
|
|
|
|
|
Groups |
185.220 |
3 |
61.740 |
4.760 |
.004* |
|
Age |
0.474 |
1 |
0.474 |
0.037 |
.849 |
|
Marital Status |
11.591 |
1 |
11.591 |
0.894 |
.348 |
|
Diabetic duration |
7.589 |
1 |
7.589 |
0.585 |
.447 |
|
Groups*Age*Marital Status*Diabetic duration a |
21.024 |
8 |
2.628 |
0.186 |
.992 |
|
Error |
907.975 |
70 |
12.971 |
|
|
|
Total |
1714.250 |
80 |
|
|
|
|
BMI |
|
|
|
|
|
|
Groups |
1.370 |
3 |
0.457 |
0.494 |
.688 |
|
Age |
1.026 |
1 |
1.026 |
1.109 |
.296 |
|
Marital Status |
1.957 |
1 |
1.957 |
2.115 |
.150 |
|
Diabetic duration |
0.002 |
1 |
0.002 |
0.002 |
.962 |
|
Groups*Age*Marital Status*Diabetic duration a |
2.639 |
8 |
0.330 |
0.342 |
.946 |
|
Error |
64.759 |
70 |
.925 |
|
|
|
Total |
81.310 |
80 |
|
|
|
|
VF |
|
|
|
|
|
|
Groups |
9.400 |
3 |
3.133 |
1.305 |
.280 |
|
Age |
3.030 |
1 |
3.030 |
1.262 |
.265 |
|
Marital Status |
8.985 |
1 |
8.985 |
3.741 |
.057 |
|
Diabetic duration |
0.932 |
1 |
0.932 |
0.388 |
.535 |
|
Groups*Age*Marital Status*Diabetic duration a |
3.477 |
8 |
0.435 |
0.168 |
.994 |
|
Error |
168.126 |
70 |
2.402 |
|
|
|
Total |
207.710 |
80 |
|
|
|
|
SM |
|
|
|
|
|
|
Groups |
2.018 |
3 |
0.673 |
0.403 |
.751 |
|
Age |
0.068 |
1 |
0.068 |
0.041 |
.841 |
|
Marital Status |
2.579 |
1 |
2.579 |
1.546 |
.218 |
|
Diabetic duration |
4.979 |
1 |
4.979 |
2.985 |
.088 |
|
Groups*Age*Marital Status*Diabetic duration a |
21.008 |
8 |
2.626 |
1.736 |
.107 |
|
Error |
116.747 |
70 |
1.668 |
|
|
|
Total |
241.530 |
80 |
|
|
|
Note: HbA1C= Hemoglobin A1C; WC = Waist circumference; BMI = Body mass index; VF = Visceral fat; SM = Skeletal muscle; Older adult experimental (n=21); Adult experimental (n =20); Older adult control (n=22); Adult control (n =17); * = Statistical significance (P < .05); a =Values by using ANCOVA
Table 6. Comparing waist circumference among adults and older adults with T2DM after receiving the program between experiment and control groups using ANOVA with LSD.
|
Group 1 |
Group 2 |
Mean Difference |
SE |
95%CI |
P-value |
|
Older adult experimental |
Adult experimental |
1.304 |
1.755 |
-4.805, 2.196 |
.460 |
|
Older adult experimental |
Adult control |
-2.306 |
1.823 |
-5.943, 1.331 |
.210 |
|
Older adult experimental |
Older adult control |
-3.209* |
1.140 |
-5.483, -0.935 |
.006* |
|
Adult experimental |
Older adult control |
-4.513* |
1.763 |
-8.028, -0.998 |
.013* |
|
Adult experimental |
Adult control |
-3.610* |
1.522 |
-6.647, -0.574 |
.020* |
Note: Older adult ASE (n=21); Adult ASE (n =20); Older adult control (n=22); Adult control (n =17); * = Statistical significance (p < .05)
DISCUSSION
This study revealed that the 12-week ASE Program for 30 minutes/day, 5 days/week, which based on the PNI (Pahlevi et al., 2017) and Self-efficacy Theory of Bandura (1977) was effective in only reduction of WC. There were no significant differences in reduction of HbA1C, WC, BMI, VF, and increase SM between the adults and older adults in the experimental group. This might be that both experimental age groups had their mean age approximately 60 years old. Increasing age (more than 50 years) may result in an increase in abdominal fat and a decrease in strength and muscle mass (Putri et al., 2020; Mahmudiono et al., 2021; Mekić et al., 2021).An increased abdominal fat results in a risk of insulin insensitivity and increased insulin resistance leading to reduced ability of glucose uptake in skeletal muscle (Kleebbua et al., 2018; Prasertsri and Leelayuwat, 2019; Putri et al., 2020; Mahmudiono et al., 2021; Mekić et al., 2021). Unfortunately, HbA1C, WC, BMI, VF, and SM were not significantly different between the two experimental age groups. This ASE might be not enough to improve outcome variables though the ASE assists to increase fat oxidation bringing to a decrease in total fat mass and increase in SM (Yang et al., 2019; Putri et al., 2020; Ooi et al., 2021). These findings were different from previous studies confirming the effectiveness of lower HbA1C (Khamsom et al., 2017; Ooi et al., 2021), WC (Khamsom et al., 2017; Kleebbua et al., 2018), and BMI (Kleebbua et al., 2018). However, HbA1C (Mahmudiono et al., 2021) and BMI (Khamsom et al., 2017) outcomes were similar to some studies. Hence, participants should maintain a regular schedule of the ASE with walking since ASE is mild to moderate intensity of the exercise (Kleebbua et al., 2018; Phonyiam et al., 2019; Prasertsri et al., 2019; Prasertsri and Leelayuwat, 2019; Terathongkum et al., 2021) and that might be not enough for increasing calorie uptake and skeletal muscle in people nearly or above 60 years old. The systematic review showed that the duration for PA interventions is at least 16 weeks, lasting 60–90 minutes for healthy life style improvement (Suriyawong & Pipatpiboon, 2022).
Furthermore, this ASE Program resulted in only WC reduction in the experimental groups. There were no significant differences in HbA1C, BMI, VF, and SM between the experimental and the control groups. Older adults in the experimental group had significantly lower WC than older adults in the control group. Adults in the experimental group also had significantly lower WC than adults and older adults in the control groups at week 13 of the study. This might be explained by the fact that ASE helps increase fat oxidation bringing to decrease in total fat mass in the experimental groups (Ooi et al., 2021; Putri et al., 2020; Yang et al., 2019). Besides, four groups received the standard care being the effective methods to control blood glucose and other outcomes. The Seven-Color Life Traffic Ping-Pong divides people based on their blood glucose level and its severity to receive treatment either lifestyle modification (food control, exercise, and emotion) or taking medications or both (Table 2). It also gives 100 scores to evaluate their performance. The more score, the better control (Teintavorn, 2019) resulting improvement of participants’ behaviors and blood glucose control (Juwa, et al., 2019). Thus, adults and older adults in the experimental groups and the control groups had better outcomes resulting in no significant difference among the four groups. This comparison between groups was similar to some studies (Phonyiam et al., 2019; Kirwan et al., 2021; Terathongkum et al., 2021), but was different from other studies (Wanna et al., 2018; Zheng et al., 2020; Mahmudiono et al., 2021; Ooi et al., 2021; Terathongkum et al., 2021). Thus, integration the ASE Program and the standard care should improve these outcome variables.
In addition, a small sample size, especially in the adult control group, is a limitation of this study that may threaten external validity and low power of the statistic test. To prevent dropouts for future studies, we suggest adding more activities in the control group to inspire them to engage in the study. Moreover, our study reassures people with T2DM to practice continuously mild to moderate intensity exercise especially the ASE with walking approximately 30 minutes a day, 5 days a week, or 150 minutes a week for superior health outcomes and complication prevention. Finally, this study did not examine intra-rater or inter-rater reliability related to outcome measurement by the RAs. This may cause measurement bias. Future research needs to control these biases in planning the study design including an adequate sample size and validating outcome variable. The next study will verify the importance of home-based exercise for people with T2DM in achieving glycemic regulation and improving nutritional status, and may include other sensitive outcome variables to ASE such as mobility, back pain, posture stability and feeling relax.
CONCLUSION
The 12- week Arm Swing Exercise Program 30 minutes/day, 5 days/week has no effect on regulating blood glucose, but has effect on reduction of waist circumference in people with T2DM, and the effects of all target variables between both adults and older adults were the same. Thus, this exercise should simply practice at home to reduce WC, but need to integrate with standard care.
ACKNOWLEDGMENTS
Thanks for the grant from the Ramathibodi School of Nursing, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Thailand. The authors are also appreciated all participants in this study.
REFERENCES
American Diabetes Association Professional Practice Committee. 2022. Prevention or delay of type 2 diabetes and associated comorbidities: Standards of medical care in diabetes-2022; [accessed 2023 Jan 1].
Bandura, A. 1977. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 84(2): 191-215.
Chia, C.W., Egan, J.M., and Ferrucci, L. 2018. Age-related changes in glucose metabolism, hyperglycemia, and cardiovascular risk. Circulation Research. 123: 886-904.
Des Jarlais, D.C., Lyles, C., and Crepaz, N. 2004. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. American Journal of Public Health. 94(3): 361-366.
Juwa, S., Wongwat, R., and Manoton, A. 2019. The effectiveness of the health behavior change program with 7 colors ball tool on knowledge, health belief and behavior related to the prevention and control of hypertension and diabetes mellitus in Maeka sub-district Muang district Phayao province. Songklanagarind Journal of Nursing. 39(2): 127-141.
Khamsom, S., Terathongkum, S., and Kittipimpanon, K. 2017. Effects of arm swing exercise program on HbA1C and nutritional status in community dwelling older adults with type 2 diabetes. Thai Journal of Nursing and Midwifery Practice. 4(2): 46-60.
Kirwan, M., Chiu, C.L., Hay, M., and Laing, T. 2021. Community-based exercise and lifestyle program improves health outcomes in older adults with type 2 diabetes. International Journal of Environmental Research and Public Health. 18: 6147.
Kleebbua, K., Piaseu, N., Neelapaichit, N., and Tantiprasoplap, S. 2018. Effects of arm swing exercise programme on nutritional status in female older adults at risk of metabolic syndrome. The Journal of Thailand Nursing and Midwifery Council. 33(1): 27-37.
Liangruenrom, N., Suttikasem, K., Craike, M., Bennie, J.A., Biddle, S.J.H., and Pedisic, Z. 2018. Physical activity and sedentary behaviour research in Thailand: a systematic scoping review. BMC Public Health. 18: 1-24.
Lin, Y., Chen, Y., Tseng, Y., Tsai, S., and Tseng, Y. 2020. Physical activity and successful aging among middle-aged and older adults: a systematic review and meta-analysis of cohort studies. Aging. 12(9): 7704-7016.
Mahmudiono, T., Setyaningtyas, S.W., Rachmah, Q., Nindya, T.S., Megatsari, H., Indriani, D., Rifqi, M.A., and Kriengsinyos, W. 2021. Self-efficacy in physical activity and glycemic control among older adults with diabetes in Jagir Subdistrict, Surabaya, Indonesia. Heliyon. 7: e07578.
Manickum, P., Madiba, T., and Ramklass, S. 2022. The effectiveness of diabetic foot-care education in a South African regional hospital: A randomised controlled trial. Journal of Endocrinology, Metabolism and Diabetes of South Africa. 27(1): 20-31.
Mekić, R., Mekić, M., Dolićanin, Z., Mavrić, A., Čaprić, I., Biševac, E., and Zećirović, A. 2021. Influence of exercise program content on elderly persons with diabetes mellitus tip 2. SportLogia. 17(1): 25- 33.
Ooi, T.C., Ludin, A.F.M., Loke, S.C., Singh, M.A.F., Wong, T.W., Vytialingam, N., Abdullah, M.M.J.A., Ng, O.C., Bahar, N., Zainudin, N., et al. 2021. A 16-Week home-based progressive resistance tube training among older adults with type-2 diabetes mellitus: Effect on glycemic control. Gerontology and Geriatric Medicine. 7: 23337214211038789.
Pahlevi, R., Putra, S.T., and Sriyono. 2017. Psikoneuroimunology approach to improve recovery motivation, decrease cortisol and blood glucose of DM type 2 patients with dhikr therapy. Ners Journal. 2(1): 60-65.
Phonyiam, R., Terathongkum, S., and Lininger, J. 2019. Effects of arm swing exercise program on blood sugar level, nutritional status and perceived self-efficacy for exercise in persons with uncontrolled type 2 diabetes mellitus. Bangkok Medical Journal 14(2): 34-39.
Prasertsri, P. and Leelayuwat, N. 2019. Effects of arm swing exercise training on cardiac autonomic functions in response to incremental exercise in overweight and normal weight young adults. Journal of the Medical Association of Thailand. 102(1): 1-9.
Prasertsri, P., Singsanan, S., Chonanant, C., Boonla, O., and Trongtosak, P. 2019. Effects of arm swing exercise training on cardiac autonomic modulation, cardiovascular risk factors, and electrolytes in persons aged 60-80 years with prehypertension: A randomized controlled trial. Journal of Exercise Science and Fitness. 17(2): 47-54.
Putri, S.T., Rahmi, U., Sumartini, S., Fitriana, L.A., and Salasa, S. 2020. Physical exercises for the elderly with diabetes mellitus type 2. Advances in Health Sciences Research. 21: 299-302.
Saelao, K. 2012. Effects of arm swing exercise and walking on health-related physical fitness of the elderly women. Journal Sports Science and Health. 13(1): 92-103.
Sitkulanan P, Kumtip P. 2020. Impact of a self-management programme monitored through the application line on eating behaviour, arm-swing exercise behaviour, and blood glucose levels in women with gestational diabetes mellitus. Journal of Thailand Nursing and Midwifery Council. 35(2): 52–69.
Suriyawong W. and Pipatpiboon, N. 2022. Social cognitive theory-based interventions on healthy lifestyles for hypertensive patients: a systematic review. Chiang Mai University Journal of Natural Sciences. 21(3): e2022040.
Teintavorn, V. 2013. Surveillance system, control and prevention of diabetes, hypertension in Thailand: Policy to practice. 3rd ed. Bangkok: Agricultural Cooperative Federation of Thailand Limited. [accessed 2023 Jan 1]. https://kpo.go.th/webkpo/tool/NCD_Policy2Action.pdf.
Terathongkum, S., Phonyiam, R., and Koonmee P. 2021. Effects of traditional and modified arm swing exercise programs on blood glucose and nutritional status among persons with type 2 diabetes: A secondary data analysis. Pacific Rim International Journal of Nursing Research. 25(3): 452-465.
Wanna, J., Terathongkum, S., and Thipsuwannakool, V. 2018. Effects of arm swing exercise program on HbA1C and nutritional status in adults with type 2 diabetes in community. Bangkok Medical Journal. 14(1): 23-8.
World Heath Organization. 2020. At a glance: WHO guidelines on physical activity and sedentary behavior. [accessed 2023 Jan 1]. https://www.who.int/publications/i/item/9789240014886.
Yang, D., Yang, Y., Li, Y., and Han, R. 2019. Physical exercise as therapy for type 2 diabetes mellitus: From mechanism to orientation. Annals of Nutrition and Metabolism.74: 313-321.
Zheng, X., Qi, Y., Bi, L., Shi, W., Zhang, Y., Zhao, D., Hu, S., Li, M., and Li, Q. 2020. Effects of exercise on blood glucose and glycemic variability in type 2 diabetic patients with dawn phenomenon. BioMed Research International. 2020: 6408724.
OPEN access freely available online
Natural and Life Sciences Communications
Chiang Mai University, Thailand. https://cmuj.cmu.ac.th
Sangthong Terathongkum and Kamonrat Kittipimpanon*
Ramathibodi School of Nursing, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok 10400, Thailand.
Corresponding author: Kamonrat Kittipimpanon E-mail: kamonrat.kit@mahidol.ac.th
Total Article Views
Editor: Sirasit Srinuanpan,
Chiang Mai University, Thailand
Article history:
Received: February 20, 2023;
Revised: June 2, 2023;
Accepted: June 7, 2023;
Published online: June 14, 2023

